Abstract
Purpose
This study examined the effects of Fil-Rouge Integrated Psycho-Oncological Support (FRIPOS) in a group of women with breast cancer compared with a group receiving treatment as usual (TAU).
Methods
The research design was a randomized, monocentric, prospective study with three time points of data collection: after the preoperative phase (T0), in the initial phase of treatments (T1), and 3 months after the start of treatments (T2). The FRIPOS group (N = 103) and the TAU group (N = 79) completed a sociodemographic questionnaire, the Symptom Checklist-90-R (SCL-90-R) at T0; the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ) C30 and EORTC QLQ-BR23 at T1; and SCL-90-R, EORTC QLQ-C30, and EORTC QLQ-BR23 at T2.
Results
A series of independent and paired t tests showed that patients in the FRIPOS group performed better on all scales related to symptomatic manifestations and on some quality of life scales (fatigue, dyspnea, and sleep disturbances) at T2. In addition, a series of ten multiple regressions were performed to predict each SCL subscale at T2 from the SCL score at T0 and the EORTC QLQ-C30 scores at T2. In nine of ten regression models (all except somatization), both FRIPOS group membership and QoL subscale contributed significantly to prediction.
Conclusions
This study suggests that patients in the FRIPOS group have more benefits in emotional, psychological, and collateral symptoms than patients in the TAU group and that these improvements are due to integrated psycho-oncology care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most commonly diagnosed cancer in Italian women [1]. In 2021, 834,200 women in Italy were living with a breast cancer diagnosis. Although the mortality rate has decreased thanks to early diagnosis and medical advances in the care of women with this disease, and the 5-year survival rate is 87% [2], it is necessary to deepen the topic of psychological adaptation to the disease, which inevitably brings changes in the different areas of a woman’s life [3].
The psycho-oncological support
Psycho-oncology is a branch of the oncology disciplines that is particularly concerned with two psychological dimensions: the psychological responses of patients and their families to all phases of disease and staff stress and the psychological, social, and behavioral factors that influence cancer onset and disease survival [4]. Psychological support for cancer patients is now recognized as a fundamental aspect of treatment pathways [5], but interventions are often highly targeted and delivered separately from the medical context; examples include cognitive behavioral therapy [6,7,8], mindfulness and relaxation techniques [9], psychoeducation [10], and family and couples therapy [11]. However, there are few operational models describing how psycho-oncological support interacts with medical staff in acute care, especially in the Italian context [12], and furthermore, there are still many barriers that prevent cancer patients from seeking support.
Barriers to seeking psychological support in cancer patients
The communication gap between the patient and the medical staff is one of the main problems [13]. In addition, according to the literature, cancer patients often have several unmet needs, with psychological and information problems being the most common [14, 15]. Finally, many patients are not fully aware of their emotional, cognitive, and psychological vulnerability. This may be a temporary condition due to the traumatic effects of the disease, which can lead to a pathological state of numbness [16], or in other cases due to their previous cognitive or emotional functioning [17, 18]. Other common problems are that patients are not adequately informed about support services [19], that they may be perceived as stigmatizing [20], and that medical staff may not be adequately informed about the role of psychosocial care [21].
Psycho-oncology as an integrated support in routine multidisciplinary cancer care
Whereas in the past, support was usually provided only at the patient’s request, today, the modality has evolved to the so-called tiered models (or stepped models) based on monitoring of suffering [22, 23]. For example, in the UK, the National for Health and Care Excellence (NICE) [24] has developed a psychological intervention pathway with a four-stage paradigm that targets psychological problems or needs through screening and provides treatment as needed.
This approach remains the most widely used and proven, including cost-effectiveness [25], but it has several limitations. First, because the causes of suffering are complex, focusing exclusively on psychological problems risks overlooking the patient’s other perceived needs [14]. In addition, research has shown that most patients who have a high distress screening score with a specific assessment tool do not want to be referred to psychological counseling, whereas patients with a low distress score often hope for some form of support [26, 27]. Finally, some research suggests that an accurate diagnosis of distress is not necessarily linearly related to the ability of health care professionals to control and effectively treat the symptoms that are the cause of distress [28].
An organized method of care that ensures that all of the patient’s needs are met in a coherent and seamless manner is referred to as an “integrated system of care.” Proposals have emerged around the world in the last decade, and although development is ongoing, studies appear promising. These procedures are integrated into clinical routines and address all patients, at least in the initial phase [29, 30].
