Abstract
Purpose
The main aim of the trial was to assess the combined impact of graded Thera-Band strengthening exercises and scapular stabilization exercises on shoulder pain, physical function, and quality of life (QoL) in post-mastectomy adhesive capsulitis (AC).
Methods
Seventy females with unilateral post-mastectomy AC partook in the trial. Participants were subdivided equally into two groups at random. Both groups obtained the traditional physical therapy program; in addition, the intervention group received graded Thera-Band exercises for shoulder muscles and scapular stabilization exercises 5 days a week for 8 weeks. Range of motion (ROM) and muscle power of shoulder were assessed by digital goniometer and handheld dynamometer, respectively. Disability of the Arm, Shoulder, and Hand questionnaire (DASH) was utilized for assessment of shoulder function and visual analogue scale (VAS) for pain measurement while short-form (SF-36) for QoL assessment. All evaluation data was recorded prior to the trial and at the eighth week of interventions for both groups.
Results
All participants achieved improvements in shoulder ROM, muscle power, pain, and all aspects of QoL; however, higher statistical improvements were reported in all measurements with respect to strengthening exercises group (p < 0.001).
Conclusion
The addition of graded Thera-Band strengthening exercises and scapular stabilization exercises in post-mastectomy AC rehabilitation program has significant benefits in shoulder function and patients’ QoL.
Trial registration: This study is retrospectively registered at ClinicalTrials.gov NCT05311839.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer surgeries particularly mastectomy results in limited shoulder movement which can lead to arm, shoulder pain, and stiffness [1]. Females who underwent mastectomy have reported a significantly higher incidence of shoulder morbidity (17%) [2]. Shoulder joint connective tissue fibrosis is common in post-mastectomy patients [3]. One of the most common symptoms of upper extremity morbidities is restriction of shoulder joint range of motion (ROM) which is linked to a lower quality of life (QoL) [4].
Adhesive capsulitis (AC) or “frozen shoulder” is an insidious inflammatory disorder characterized by a painful, progressive decrease in passive or active glenohumeral joint ROM caused by gradual fibrosis and subsequent contracture of the glenoid capsule [5]. AC frequently progresses through 3 different phases; the first one is the painful freezing phase, remains from 2 to 9 months, and is associated with emergence of sharp, diffuse shoulder discomfort that usually aggravates during night; the second phase is the frozen phase, lasts from 4 to 12 months, where pain starts to fade with a gradual decrease in glenohumeral joint ROM; and the last phase is the thawing phase where there is a gradual regain of ROM and takes from 5 months to 2 years to complete [6, 7].
AC can be treated either conservatively or surgically. Conservative treatment consists of a variety of exercise techniques and physical therapy modalities such as hot–cold therapy [8], transcutaneous electrical nerve stimulation (TENS), ultrasound (US), acupuncture [9, 10], and laser [11]. Active and passive ROM exercises, self-stretching, stretching exercises under the guidance of a physiotherapist, mobilization and manipulation techniques, resistance exercises, patient education, and home exercises are all part of the exercise program [12].
Exercise therapy might help in the reduction of pain and restoration of the range, coordination, and control of movement in patients with AC [13]. Graded resistance exercises are effective in decreasing fatigue levels and enhancing functional capacity and muscle strength [14]. Progressive strengthening exercise is extremely effective in reducing sarcopenia. Strength training improves muscle strength by increasing muscle mass and enhancing the recruitment and the firing rate of motor units [15]. Thera-Bands are a type of resistance exercise training tools which can provide a variable resistance and allow changes over ROM, thus preventing the risk of higher weight loading during strengthening exercises. In addition, elastic bands can provide efficient resistance and enhance muscle activation for promoting muscle strength in treatment of shoulder diseases. They are frequently used during exercise rehabilitation programs due to their simplicity, economic, and safety benefits [16,17,18].
The scapular stabilization exercise can be applied to patients with limited shoulder joint mobility and functional deterioration such as shoulder impingement syndrome, AC, and rotator cuff injury. As a result, rehabilitation exercises which strengthen the scapula’s stability can be extremely beneficial in rehabilitation treatment of patients with shoulder pain and problems [19].
