Abstract
Purpose
Routinely assessing quality of life (QoL) of patients with cancer is crucial for improving patient-centred cancer care. However, little is known about whether or how cancer centres assess QoL for clinical practice or for research purposes. Therefore, our study aimed to investigate if QoL data is collected and if so, how and for what purposes.
Method
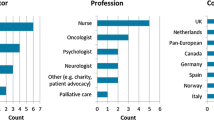
We conducted a cross-sectional survey study among 32 cancer centres in Europe and Canada. Centre representatives identified persons who they judged to have sufficient insight into QoL data collections in their wards to complete the survey. Descriptive statistics were used to summarise the information on QoL assessment and documentation.
Results
There were 20 (62.5%) responding cancer centres. In total, 30 questionnaires were completed, of which 13 were completed for cancer wards and 17 for palliative care wards. We found that 23.1% and 38.5% of the cancer wards routinely assessed QoL among inpatients and outpatients with cancer, respectively, whereas, in palliative care wards, 52.9% assessed QoL for outpatients with cancer and 70.6% for the inpatients. Wide variabilities were observed between the cancer centres in how, how often, when and which instruments they used to assess QoL.
Conclusion
A sizable proportion of the cancer wards, especially, and palliative care wards apparently does not routinely assess patients’ QoL, and we found wide variabilities between the cancer centres in how they do it. To promote routine assessment of patients’ QoL, we proposed several actions, such as addressing barriers to implementing patient-reported outcome measures through innovative e-health platforms.
Similar content being viewed by others
Data availability
Not applicable.
References
World Health Organization (2020) WHO report on cancer: setting priorities, investing wisely and providing care for all. Available from: https://www.who.int/publications/i/item/9789240001299. Accessed 16 Nov 2022
Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ (2009) What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer 17:1117–1128. https://doi.org/10.1007/s00520-009-0615-5
Hart NH, Crawford-Williams F, Crichton M, Yee J, Smith TJ, Koczwara B et al (2022) Unmet supportive care needs of people with advanced cancer and their caregivers: a systematic scoping review. Crit Rev Oncol/Hematol 176:103728. https://doi.org/10.1016/j.critrevonc.2022.103728
Miller BE, Pittman B, Strong C (2003) Gynecologic cancer patients’ psychosocial needs and their views on the physician’s role in meeting those needs. Int J Gynecol Cancer 13:111–119. https://doi.org/10.1136/ijgc-00009577-200303000-00002
Murray SA, Kendall M, Boyd K, Worth A, Benton TF (2004) Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliat Med 18:39–45. https://doi.org/10.1191/0269216304pm837oa
Beernaert K, Pardon K, Van den Block L, Devroey D, De Laat M, Geboes K et al (2016) Palliative care needs at different phases in the illness trajectory: a survey study in patients with cancer. Eur J Cancer Care 25:534–543. https://doi.org/10.1111/ecc.12522
Kaasa S, Loge JH, Aapro M, Albreht T, Anderson R, Bruera E et al (2018) Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol 19:e588–e653. https://doi.org/10.1016/S1470-2045(18)30415-7
Chen J, Ou L, Hollis SJ (2013) A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res 13:211. https://doi.org/10.1007/s001090000086
Kotronoulas G, Kearney N, Maguire R, Harrow A, Di Domenico D, Croy S et al (2014) What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol 32:1480–1510. https://doi.org/10.1200/jco.2013.53.5948
Yang LY, Manhas DS, Howard AF, Olson RA (2018) Patient-reported outcome use in oncology: a systematic review of the impact on patient-clinician communication. Support Care Cancer 26:41–60. https://doi.org/10.1007/s00520-017-3865-7
Bennett AV, Jensen RE, Basch E (2012) Electronic patient-reported outcome systems in oncology clinical practice. CA-Cancer J Clin 62:336–347. https://doi.org/10.3322/caac.21150
Howell D, Molloy S, Wilkinson K, Green E, Orchard K, Wang K et al (2015) Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol 26:1846–1858. https://doi.org/10.1093/annonc/mdv181
Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P et al (2016) Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol 34:557. https://doi.org/10.1200/jco.2015.63.0830