The FRIPOS project
The Fil-Rouge Integrated Psycho-Oncological Support (FRIPOS) project is in line with the agreement of April 17, 2019, between the Italian State and its Regions, and the European Cancer Plan presented in February 2021 [31], even if it was designed following the Italian National Cancer Plan of 2016. In it, an integrated supportive intervention based on a close synergy between psycho-oncologists, medical, and nursing staff is proposed [32, 33].
The aim of this study was to evaluate the impact of the FRIPOS model compared with routine care in a sample of women with breast cancer.
Clinical steps and research procedure
As shown in Table 1, which illustrates the clinical and research steps during the project, the psycho-oncologist was present in the FRIPOS group at various times during cancer treatment.
The overall clinical goals of the intervention were identified by consulting the clinical scientific literature and can be summarized as follows: (A) encouraging the patient to adapt to the new condition by helping her cope with the physical, psychological, social, and relational changes caused by the disease [34]; (B) deepening the problem areas by identifying the patient’s needs in order to provide integrated and personalized therapeutic interventions [35, 36]; (C) facilitating emotional expression by encouraging the patient to recognize and control anxious and/or depressive states [37]; (D) paying attention to body image to facilitate the process of accepting therapies [38, 39]; (E) communicating the patient’s needs to the treatment team to jointly develop a rehabilitation project for each individual patient [40].
We hypothesized that women who received integrated support would have lower scores for psychopathological symptoms, better psychological and emotional functioning, and better quality of life parameters than the group that received treatment as usual (TAU).
Ethics and research design
The intervention and the filling in of the questionnaires took place during the hospitalization in the surgical department and during the visit to the oncological day hospital and/or to the “Alte Energie” Center of the Oncological Radiotherapy Department of the Clinical Institute of S. Anna in Brescia — San Donato Group. The project was approved by the Ethics Committee of the Clinical Institute of S. Anna in Brescia (Prot. Number: 2016.1.1; June 6, 2016).
The questionnaires were labeled with an alphanumeric code, the combination of which was known only to the nursing staff responsible for randomization. The medical staff and the researchers who performed the data analysis were blinded to this information.
The research design was a randomized, prospective study with triple data collection according to the steps of the clinical intervention: preoperative phase (T0), initial phase of treatments (T1), and 3 months after the start of treatments (T2) (Table 1).
In the pre-study phase, nurses informed patients of the opportunity to participate in the research project, obtained informed consent, and performed randomization using the online software Research Randomizer (version 4.0). The Symptom Checklist-90-R (SCL-90-R) was used only at T0 and T2 because it was considered a specific and primary tool for evaluating the FRIPOS program by assessing symptom indices at baseline and at the end of the project. At T1 and T2, patients completed two quality of life (QLQ) questionnaires developed by the European Organization for Research and Treatment of Cancer (EORTC), namely C-30 and BR-23.
Measures
The instruments used are all standardized and validated in the Italian context.
Symptom Checklist-90-R
The SCL-90-R [41, 42] is a self-administered questionnaire for the assessment of psychological stress and psychopathological symptoms. It consists of 90 items measuring both a Global Severity Index, a global indicator of the intensity of psychological distress complained of by the respondent, and nine primary symptom dimensions: somatization (SOM), obsessions (O-C), interpersonal sensitivity (I-S), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR), and psychoticism (PSY).
Subjects’ responses ranged from 0 (not at all) to 4 (very strongly). Cronbach’s α was measured on item scores at the two induction time points, with α at T0 = 0.96 and α at T2 = 0.98.
EORTC QLQ-C30 and EORTC QLQ-BR23
The EORTC QLQ-C30 [43] is an instrument for measuring quality of life in cancer patients. In addition to the general quality of life (QoL) assessment, this questionnaire includes the following: five function scales — physical (PF), role (RF), cognitive (CF), emotional (EF), and social (SF) functions; three symptom-related scales — fatigue (FA), nausea and vomiting (NV), and pain (PA); and six individual items on loss of appetite (AP), dyspnea (DY), sleep disturbances (SD), constipation (CO), diarrhea (DI), and financial difficulties (FD). The test includes 30 items with a response range of 1 (none) to 4 (very severe). The QLQ-BR23 is a questionnaire designed to assess the specific problems of breast cancer patients. This particular module includes 23 questions assessing body image (BRBI), sexual functioning (BRSEF), sexual experience (BRSEE), future prospects (BRFU), side effects of systemic therapy (BRST), breast symptoms (BRBS), arm symptoms (BRAS), and hair loss (BRHL). Responses ranged from 1 (none) to 4 (very severe). Cronbach’s α of the QLQ-C30 at T1 = 0.80 and T2 = 0.85, whereas the α of the QLQ-BR23 at T1 = 0.71 and T2 = 0.78.