Since the incidence of shoulder morbidity is six times higher following mastectomy compared to conservative therapy [20], which in turn influencing the patients’ ability on performing ADL, in addition to the lack of literature research on AC rehabilitation following mastectomy, the need of developing an efficient exercises program is necessary; hence, this experiment targeted to assess the impact of combining Thera-Band strengthening exercises with scapular stabilization training on AC following mastectomy in term of shoulder pain, function, and QoL.
Methods
Design and setting
This study was a randomized controlled experimental trial and was approved by the Ethical Committee of Faculty of Physical Therapy, Cairo University. The study was retrospectively registered in the Clinical Trials Registry (No: NCT05311839), and it was carried out between January 2021 and December 2021 at the outpatient clinic of Faculty of Physical Therapy, Cairo University. All the procedures used were conducted following the ethical rules of the Declaration of Helsinki.
Participants
Seventy females diagnosed with one-sided post-mastectomy AC participated in this study. All patients were diagnosed by a specialized orthopedist. The procedures of this trial were carried out at the outpatient clinic at the Faculty of Physical Therapy, Cairo University. Females who met the following inclusion criteria participated in the study; age ranged from 40 to 60 years, 2nd phase of AC, shoulder pain and stiffness for at least 3 months, and restriction in shoulder ROM (involving flexion, abduction, and internal/external rotation) less than 50% when compared to the other shoulder. The exclusion criteria included shoulder or acromioclavicular joint osteoarthritis, bone diseases, infection, severe osteoporosis, tumors or metastasis, history of previous shoulder trauma or accidental injuries, previous history of dislocation, surgery on the specific shoulder, and any other shoulder problems as supraspinatus tendonitis and impingement, neurological diseases (parkinsonism, stroke, radiating pain to arm), recent shoulder fracture or wound, diabetes mellitus, rheumatoid arthritis, and severe psychiatric illness.
Prior to participating in the trial, all participants were educated about the trial’s purposes, benefits, and steps and signed a consent form. Small groups of one to four patients underwent the sessions at a time, supervised by specialized physical therapist. The study included two equal groups of participants who were allocated randomly. The intervention group received graded Thera-Band exercises for the restricted shoulder ROM (flexion, abduction, and internal/external rotation) and scapular stabilization exercises (60 min, 5 days per week for 8 weeks) plus a conventional physiotherapy program including hot packs, active ROM exercises, pendular exercises, wall climb exercises, mobilization exercises, and shoulder capsular stretching. The control group obtained only the conventional physiotherapy program (30–40 min, 5 days weekly for 8 weeks).
Sample size and randomization
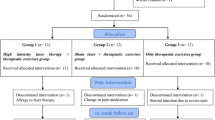
The estimated sample size for this trial was 32 participants for each group, as calculated using G*POWER statistical software (version 3.1.9.2) according to shoulder external rotation data from a pilot study conducted on 5 subjects per group. α = 0.05, power is 80%, effect size = 0.72, and allocation ratio N2/N1 = 1 was used in the calculations. For a possible drop out, the sample size was increased by 10%. Randomized assignment of patients was done equally either to intervention group (n = 35) or control group (n = 35). The randomization process was carried out by a physiotherapist who was not involved in the data collection processes. Each patient received a unique computer-generated random code using the GraphPad software© (1:1 simple randomization), concealed in a sealed envelope. The sealed envelopes were given to the physiotherapist before the treatment. The results were collected prior to the trial and at the 8th week of therapy by therapist who was blind to the distribution process.
Treatment procedures
All patients within both groups received the conventional physiotherapy program, 5 days a week for 8 weeks, and the duration of treatment was approximately 30–40 min.
The control group
The participants within this group received the conventional physiotherapy program including hot packs (5–10 min), passive mobilization exercises for glenohumeral (GH) joint, and scapulothoracic articulation. GH joint mobilizations (posterior gliding for increasing flexion and internal rotation, caudal glide for increasing abduction, and anterior gliding for increasing external rotation). Scapulothoracic mobilization was applied for improving the movements of scapula (protraction/retraction, elevation/depression, and rotation). For active ROM exercises and pendular exercises, the patient was instructed to lean forward and place the unaffected hand on a table. While keeping a straight back and a relaxed shoulder, softly sway the arm forth and backward; the exercise was repeated by shifting the arm from side to side and then in an orbicular movement (10 reps, 5 times per day), wall climb exercises (hold for 15–30 s at the peak, 10 reps, 5 times daily), and capsular stretching exercises (anterior, posterior and inferior capsular stretches) and sustaining for 15–30 s, 5 reps, 5 times/day [21, 22].