Hansson E, Carlström E, Olsson L-E, Nyman J, Koinberg I (2017) Can a person-centred-care intervention improve health-related quality of life in patients with head and neck cancer? A randomized, controlled study. BMC Nurs 16:1–12. https://doi.org/10.1186/s12912-017-0206-6
Black N (2013) Patient reported outcome measures could help transform healthcare. BMJ 346:f167. https://doi.org/10.1136/bmj.f167
Lipscomb J, Donaldson MS, Hiatt RA (2004) Cancer outcomes research and the arenas of application. J Natl Cancer Inst Monogr 2004:1–7. https://doi.org/10.1093/jncimonographs/lgh038
Zhang B, Lloyd W, Jahanzeb M, Hassett MJ (2018) Use of patient-reported outcome measures in quality oncology practice initiative–registered practices: results of a national survey. J Oncol Pract 14:e602–e611. https://doi.org/10.1200/jop.18.00088
Anatchkova M, Donelson SM, Skalicky AM, McHorney CA, Jagun D, Whiteley J (2018) Exploring the implementation of patient-reported outcome measures in cancer care: need for more real-world evidence results in the peer reviewed literature. J Patient-Rep Outcomes 2:1–21. https://doi.org/10.1186/s41687-018-0091-0
Oslo University Hospital. About European Palliative Care Research Centre [updated 22 Oct 2021. Internet]. Available from: https://oslo-universitetssykehus.no/avdelinger/kreftklinikken/avdeling-for-kreftbehandling/about-prc
Oslo University Hospital. PRC collaborating centres [updated 24 Nov 2021. Internet]. Available from: https://oslo-universitetssykehus.no/avdelinger/kreftklinikken/avdeling-for-kreftbehandling/collaborating-centres-1
Nguyen H, Butow P, Dhillon H, Sundaresan P (2021) A review of the barriers to using patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) in routine cancer care. J Med Radiat Sci 68:186–195. https://doi.org/10.1002/jmrs.421
Nguyen H, Butow P, Dhillon H, Morris L, Brown A, West K et al (2020) Using patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) in routine head and neck cancer care: what do health professionals perceive as barriers and facilitators? J Med Imag Radiat Oncol 64:704–710. https://doi.org/10.1111/1754-9485.13048
van Egdom LS, Oemrawsingh A, Verweij LM, Lingsma HF, Koppert LB, Verhoef C et al (2019) Implementing patient-reported outcome measures in clinical breast cancer care: a systematic review. Value Health 22:1197–1226. https://doi.org/10.1016/j.jval.2019.04.1927
Cresswell K, Williams R, Sheikh A (2020) Developing and applying a formative evaluation framework for health information technology implementations: qualitative investigation. J Med Internet Res 22:e15068. https://doi.org/10.2196/15068
Roberts NA, Janda M, Stover AM, Alexander KE, Wyld D, Mudge A (2021) The utility of the implementation science framework “Integrated Promoting Action on Research Implementation in Health Services” (i-PARIHS) and the facilitator role for introducing patient-reported outcome measures (PROMs) in a medical oncology outpatient department. Qual Life Res 30:3063–3071. https://doi.org/10.1007/s11136-020-02669-1
Why and what [internet]. Available from: https://mypath-cancercare.eu/elementor-139/why-and-what/. Accessed 16 Nov 2022
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. RM acquired the data and conducted the data analyses, which were then checked by KB. RM, ER and KB drafted and revised the manuscript critically for important intellectual content. All authors made substantial contribution to interpreting the data and revising the manuscript critically; have given the final approval of the manuscript to be submitted for publication; and have participated sufficiently in the work to take responsibility for appropriate portions of the content.
Corresponding author
Ethics declarations
Ethical approval
This research was approved by the Medical Ethical Committee of the University Hospital Brussels (BUN: 1432021000536) and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and subsequent amendments.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All study participants agreed to the use of their data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miranda, R., Raemdonck, E., Deliens, L. et al. Do cancer centres and palliative care wards routinely measure patients’ quality of life? An international cross-sectional survey study. Support Care Cancer 31, 499 (2023). https://doi.org/10.1007/s00520-023-07964-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07964-4