Statistical analyses
Statistical analyses were performed using Statistical Package for the Social Sciences software (SPSS, version 26). A total of 124 subjects (69.67%) answered the entire questionnaire without omissions. Subscales with two or more missing values were not included in the calculation. This procedure resulted in 177 complete questionnaires (98.2%).
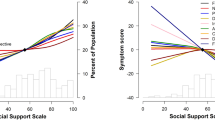
To compare the two groups (FRIPOS group and TAU group) analyzed at the same time of administration, multiple independent-samples t tests were performed to determine whether there were differences in the subscales of the three instruments at T0 (for SCL-90-R) or T1 (for QLQ-C30 and QLQ-BR23) compared with T2. Then, a series of paired-samples t tests were performed to determine whether there was a statistically significant difference between T0 (for SCL-90-R) or T1 (for QLQ-C30 and QLQ-BR23) and T2, in the TAU and FRIPOS groups separately. Finally, a series of 10 multiple regressions were performed after controlling for sociodemographic variables (age, romantic relationship, and presence of sons or daughters) to predict each SCL-90-R subscale at T2 from the SCL-90-R score at T0 and the quality-of-life measure at T2, using the QLQ-C30 scores at T2. We used multiple regression analyses to determine the relative contribution of each predictor (membership in the FRIPOS group vs membership in the TAU group and QoL index) to the total variance explained.
Sample
Women who had been diagnosed with operable breast cancer were included in the study (ICD-10-CM Diagnosis Code C50.919) [110]. The exclusion criteria for the study were (a) cognitive impairment and/or psychiatric comorbidity and/or a physical condition related to the disease that, in the opinion of the treating physicians or the administrator, could lead to invalid data when completing the questionnaires; (b) poor knowledge of the Italian language; and (c) an assumed life expectancy of less than 6 months at the time of initial diagnosis.
A total of 270 women were recruited for this study, of whom 182 gave informed consent to participate and provided data 3 times (participation rate 60%): 103 belong to the FRIPOS group and 79 to the control group (TAU). The mean age of the sample is 57.88 years (SD = 11.55) and ranges from 25 to 87 years. Table 2 shows the sociodemographic variables of the women who participated in the study.
Results
SCL-90-R
Analysis of the results at T0 in terms of psychopathological symptoms did not reveal a significant difference between the two groups (FRIPOS and TAU) in any of the SCL-90-R scales. However, at T2, there was a statistically significant difference between the two groups in all scales of the SCL-90-R. Specifically, in the FRIPOS group, there were improvements in the following: SOM (0.06, 95% CI, 0.01 to 0.12); O-C (0.20, 95% CI, 0.11 to 0.28); DEP (0.18, 95% CI, 0.04 to 0.17); ANX (0.33, 95% CI, 0.24 to 0.43); HOS (0.10, 95% CI, 0.05 to 0.16); PHOB (0.36, 95% CI, 0.01 TO 0.07); PAR (0.10, 95% CI, 0.04 to 0.16); PSY (0.19, 95% CI, 0.13 to 0.25); and on the GSI of 0.16 (95% CI, 0.11 to 0.21). Using the repeated-measures t test, a mean significant worsening on the I-S scale of 0.21 (95% CI, − 0.32 to − 0.09) was found when comparing T0 and T2 in the TAU group (Table 3).
EORTC QLQ-C30
Analysis of the data collected with the QLQ-C30, shown in Table 4, indicates that there were no statistically significant differences between the FRIPOS group and the TAU group at T1, making the two subgroups comparable.
An independent comparison of the two groups at T2 shows that the FRIPOS group performed better on both the QoL scale and the EF scale. Longitudinal comparison (by paired t test analyses) between the groups shows that participation in the FRIPOS project resulted in an improvement on the EF scale of 5.53 (95% CI, − 9.62 to − 1.43), whereas in the TAU group, there was a worsening of 3.45 (95% CI, 0.32 to 7.21), a worsening on the QoL scale of 5.06 (95% CI, 1.40 to 8.73), and on the PF subscale of 0.4.14 (95% CI, 0.16 to 6.63).
In addition, there was evidence of treatment benefit in some of the subscales related to physical symptoms: Patients in the FRIPOS group showed better scores on the indices FA, DY, and SL. There was also a significant worsening of 0.295 (95% CI, − 6.58 to − 0.67) in the DI subscale.