The intervention group
The participants within this group received graded Thera-Band exercises and scapular stabilization exercises (60 min, 5 days per week for 8 weeks) plus a conventional physiotherapy program.
Thera-Band exercises
Patients in the intervention group received graded Thera-Band exercises (Thera-Band®, Hygenic Corporation, Akron, OH, USA). For Thera-Band application for shoulder flexors and abductors, the patient was in a comfortable standing position with both feet firmly positioned on the Thera-Band. The patient was instructed to grasp the end of the Thera-Band and gradually flex and abduct the shoulder from the starting position, hold for (25 s), and then return to the starting position without bouncing. For shoulder internal rotation, the patient was asked to stand and hold the Thera-Band in the hand while the direction of resistive power away from the side at the level of elbow which is bent to 90°. The patient was instructed to internally rotate the arm by pulling across the front of the trunk. For shoulder external rotation, the patient was instructed to stand with Thera-Band beside the body at level of elbow and to flex her elbow to 90°, grasping the elastic band and rotating the arm laterally. All patients performed the above exercises for 30 min with 2–3 series of 10–15 reps of every exercise. All patients started strengthening exercises with the yellow color, progressed to the red, and then the green. When the patient could easily complete three sets of 10–15 reps, progression to the next color was considered [21,22,23].
Scapular stabilization exercises
In addition to graded Thera-Band exercises, the patients in the intervention group performed the following scapular stabilization exercises for 30 min, 10 reps each:
-
1)
Scapular clock exercises: in the standing position, the patient was asked to place the arm on a wall with fully extended elbow, with the fingers directed towards the 12, 3, 6, and 9 o’clock positions. These exercises improved scapular elevation, protraction, depression, and retraction, respectively.
-
2)
Towel slide exercises: with slightly flexed elbow, the patient was instructed to place the hand on a towel on the wall and wash the wall in approximately a 12 inch backward and forward motion, moving from the extended arm, retracted scapula, and to a flexed arm and protracted scapula.
-
3)
Ball stabilization exercises: while standing close to the wall, the participant was asked to position her affected hand on the ball and keep the ball from moving as disturbance was applied in different directions.
-
4)
Lawnmower exercises: the patient stood with abducted legs, bent knees, and holding a weight in the hand for resistance. The patient was asked to pull using large amounts of lower extremity extension and trunk rotation to guide the shoulder movement.
-
5)
Serratus anterior punch: in standing position, the patient was instructed to perform alternative serratus anterior punches while holding the Thera-Band for resistance [24, 25].
Outcome measurements
Physical function, pain, and QoL were among the outcome measures. The measures were taken before the trial and at the end of the eighth week of therapy. Shoulder range of motion, muscles strength, and the Disability of the Arm, Shoulder, and Hand questionnaire (DASH) are all used to measure physical function. Shoulder pain was assessed by visual analogue scale (VAS). The Medical Outcomes Study short-form questionnaire (SF-36) was used to assess QoL.
A digital goniometer with good reliability (r > 0.84) was utilized to quantify shoulder flexion and abduction ROM in supine with extended elbow, while internal/external rotations were measured in sitting with adducted shoulder and mid position of forearm. All measures were taken 3 times, and then the average was scored [26, 27].
A handheld dynamometer (J Tech Commender Muscle Tester, Salt Lake City, UT, USA), a valid tool (r = 0.81), was employed to test the muscle power of shoulder flexors, abductors, and internal/external rotators by measuring maximum isometric contraction in kg. Each record was done 3 times, and then the average was scored [28].
The DASH was designed to evaluate upper limb disorders and impairment and track changes and functional level over time. This questionnaire’s Arabic version is regarded as a plain, reliable (r = 0.97), and validated (r = 0.94) measurement instrument. The more the score, the more severe the symptoms [29].
The VAS is a reliable measure with an ICC of 0.97, consists of 10-cm line, and was utilized to quantify the pain severity within shoulder, where the score of zero means no pain, while a score of ten means significant pain [30].
