Abstract
Objective
Systematic understanding of patients’ unmet needs is essential for providing effective supportive care. This study sought to compare the unmet needs of patients with cancer identified by health care providers (HCPs) among four major healthcare systems.
Methods
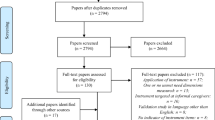
HCPs (n = 247) participated in the International Psycho-Oncology Society (IPOS) Survivorship Online Survey, evaluating their patients’ unmet needs. The country of HCPs was grouped into four major healthcare systems: Beveridge model, Bismarck model, National Health Insurance model, and out-of-pocket model.
Results
Most HCPs were from countries with the Bismarck model. Substantial levels (> 50%) of unmet needs in all domains are reported across the four healthcare systems. Pediatric patients/survivors living in countries under out-of-pocket healthcare model were evaluated to have less unmet needs for managing decline in physical or cognitive functioning and insomnia/sleep difficulty/fatigue, than those in countries under Beveridge, Bismarck, and National Health Insurance models. Moreover, middle-aged patients/survivors under Beveridge and National Health Insurance models were likely to have greater unmet needs for dealing with cancer-related financial concerns than those under Bismarck model.
Conclusion
This study provides valuable insights into the unmet needs of patients with cancer in different healthcare systems, highlighting the significance of targeted interventions to address the unique needs of patients across diverse healthcare systems. Further investigation is warranted to identify the system factors associated with patients’ unmet needs, enabling the development of effective healthcare policies and interventions to comprehensively address the multifaceted needs of patients with cancer.


Similar content being viewed by others
Data availability
The data that support the findings of the paper are available from the corresponding author upon reasonable request.
References
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clin 73(1):17–48
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
International Agency for Research on Cancer. World Health Organization. Press Release Nº 292. Latest global cancer data: cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. Lion, France. Available at: https://www.iarc.who.int/wp-content/uploads/2020/12/pr292_E.pdf. Accessed 24 Feb 2023
Carlson LE, Angen M, Cullum J et al (2004) High levels of untreated distress and fatigue in cancer patients. Br J Cancer 90(12):2297–2304
Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psychooncology 10(1):19–28
Serpentini S, Tessarin S, Capovilla E (2015) La cura psicosociale in oncologia. Nuovi standard e linee guida. Teramo: Artemia
National Breast Cancer Centre and National Cancer Control Initiative (2003) Clinical practice guidelines for the psychosocial care of adults with cancer. Available at http://www.nhmrc.gov.au/publications/synopses/cp90synhtm. Accessed 24 Feb 2023
Carey M, Lambert S, Smits R, Paul C, Sanson-Fisher R, Clinton-McHarg T (2012) The unfulfilled promise: a systematic review of interventions to reduce the unmet supportive care needs of cancer patients. Support Care Cancer 20(2):207–219
Foot G, Sanson-Fisher R (1995) Measuring the unmet needs of people living with cancer. Cancer Forum 19(2):131–135
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P (2000) The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 88(1):226–237
Gysels M, Higginson I, Rajasekaran M, Davies E, Harding R (2004) Improving supportive and palliative care for adults with cancer: research evidence. National Institute for Health and Clinical Excellence, London
de Heus E, van der Zwan JM, Husson O, Frissen AR, van Herpen CML, Merkx MAW, Duijts SFA (2021) Unmet supportive care needs of patients with rare cancer: a systematic review. Eur J Cancer Care 30(6):e13502
Carr W, Wolfe S (1976) Unmet needs as sociomedical indicators. Int J Health Serv 6(3):417–430
Pappa E, Kontodimopoulos N, Papadopoulos A, Tountas Y, Niakas D (2013) Investigating unmet health needs in primary health care services in a representative sample of the Greek population. Int J Envir Res Public Health 10(5):2017–2027