EORTC QLQ-BR23
For the QLQ-BR23 scales specifically related to breast cancer listed in Table 5, patients in the TAU group worsened on both the BRBI scale (8.12 (95% CI, 3.69 to 12.55)) and the BRFU scale (8.02 (95% CI, 2.51 to 13.22)), which was not the case for patients who participated in the FRIPOS project group. Here, there was no significant worsening of the scores and even an improvement in the BRFU score of 9.57 (95% CI, − 15.55 to − 3.58).
For the symptom scales, inclusion of patients in the FRIPOS group resulted in significant stability in all subscales, whereas there was significant deterioration only in the TAU group, in the BRST scale of 8.02 (95% CI, − 11.95 to − 4.07), the BRBS scale of 5.10 (95% CI, − 8.61 to − 1.58), and the BRAS scale of 5.63 (95% CI, − 10.02 to − 1.23).
The role of integrated support and quality of life in explaining symptomatology at T2
A series of multiple regressions were performed to predict each subscale of the SCL-90-R at T2 from each subscale of the SCL-90-R at T0 and the QLQ-C30-derived QL scores at T2. In all regression analyses, linearity was assessed by partial regression plots and a plot of student residuals against predicted scores. Independence of the residuals was demonstrated by a Durbin-Watson statistic with values of 1.476 (hostility subscale) and 2.134 (somatization subscale). Homoscedasticity was determined by visual inspection of a plot of student residuals compared with unstandardized predicted values. There was no evidence of multicollinearity, as judged by tolerance values greater than 0.1. The multiple regression model for somatization statistically significantly predicted somatization at F(6, 170) = 23.545, p < 0.001, adj. R2 = 0.44. The same was true for the following subscales: O-C, with F(6, 170) = 24.000, p < 0.001, adj. R2 = 0.44; I-S, with F(6, 170) = 9.044, p < 0.001, adj. R2 = 0.22; DEP, with F(6, 170) = 23.496, p < 0.001, adj. R2 = 0.43; ANX, with F(6, 170) = 22.541, p < 0.001, adj. R2 = 0.42; HOS, with F(6, 170) = 8.819, p < 0.001, adj. R2 = 0.21; PHOB, with F(6, 170) = 9.672, p < 0.001, adj. R2 = 0.23; PAR, with F(6, 170) = 13.517, p < 0.001, adj. R2 = 0.30; PSY, with F(6, 170) = 17.806, p < 0.001, adj. R2 = 0.36. In addition, the multiple regression model for the Global Severity Index statistically significantly predicted the value of this index at T2, F(6, 170) = 24.503, p < 0.001, adj. R2 = 0.45. In nine of ten regression models, both FRIPOS group membership and the QoL subscale significantly contributed to prediction, with a significance level of at least p < 0.05. Somatization symptomatology was the only subscale for which FRIPOS group membership did not make a statistically significant contribution to prediction, whereas the QoL subscale did. Regression coefficients and standard errors are provided in Table 6.
Discussion
The integrated approach proposed in the FRIPOS project seems to be an adequate response to the claims that appear in the literature related to the concept of holistic management [44, 45] and joins the studies that have already demonstrated its effectiveness and importance [46,47,48].
Indeed, the inclusion of the psycho-oncologist in the treatment has brought significant benefits or at least a state of stability in many areas (in contrast to what happened in the group TAU), especially in relation to several aspects highlighted in the literature: the development of symptomatic manifestations related to psychopathology as a result of or during the journey against cancer and the indices of psychological functioning, especially at the emotional level [49]. Specifically, improvements in symptomatic manifestations (somatization, obsessiveness, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism), emotional functioning, and future outlook were observed in the FRIPOS group. The significantly worse score on the I-S scale in the TAU group could be related to the challenges of a cancer diagnosis at the interpersonal level, such as changes in body image and loss of femininity, or at the level of the life-threatening event [50]. The personal support in the FRIPOS group might have helped patients to cope with and regulate feelings of inadequacy, inferiority, and discomfort in interpersonal interactions, but because of the complexity of the physical and psychological correlates of breast cancer, this aspect needs further investigation.