The short-form SF-36, including physical function, role physical, general health, vitality, bodily pain, mental health, role emotional, and social function, was used for assessment of patients’ QoL. The Cronbach’s alpha coefficient was 0.94, while the inter-rater reliability was outstanding (ICC = 0.98) [31].
Statistical analysis
An unpaired t test was employed to compare subjects’ characteristics between the groups. The chi-squared test was used to compare the allocation of the afflicted arm and adjunctive therapy between the groups. For ensuring normal data allocation, the Shapiro–Wilk test was utilized. For group homogeneity determination, Levene’s test for homogeneity of variances was utilized. The effect of therapy on VAS, DASH, shoulder ROM and strength, and QoL was investigated using a mixed model MANOVA. Post hoc test utilizing Bonferroni correction was performed for subsequent various comparisons. All statistical measurements had a significant level of p 0.05. For all statistical analysis, IBM SPSS (Chicago, IL, USA) version 25 for Windows (IBM SPSS, Chicago, IL, USA) was used.
Results
Participants’ characteristics
The patients’ flow diagram through the trial is illustrated in Fig. 1. Seventy patients participated in this study with no significant difference in subjects’ age, BMI, affected arm, and adjunctive therapy distribution between the groups (p > 0.05) (Table 1).
Intervention effect on VAS, DASH, shoulder ROM, and strength and QoL
The interaction of intervention and time was significant (F (18,51) = 139.81, p = 0.001, = 0.98). The main effect of time was significant (F (18,51) = 1181.78, p = 0.001, = 0.99). The main effect of intervention was significant (F (18,51) = 35.59, p = 0.001, = 0.92).
Comparisons in each group
The VAS and DASH of both groups were statistically lower following intervention contrast to pre-intervention (p 0.001) (Table 2). The post-therapy shoulder ROM (flexion, abduction, external and internal rotation) and shoulder strength (flexors, abductors, internal/external rotators) of both groups were statistically higher than the pre-therapy levels (p 0.001) (Tables 3 and 4). Both groups demonstrated a significant improvement in all aspects of their QoL after intervention compared to pre-intervention (p < 0.001) (Table 5).
Comparisons between both groups
Pre-therapy, statistical difference between the groups was not reported (p > 0.05). Following therapy, the intervention group showed statistical lowering in VAS and DASH than the control group (p < 0.001) (Table 2). Moreover, comparing to the control group, the intervention group had higher statistical improvements in shoulder ROM (flexion, abduction, external/internal rotation), strength (flexors, abductors, external and internal rotators) (Tables 3 and 4), and in all aspects of QoL after therapy (p < 0.001) (Table 5).
Discussion
Pain and ROM restriction within AC are likely due to fascial constraints, muscle stiffness with trigger spots, in addition to capsular and ligamentous rigidity [32]. This study was a randomized retrospective-controlled trial that aimed to assess the impacts of shoulder strengthening and scapular stabilizing exercises on physical function, pain, and QoL in post-mastectomy patients with AC, where the control group received 30–40 min of traditional therapy and the intervention group with both interventions received > 60 min. The results illustrated higher statistical improvements of all parameters in favor to the strengthening exercises group. All patients in this trial achieved improvement in pain and shoulder joint ROM, as mobilization has been showed to lower pain through the neurophysiologic impacts of mobilization on peripheral mechanoreceptor activation and nociceptors inhibition; additionally, improvement of ROM could be explained by the effect of mobilization on shoulder AC as posterior–anterior glide was chosen to improve the outer ROM, while caudal glide was chosen to improve abduction. It is possible that the glenohumeral joint’s posterior–anterior and caudal glides improved capsular extensibility and lengthened soft tissues, which were restricting joint motion. As a result of the greater capsular extensibility, the glenohumeral joint may have had more ROM. These treatments are also hypothesized to boost proprioceptive and kinesthetic sensations within the joint, allowing participants to perform tasks within their new ROM; as a result, the individual’s ROM can be maintained. Another possible explanation is the impact of stretching exercises which have been shown to improve the extensibility of soft tissue through the creep response, modifying viscoelastic characteristics and hence increasing ROM. Individuals must perform tasks within their newly acquired range of motion in order to retain joint motion. This conclusion backs up prior studies indicating that mobilization and stretching exercises can help with AC [33,34,35,36].