Chen J, Hou F (2002) Unmet needs for health care. Health Rep 13(2):23–34
Sibley LM, Glazier RH (2009) Reasons for self-reported unmet healthcare needs in Canada: a population-based provincial comparison. Healthc Pol 5(1):87–101
Kim YS, Lee J, Moon Y, Kim KJ, Lee K, Choi J, Han SH (2018) Unmet healthcare needs of elderly people in Korea. BMC Geriatr 18(1):98
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P (2000) The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 88(1):226–237
Bergerot CD, Mitchell HR, Ashing KT, Kim Y (2017) A prospective study of changes in anxiety, depression, and problems in living during chemotherapy treatments: effects of age and gender. Support Care Cancer 25(6):1897–1904
Hodgkinson K, Butow P, Hunt GE et al (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology 16(9):796–804
World Health Organization (2000) The World Health Report 2000 - Health systems: improving performance. World Health Organization, Geneva
Kim Y, Ting A, Carver CS et al (2023) International collaboration for assessing unmet needs of cancer survivors and family caregivers: lens of healthcare professionals. Psychooncology 32(1):77–85
Capture RED. Available at: https://projectredcap.org/software/. Accessed 24 Feb 2023
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P (2000) The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 88(1):226–237
Bergerot CD, Wang AW, Dégi LC, Bahcivan O, Kim Y (2023) Cancer patients’ unmet needs in three low- to middle- income countries: perspectives from health care providers. Cancer Invest 16:1–8
Razavi M, Bergerot CD, Clark KL et al (2022) Association between requests for supportive care assistance and patients’ characteristics, prior to treatment in a comprehensive cancer center. Psychooncology 31(8):1347–1353
Deshields TL, Wells-Di Gregorio S, Flowers SR, Irwin KE, Nipp R, Padgett L, Zebrack B (2021) Addressing distress management challenges: recommendations from the consensus panel of the American Psychosocial Oncology Society and the Association of Oncology Social Work. CA Cancer J Clin 71(5):407–436
Smith SK, Loscalzo M, Mayer C, Rosenstein DL (2018) Best practices in oncology distress management: beyond the screen. Am Soc Clin Oncol Educ Book 38:813–821
Ranabhat CL, Atkinson J, Park MB, Kim CB, Jakovljevic M (2018) The influence of universal health coverage on life expectancy at birth (LEAB) and healthy life expectancy (HALE): a multi-country cross-sectional study. Front Pharmacol 9:960
Kong YC, Wong LP, Ng CW et al (2020) Understanding the financial needs following diagnosis of breast cancer in a setting with universal health coverage. Oncologist 25(6):497–504
Gordon LG, Merollini KMD, Lowe A, Chan RJ (2017) A systematic review of financial toxicity among cancer survivors: we can’t pay the co-pay. Patient 10(3):295–309
Büttner M, König HH, Löbner M, Briest S, Konnopka A, Dietz A, Riedel-Heller S, Singer S (2019) Out-of-pocket-payments and the financial burden of 502 cancer patients of working age in Germany: results from a longitudinal study. Support Care Cancer 27(6):2221–2228
Bhoo-Pathy N, Ng CW, Lim GC et al (2019) Financial toxicity after cancer in a setting with universal health coverage: a call for urgent action. J Oncol Pract 15(6):e537–e546
Funding
The writing of this manuscript was supported by the National Institute of Nursing Research (R01NR016838) to YK.
Author information
Authors and Affiliations
Contributions
CDB, AWTW, SS, CB, YK: conception and design. CDB, AWTW, SS, CB, YK: drafting the manuscript review of the literature. CDB, AWTW, SS, CB, YK: critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The survey content and procedure were reviewed and approved by the Institutional Review Board of the University of Miami, FL, USA and the IPOS research committee. This is not a human subject research and informed consent was not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bergerot, C.D., Wang, A.WT., Serpentini, S. et al. Healthcare providers’ perceptions about the unmet needs of their patients with cancer across healthcare systems: results of the International Psycho-Oncology Society survivorship survey. Support Care Cancer 31, 538 (2023). https://doi.org/10.1007/s00520-023-07998-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07998-8