In addition, the results show the effectiveness of the integrated intervention in terms of quality-of-life scales, especially in terms of fatigue, dyspnea, and sleep disturbances. This result can be taken as an indication of the importance of assessing not only the level of distress, but a more comprehensive picture of the person (including the assessment of unmet needs), taking into account in particular nonverbal behaviors as part of a holistic approach that can be of greater use for interventions in breast cancer patients. One of the advantages of the FRIPOS personalized approach is that it can be adapted to the specific needs of the patient. The psycho-oncologist throughout the oncological path can therefore implement psychological support on the basis of the particular psychological functioning of the person. In line with the literature [51, 52], starting from clinical observation, we found that the patients’ needs concerned emotional health, continuity of care, information, adverse effects on their own body and mind, information, and social support. The composition of these needs in each patient varied on the basis of age, stage of treatment, social status, and family composition.
In nine of ten regression models for psychological symptomatology (all except the somatization subscale), membership in the FRIPOS group together with the quality-of-life subscales significantly contributed to the prediction of the mean score of the respective subscale at T2. These results suggest that the FRIPOS program was effective, confirming the hypothesis and joining the ranks of studies demonstrating the importance of integrated approaches [48]. Furthermore, the regression analyses underscore the importance of monitoring quality of life in relation to the potential psychopathological consequences of breast cancer diagnosis and cancer-related treatments, as called for by the scientific community [53]. An integrated approach also allows the psycho-oncologist to continuously and directly assess the patient's psychophysical state, as unmediated observation allows for the capture of all implicit stress signals that cannot always be accurately captured by conventional stress measurement tools [54]. Another strength of this integrated support is that it addresses all patients indiscriminately, i.e., both those who are unable or unwilling to consciously ask for help [55] and those who face unmet needs and find a setting in which to talk about their problems. The integrated intervention does not take the form of a psychological takeover through coercion, but by offering a resource that the patient can access directly according to the perceived needs, an intervention that can adapt to the complexity of each case, and the heterogeneity of the types of patients [56, 57].
Further studies on the cost-effectiveness of an integrated approach are needed, especially for health systems such as the Italian one, which faces an increasing demand for integrated psycho-oncology services but also dwindling financial resources, especially for psychosocial care.
Despite methodological limitations such as the relatively small sample size, the use of self-reports, and a possible implicit influence of the greater participation in the FRIPOS group (in which the women who completed all three surveys were more numerous), this study may provide important general insights for the clinical setting, including various health situations in which the presence of a parallel psychological support network in conjunction with medical interventions could significantly affect the quality of life and psychophysiological balance of those involved in the treatment process. Another limitation is that due to the pioneering and exploratory nature of this project, there is not yet a manualization of the integrative interventions. For this reason, the intervention was planned using information from the scientific literature on actual difficulties reported by cancer patients (especially breast cancer patients), but no measures were taken to ensure consistency of treatment. This problem needs to be addressed in the future. Potential psychological variables that would be useful to examine in future research involve perceived support by family and partner and specific personality traits.
Conclusions
The FRIPOS project aims to create a holistic pathway for the psycho-oncological care of cancer patients. It also aims to provide Italian health policy makers with a solid decision-making basis for the timely introduction of integrated psycho-oncology services in the Italian health system. In this study, the involvement of a psycho-oncologist during cancer treatment was found to be crucial for breast cancer patients’ psychological well-being and coping with several aspects related to the disease. To improve the situation of women with breast cancer (as well as other cancer patients), it is desirable that psychological support be offered to provide patients with a flexible, integrated, and adaptable treatment pathway for each person’s specific individuality.