Following mastectomy, the main cause of shoulder dysfunction is not only the glenohumeral joint disorder but also the adhesions in the axillary and pectoral areas between the pectoral muscles, subcutaneous tissue, and skin that may prevent complete extension of the pectoralis, resulting in limitation of both shoulder flexion and abduction [37, 38]. So, introducing progressive strengthening exercises during treatment could overcome the consequence muscles weakness caused by adhesions and encourage gaining more shoulder range, promote neuromuscular control, ameliorate general strength, and facilitate optimal strength ratios of the rotator cuff and scapular rotator muscles, and hence facilitate rapid recovery from AC, and that may illustrate the higher statistical improvement in all shoulder ROM within the resistance exercises group compared to the other group which in turn facilitate the activities of daily living (ADL) and improve the shoulder function. These results support and come in line with other studies [21,22,23, 39,40,41,42] and emphasize on the prominent role of strengthening exercises in AC rehabilitation, as Harishkumar et al. (2017) [21] added Thera-Band strengthening exercises to traditional care in AC cases and evaluated the shoulder function and ROM after 3 weeks of intervention which showed higher statistical improvements than receiving traditional care only, while Rawat et al. (2016) [22] studied the impacts of gradual resistance exercises of rotator cuff muscles beside receiving TENS and shoulder joint mobilization techniques for 1 month and reported significant ameliorations in shoulder functional level, pain, muscle strength, and ROM. Datar and Devi [23] studied the effects of Thera-Band strengthening exercises on shoulder dysfunction following mastectomy in term of muscle power, shoulder functional capacities, and ADL; evaluations were done after 2 months of intervention and demonstrated that Thera-Band exercises have significantly improved the outcome measures for strength and daily tasks involving upper extremity.
Shrug sign is one of the issues that may be exhibited during application of resistance exercises for shoulder abduction. One of the benefits of Thera-Band is the ability to assist in rotator cuff retraining during starting abduction, as the elastic band generates “upward and inward” resistance vector against which the patient must push in a “downward and outward” direction. This action activates the start of abduction additionally the rotator cuff’s depression and stability activities, which occur before and during abduction. According to anecdotal evidence, this exercise helps patients with the shrug sign diminish early upper trapezius activity during abduction [32].
In terms of muscle strength, the resistance training group demonstrated better statistical results, which could be illustrated by the fact that strengthening exercises cause significant physiological variations in skeletal muscles including contractile and/or non-contractile muscle compositions. Mechanical stress causes disruption of myofibers and extracellular matrix, which stimulates protein synthesis, resulting in muscle growth by increment the sarcomeres number, which leads to an increase in pinnation angle and fascicle length and so muscle expansion [43].
Several studies have documented alteration of scapular motion in the mastectomy side which in turn affect the shoulder motion pattern and contribute to incidence of frozen shoulder [44, 45]; scapular stabilizers’ weakness causes a disruption in the scapula–humeral rhythm, resulting in shoulder dysfunction and micro-damage to the shoulder muscles, capsule, and ligaments. The scapula must rotate vertically, tilt posteriorly, and rotate externally during overhead exercises; scapular stabilizers’ weakness causes an imbalance of force coupling between the trapezius, serratus anterior, and rhomboids, resulting in downward rotation, anterior tilting, and internal rotation of the scapula during arm abduction. This fatigue-induced weakness deficit may have a detrimental influence on scapular posture and allow for increased lateral scapular gliding during functional activities [25], so scapular stabilization is an important part of exercises therapy for optimizing scapular alignment during upper extremity movement and for providing direct control of the scapular posture, allowing for proper length–tension ratios in the shoulder muscles. Hence, adding scapular stabilization exercises in the rehabilitation program is very essential and coincided with various studies that support the role of these exercises in normally restoring both shoulder and scapular balance and motion [24, 25, 46,47,48,49] and that could be explained as one of the factors that assist in shoulder AC improvement, as Kirthika et al. (2015) [24] and Gulwani (2020) [25] added scapular stabilization exercises to conventional care in cases with 2nd phase of AC and evaluated the shoulder function and ROM after 2 weeks of intervention and concluded that those exercises are beneficial for enhancing shoulder ROM and functional abilities; also, Yatheendra et al. (2015) [46] evaluated the impacts of combined scapular stabilization exercises and mobilization techniques on patients with AC for 4 weeks; the study comes to the conclusion that both interventions are effective in reducing shoulder discomfort, enhancing ROM, and improving functional capacity in AC.