Data availability
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
References
(2022) Il tumore della mammella. https://www.salute.gov.it/portale/tumori/dettaglioContenutiTumori.jsp?lingua=italiano&id=5538&area=tumori&menu=vuoto. Accessed 3 Aug 2022
Gori S, Miglietta F, Modena A (2021) Mammella. In: AIOM, AIRTUM, SIAPEC-IAP et al (eds) I numeri del cancro in Italia 2021. Intermedia Editore, Orvieto (TR), pp 64–66
Gandino G, Dipaola D, Triscio V et al (2017) The impact of breast cancer on the body, femininity and relations a research through the Rorschach test. Minerva Psichiatr 58:135–143. https://doi.org/10.23736/S0391-1772.17.01933-1
Holland JC, Weiss TR (2010) History of psycho-oncology. In: Holland JC, Jacobsen PB, Loscalzo MJ (eds) Psycho-oncology, 2nd edn. Oxford University Press, New York, pp 3–12
Appleton L, Poole H, Wall C (2018) Being in safe hands: patients’ perceptions of how cancer services may support psychological well-being. J Adv Nurs 74:1531–1543. https://doi.org/10.1111/jan.13553
Faretta E, Borsato T, Civilotti C et al (2016) EMDR and CBT: a comparative clinical study with oncological patients. J EMDR Pract Res 10:215–227. https://doi.org/10.1891/1933-3196.10.3.215
Chambers SK, Hutchison S, Mihalopoulos C, Dunn JC (2014) A randomized trial comparing two low-intensity psychological interventions for distressed patients with cancer and their caregivers. Oncol Nurs Forum 41:E256–E266. https://doi.org/10.1188/14.ONF.E256-E266
Ye M, Du K, Zhou J et al (2018) A meta-analysis of the efficacy of cognitive behavior therapy on quality of life and psychological health of breast cancer survivors and patients. Psychooncology 27:1695–1703. https://doi.org/10.1002/pon.4687
Ledesma D, Kumano H (2009) Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology 18:571–579. https://doi.org/10.1002/pon.1400
Sagar SM (2016) Integrative oncology: are we doing enough to integrate psycho-education? Future Oncol 12:2779–2783. https://doi.org/10.2217/fon-2016-0345
Kissane D (2003) Family focused grief therapy: the role of the family in preventive and therapeutic bereavement care. Bereavement Care 22:6–8. https://doi.org/10.1080/02682620308657563
Meggiolaro E, De Padova S, Ruffilli F et al (2021) From distress screening to uptake: an Italian multicenter study of cancer patients. Cancers (Basel) 13:3761. https://doi.org/10.3390/cancers13153761
Arora NK (2003) Interacting with cancer patients: The significance of physicians’ communication behavior. Soc Sci Med 57:791–806. https://doi.org/10.1016/S0277-9536(02)00449-5
Van Scheppingen C, Schroevers MJ, Smink A et al (2011) Does screening for distress efficiently uncover meetable unmet needs in cancer patients? Psychooncology 20:655–663. https://doi.org/10.1002/pon.1939
Soothill K, Morris SM, Harman J et al (2001) The significant unmet needs of cancer patients: probing psychosocial concerns. Support Care Cancer 9:597–605. https://doi.org/10.1007/s005200100278
Swartzman S, Booth JN, Munro A, Sani F (2017) Posttraumatic stress disorder after cancer diagnosis in adults: a meta-analysis. Depress Anxiety 34:327–339. https://doi.org/10.1002/da.22542
Ghirardello D, Munari J, Testa S et al (2018) Italian adaptation of the brief modified experiences in close relationships scale in a sample of cancer patients: factor analysis and clinical implications. Res Psychother: Psychopathol Process Outcome 21(3). https://doi.org/10.4081/ripppo.2018.319
Eakin EG, Strycker LA (2001) Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: patient and provider perspectives. Psychooncology 10:103–113. https://doi.org/10.1002/pon.500
Dilworth S, Higgins I, Parker V et al (2014) Patient and health professional’s perceived barriers to the delivery of psychosocial care to adults with cancer: a systematic review. Psychooncology 23:601–612. https://doi.org/10.1002/pon.3474
Rose S, Boyes A, Kelly B et al (2018) Help-seeking behaviour in newly diagnosed lung cancer patients: assessing the role of perceived stigma. Psychooncology 27:2141–2147. https://doi.org/10.1002/pon.4779
Hutchison SD, Steginga SK, Dunn J (2006) The tiered model of psychosocial intervention in cancer: a community based approach. Psychooncology 15:541–546. https://doi.org/10.1002/pon.973
Singer S, Danker H, Briest S et al (2014) Effect of a structured psycho-oncological screening and treatment model on mental health in cancer patients (STEPPED CARE): study protocol for a cluster randomized controlled trial. Trials 15:1–6
Savard J, Ivers H, Savard M-H et al (2021) Efficacy of a stepped care approach to deliver cognitive-behavioral therapy for insomnia in cancer patients: a noninferiority randomized controlled trial. Sleep 44:zsab166
NICE | The National Institute for Health and Care Excellence. https://www.nice.org.uk/guidance/csg4/resources/improving-supportive-and-palliative-care-for-adults-with-cancer-pdf-773375005. Accessed 3Aug 2022
Watson M, Dunn J (2016) The multidisciplinary art and science of cancer care: integrating psycho-oncology. Future Oncol 12:2775–2778. https://doi.org/10.2217/fon-2016-0374
Philip EJ, Merluzzi TV (2016) Psychosocial issues in post-treatment cancer survivors: desire for support and challenges in identifying individuals in need. J Psychosoc Oncol 34:223–239. https://doi.org/10.1080/07347332.2016.1157716
Jacobs LA, Blauch AN, Pucci DA et al (2017) Does screening for anxiety and depression efficiently identify patients who want help? J Clin Oncol 35:e21604–e21604. https://doi.org/10.1200/jco.2017.35.15_suppl.e21604
Absolom K, Holch P, Pini S et al (2011) The detection and management of emotional distress in cancer patients: the views of health-care professionals. Psychooncology 20:601–608. https://doi.org/10.1002/pon.1916
Sharpe M, Walker J, Hansen CH et al (2014) Integrated collaborative care for comorbid major depression in patients with cancer (SMaRT Oncology-2): a multicentre randomised controlled effectiveness trial. The Lancet 384:1099–1108. https://doi.org/10.1016/S0140-6736(14)61231-9
Li M, Kennedy EB, Byrne N et al (2017) Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psychooncology 26:573–587. https://doi.org/10.1002/PON.4286
Commission to the European Parliament and the Council (2021) Europe’s beating cancer plan. https://health.ec.europa.eu/system/files/2022-02/eu_cancer-plan_en_0.pdf. Accessed 3 Aug 2022
Grimmett C, Heneka N, Chambers S (2022) Psychological interventions prior to cancer surgery: a review of reviews. Curr Anesthesiol Rep 12:78–87. https://doi.org/10.1007/s40140-021-00505-x
Lucchini D, Giampaolo R, Fogazzi G et al (2020) Fil-Rouge: implementazioni dell’approccio integrato nell’iter terapeutico antitumorale in un campione di donne affette da neoplasia mammaria: progetto pilota. Psicologia della Salute 3:5–34. https://doi.org/10.3280/PDS2020-003001
Seiler A, Jenewein J (2019) Resilience in cancer patients. Front Psychiatry 10:208. https://doi.org/10.3389/fpsyt.2019.00208
Kalter J, Verdonck-de Leeuw IM, Sweegers MG et al (2018) Effects and moderators of psychosocial interventions on quality of life, and emotional and social function in patients with cancer: an individual patient data meta-analysis of 22 RCTs. Psychooncology 27:1150–1161. https://doi.org/10.1002/pon.4648
Carlson LE, Waller A, Mitchell AJ (2012) Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol 30:1160–1177. https://doi.org/10.1200/JCO.2011.39.5509
De Vincentis G, Monari F, Baldari S et al (2018) Narrative medicine in metastatic prostate cancer reveals ways to improve patient awareness & quality of care. Future Oncol 14:2821–2832. https://doi.org/10.2217/fon-2018-0318
Fobair P, Stewart SL, Chang S et al (2006) Body image and sexual problems in young women with breast cancer. Psychooncology 15:579–594. https://doi.org/10.1002/pon.991
Boquiren VM, Esplen MJ, Wong J et al (2016) Sexual functioning in breast cancer survivors experiencing body image disturbance. Psychooncology 25:66–76. https://doi.org/10.1002/pon.3819
Harrison JD, Young JM, Price MA et al (2009) What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer 17:1117–1128. https://doi.org/10.1007/s00520-009-0615-5
Derogatis LR (1994) Symptom Checklist-90-R: administration, scoring & procedure manual for the revised version of the SCL-90. National Computer Systems, Minneapolis
Prunas A, Sarno I, Preti E et al (2012) Psychometric properties of the Italian version of the SCL-90-R: a study on a large community sample. Eur Psychiatry 27:591–597. https://doi.org/10.1016/j.eurpsy.2010.12.006
Osoba D, Zee B, Pater J et al (1994) Psychometric properties and responsiveness of the EORTC Quality of Life Questionnaire (QLQ-C30) in patients with breast, ovarian and lung cancer. Qual Life Res 3:353–364. https://doi.org/10.1007/BF00451727
Peckham M, Pinedo B, Veronesi U (1996) Oxford textbook of oncology. Elsevier Science
Lopez G, McQuade J, Cohen L et al (2017) Integrative oncology physician consultations at a comprehensive cancer center: analysis of demographic, clinical and patient reported outcomes. J Cancer 8:395–402. https://doi.org/10.7150/jca.17506
Powell Davies G, Williams AM, Larsen K et al (2008) Coordinating primary health care: an analysis of the outcomes of a systematic review. Med J Aust 188:S65–S68. https://doi.org/10.5694/j.1326-5377.2008.tb01748.x