Moreover, the experimental group demonstrated greater improvement in ADL regarding to the DASH scores and additionally in QoL which may be attributed to the crucial role of strengthening exercises among the various forms of physical exercise programs due to the link between muscle impairment, pain, and dysfunction [50], as strengthening of shoulder and scapular stabilizers has significant impacts in reducing pain and improving shoulder ROM, functional capacity, and muscle power by regaining scapula–humeral rhythm in AC [32].
The study confirmed the importance of exercises therapy in AC management without reporting any adverse effects and presents the preliminary evidences for introducing strengthening exercises as an essential part in AC rehabilitation; however, some limitations must be considered when explaining these results; the most significant drawback of this experiment was the lack of scapular movement analysis which could provide better statistical results; other restrictions are the absence of blinding during the treatment sessions and absence of AC imaging assessments that could provide better prognosis; also the long-term effect of treatment was not examined due to the difficulty of following up after the trial, so future trials analyzing the scapular motion with patients’ follow-up are recommended; also it is critical to promote knowledge about the protection, early diagnosis, and quick treatment of shoulder problems following mastectomy in order to reduce women sufferance and financial costs, so trials should be conducted to evaluate early physical therapy intervention in prevention shoulder morbidity following mastectomy; moreover, evaluation of the impact of different approaches of exercises therapy with longer duration should be carried out.
Conclusion
Rehabilitation exercises program including progressive strengthening of both scapular and shoulder muscles played a significant role in improvements of shoulder ROM and function which reflected on patients’ QoL and ADL, so emphasis on strengthening exercises during rehabilitation can be of great benefit in AC treatment.
Data Availability
The data sets generated during and/or analyzed during the current study are available within the manuscript.
Abbreviations
- QoL:
-
Quality of life
- AC:
-
Adhesive capsulitis
- ROM:
-
Range of motion
- VAS:
-
Visual analogue scale
- DASH:
-
The Disability of the Arm, Shoulder, and Hand questionnaire
- SF-36:
-
Short-form
References
Oliveira M, Gurgel M, Miranda M, Okubo M, Feijó L, Souza G (2009) Efficacy of shoulder exercises on locoregional complications in women undergoing radiotherapy for breast cancer: clinical trial. Braz J Phys Ther 13(2):136–143
Blomqvist L, Stark B, Engler N, Malm M (2004) Evaluation of arm and shoulder mobility and strength after modified radical mastectomy and radiotherapy. Acta Oncol 43(3):280–283
Dilaveri CA, Sandhu NP, Neal L, Neben-Wittich MA, Hieken TJ, Mac Bride MB et al (2014) Medical factors influencing decision making regarding radiation therapy for breast cancer. Int J Women’s Health 6:945–951
Nesvold IL, Fossa SD, Holm I, Naume B, Dahl AA (2010) Arm/shoulder problems in breast cancer survivors are associated with reduced health and poorer physical quality of life. Acta Oncol 49:347–353
Neviaser AS, Hannafin JA (2010) Adhesive capsulitis: a review of current treatment. Am J Sports Med 38(11):2346–2356
Prestgaard TA (n.d.) Frozen shoulder (adhesive capsulitis). In: UpToDate [online]. Available at: https://www.uptodate.com/contents/frozen-shoulder-adhesive-capsulitis. Accessed 1 Nov 2017
Dias R, Cutts S, Massoud S (2005) Frozen shoulder. BMJ 331(7530):1453–1456
Leung MS, Cheing GL (2008) Effects of deep and superficial heating in the management of frozen shoulder. J Rehabil Med 40:145–150
Cheing GL, So EM, Chao CY (2008) Effectiveness of electroacupuncture and interferential eloctrotherapy in the management of frozen shoulder. J Rehabil Med 40:166–170