Kusch M, Labouvie H, Schiewer V et al (2022) Integrated, cross-sectoral psycho-oncology (isPO): a new form of care for newly diagnosed cancer patients in Germany. BMC Health Serv Res 22:1–31. https://doi.org/10.1186/s12913-022-07782-0
Walker J, Sharpe M (2009) Depression care for people with cancer: a collaborative care intervention. Gen Hosp Psychiatry 31:436–441. https://doi.org/10.1016/j.genhosppsych.2009.05.010
Civilotti C, Botto R, Maran DA et al (2021) Anxiety and depression in women newly diagnosed with breast cancer and waiting for surgery: prevalence and associations with socio-demographic variables. Medicina (Lithuania) 57:454. https://doi.org/10.3390/medicina57050454
Wang YH, Li JQ, Shi JF et al (2020) Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry 25:1487–1499. https://doi.org/10.1038/s41380-019-0595-x
Chae BJ, Lee J, Lee SK et al (2019) Unmet needs and related factors of Korean breast cancer survivors: a multicenter, cross-sectional study. BMC Cancer 19:839. https://doi.org/10.1186/s12885-019-6064-8
Liu X, Chen Y, Cheng AS et al (2022) Conceptualizing problems with symptoms, function, health behavior, health-seeking skills, and financial strain in breast cancer survivors using hierarchical clustering. J Cancer Surviv 16:751–759. https://doi.org/10.1007/s11764-021-01068-w
Mokhatri-Hesari P, Montazeri A (2020) Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual Life Outcomes 18:1–25
Götz A, Kröner A, Jenewein J, Spirig R (2019) Evaluation of the adherence of distress screening with the distress thermometer in cancer patients 4 years after implementation. Support Care Cancer 27:2799–2807
Merckaert I, Libert Y, Messin S et al (2010) Cancer patients’ desire for psychological support: prevalence and implications for screening patients’ psychological needs. Psychooncology 19:141–149. https://doi.org/10.1002/pon.1568
Faretta E, Civilotti C (2016) EMDR therapy in psycho-oncology: a bridge between mind and body. J EMDR Pract Res 10:138–152. https://doi.org/10.1891/1933-3196.10.3.138
Slevin ML, Nichols SE, Downer SM et al (1996) Emotional support for cancer patients: what do patients really want? Br J Cancer 74:1275–1279. https://doi.org/10.1038/bjc.1996.529
Acknowledgements
We thank the patients who participated in the study and dedicated time and resources at a particularly sensitive moment in their lives. We also thank the professionals who made the development and implementation of the Fil-Rouge project possible: Psychological Service of the Clinical Institute of S. Anna Brescia, San Donato Group; Scientific Committee of the PRIAMO Association; Service of Minimally Invasive Diagnosis and Intervention in Breast Care of the Clinical Institute of S. Anna Brescia, San Donato Group; Service of Breast Diagnosis and Minimally Invasive Intervention of the Clinical Institute of San Rocco OME, San Donato Group; Service of Breast Radiology; U.O. General Surgery of S. Anna Clinical Institute Brescia, San Donato Group; Pathological Anatomy Service of S. Anna Clinical Institute Brescia, San Donato Group; Department of Medical Oncology of S. Anna Clinical Institute Brescia, San Donato Group; Department of Oncology and Oncology Day Hospital of S. Anna Clinical Institute Brescia, San Donato Group; Department of Radiotherapy and Clinical Oncology of S. Anna Clinical Institute Brescia, San Donato Group; Secretariat of the Breast Unit of S. Anna Clinical Institute Brescia, San Donato Group; and Analytical Laboratory of S. Anna Clinical Institute Brescia, San Donato Group.
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. This research was funded by Associazione Priamo, viale Piave, 101—25123 Brescia; www.associazionepriamo.it.
Author information
Authors and Affiliations
Contributions
Conceptualization, C.C., D.L. and F.P.; methodology, D.L., G.F., F.P., A.Be., A.Bu., V.G., N.R.; formal analysis, C.C. and A.D.B.; data curation, C.C., E.D.; writing-original draft preparation, C.C.; writing, C.C., A.D.B., E.D., G.D.F., G.G.; supervision, D.L., F.V., G.D.F., G.G.; project administration, D.L., G.F., F.P., A.Be., A.Bu., V.G., N.R.; funding acquisition, D.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the S. Anna Clinical Institute in Brescia (Prot. Number: 1.0; 06/06/2016).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Civilotti, C., Lucchini, D., Fogazzi, G. et al. The role of integrated psychological support in breast cancer patients: a randomized monocentric prospective study evaluating the Fil-Rouge Integrated Psycho-Oncological Support (FRIPOS) program. Support Care Cancer 31, 266 (2023). https://doi.org/10.1007/s00520-023-07732-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07732-4