Ma T, Kao MJ, Lin IH, Chiu YL, Chien C, Ho TJ et al (2006) A study on the clinical effects of physical therapy and acupuncture to treat spontaneous frozen shoulder. Am J Chin Med 34:759–775
Stergioulas A (2008) Low-power laser treatment in patients with frozen shoulder: preliminary results. Photomed Laser Surg 26:99–105
Kelley MJ, McClure PW, Leggin BG (2009) Frozen shoulder: evidence and a proposed model guiding rehabilitation. J Orthop Sports Phys Ther 39:135–148
Hanchard NCA, Goodchild LM, Thompson J, O’Brien T, Davison D, Richardson C (2012) Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy 98(2):117–120
Santos WD, Gentil P, de Moraes RF, Júnior JB, Campos MH, Lira CA et al (2017) Chronic effects of resistance training in breast cancer survivors. Biomed Res Int 2017:8367803
Mayer F, Scharhag-Rosenberger F, Carlsohn A, Cassel M, Muller S, Scharhag J (2011) The intensity and effects of strength training in the elderly. DeutschesArzteblatt Int 108(21):359
Cho J, Lee K, Kim M, Hahn J, Lee W (2018) The effects of double oscillation exercise combined with elastic band exercise on scapular stabilizing muscle strength and thickness in healthy young individuals: a randomized controlled pilot trial. J Sports Sci Med 17:7–16
Lins C, Castro A, Medina GIS, Azevedo E, Donato BS, Chagas MSS et al (2019) Alternative scapular stabilization exercises to target strength, endurance and function of shoulders in tetraplegia: a prospective non-controlled intervention study. J Spinal Cord Med 42:65–76
Yoo IG, Yoo WG (2013) The effect of a new neck support tying method using thera-band on cervical rom and shoulder muscle pain after overhead work. J Phys Ther Sci 25:843–844
BasKurt Z, BasKurt F, Gelecek N, Ozkan MH (2011) The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil 24(3):173–179
Cheville AL, Tchou J (2007) Barriers to rehabilitation following surgery for primary breast cancer. J Surg Oncol 95:409–418
Harishkumar S, Kiruthika S, Arunachalam R, Kumerasan A (2017) To analyse the effect of theraband strengthening with conventional exercise on pain, function & range of motion in patients with adhesive capsulitis. Int J Pharma Bio Sci 8(4):214–227
Rawat P, Eapen C, Seema KP (2017) Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: a randomized controlled trial. J Hand Ther 30:235–241
Datar NA, Devi TP (2019) Effect of graded thera-band exercises on shoulder muscle strength and activities of daily life in modified radical mastectomy subjects. Biomed Pharmacol J 12(3):1345–1351
Kirthika SV, Bhavani PB, Rajlakshmi V (2015) Effect of combining scapular stabilization techniques with conventional physiotherapy in improving range of motion and functional ability in subjects with phase II adhesive capsulitis of the shoulder joint. J Physiother Occup Ther 1(1):25–34
Gulwani AH (2020) A study to find out the effect of scapular stabilization exercises on shoulder ROM and functional outcome in diabetic patients with stage 2 adhesive capsulitis of the shoulder joint: an interventional study. Int J Sci Healthc Res 5(2):320–333
Sabari JS, Maltzev I, Lubarsky D, Liszkay E, Homel P (1998) Goniometric assessment of shoulder range of motion: comparison of testing in supine and sitting positions. Arch Phys Med Rehabil 79(6):647–651. https://doi.org/10.1016/S0003-9993(98)90038-7
Riddle DL, Rothstein JM, Lamb RL (1987) Goniometric reliability in a clinical setting. Shoulder measurements. Phys Ther 67:668
Roy JS, MacDermid JC, Orton B, Tran T, Faber KJ, Drosdowech D, Athwal GS (2009) The concurrent validity of a hand-held versus a stationary dynamometer in testing isometric shoulder strength. J Hand Ther 22(4):320–327
Alotaibi NM, Aljadi SH, Alrowayeh HN (2016) Reliability, validity and responsiveness of the Arabic version of the disability of arm, shoulder and hand (DASH-Arabic). Disabil Rehabil 38(25):2469–2478. https://doi.org/10.3109/09638288.2015.1136846
Boonstra AM, Preuper HRS, Reneman MF, Posthumus JB, Stewart RE (2008) Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 31(2):165–169
Guermazi M, Allouch C, Yahia M, Huissa TB, Ghorbel S, Damak J, Mrad MF, Elleuch MH (2012) Translation in Arabic, adaptation and validation of the SF-36 health survey for use in Tunisia. Ann Phys Rehabil Med 55(6):388–403
Page P, Labbe A (2010) Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther 5(4):266–273
Çelik D, Mutlu EK (2016) Does adding mobilization to stretching improve outcomes for people with frozen shoulder? A randomized controlled clinical trial. Clin Rehabil 30(8):786–794
Russell S, Jariwala A, Conlon R, Selfe J, Richards J, Walton M (2014) A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J Shoulder Elbow Surg 23(4):500–507
Dempsey AL, Mills T, Karsch RM, Branch TP (2011) Maximizing total end range time is safe and effective for the conservative treatment of frozen shoulder patients. Am J Phys Med Rehabil 90(9):738–745
Favejee MM, Huisstede BM, Koes BW (2011) Frozen shoulder: the effectiveness of conservative and surgical interventions–systematic review. Br J Sports Med 45(1):49–56
Kim KH, Yeo SM, Cheong IY, Kim Y, Jeon BJ, Hwang JH (2019) Early rehabilitation after total mastectomy and immediate reconstruction with tissue expander insertion in breast cancer patients: a retrospective case-control study. J Breast Cancer 22(3):472–483
Leonidou A, Woods DA (2014) A preliminary study of manipulation under anaesthesia for secondary frozen shoulder following breast cancer treatment. Ann R Coll Surg Engl 96:111–115
Chan HBY, Pua PY, How CH (2017) Physical therapy in the management of frozen shoulder. Singapore Med J 58(12):685–689
Ruivo RM, Donatelli R, Parraca JA (2017) A specific multi-approach intervention for adhesive capsulitis: a case page 3 of 7 report. J Excer Sports Orthop 4(3):1–7
Ok SJ (2016) Effects of resistance exercise using elastic band on range of motion, function and shoulder pain among patients with rotator cuff repair. Korean J Adult Nursing 28(5):491–500
Zhu P, Liao B, Wang Z, Sun Z, Yang W, Cai Y (2021) Resistance band training after triamcinolone acetonide injection for subacromial bursitis: a randomized clinical trial. J Rehabil Med 53(1):jrm00140
Hedayatpour N, Falla D (2015) Physiological and neural adaptations to eccentric exercise: mechanisms and considerations for training. Biomed Res Int 2015:193741
Shamley D, Srinaganathan R, Oskrochi R, Lascurain-Aguirrebeña I, Sugden E (2009) Three-dimensional scapulothoracic motion following treatment for breast cancer. Breast Cancer Res Treat 118:315–322
Crosbie J, Kilbreath SL, Dylke E, Refshauge KM, Nicholson LL, Beith JM et al (2010) Effects of mastectomy on shoulder and spinal kinematics during bilateral upper-limb movement. Phys Ther 90(5):679–691
Yatheendra kG, Sudhakar S, yashvanth A, Siva JN (2015) Effect of high-grade mobilisation techniques and scapular stabilization exercises in frozen shoulder. Int J Phys Educ Sports Health 2(1):80–83
Voight ML, Thomson BC (2000) The role of the scapula in the rehabilitation of shoulder injuries. J Athl Train 35(3):364–437
Song MJ, Kang TW (2021) The effect of a four-week scapular stabilization exercise program using PNF technique on scapular symmetry and range of flexion motion, pain, function, and quality of life in post-mastectomy women with breast cancer. PNF Mov 19(1):19–29
Nam S, Kang T (2017) Effect of scapular stabilization exercise on shoulder joint range of motion, pain and functional level in women who underwent breast cancer resection. Korean J Orthop Phys Ther 23(2):69–74
Serra-Añó P, Pellicer-Chenoll M, García-Massó X, Morales J, Giner-Pascual M, González LM (2012) Effects of resistance training on strength, pain and shoulder functionality in paraplegics. Spinal Cord 50:827–831
Acknowledgements
We are grateful to our patients for taking part in this study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Nancy H. Aboelnour, Fatma Alzahraa H. Kamel, and Noha M. Kamel. The first draft of the manuscript was written by Nancy H. Aboelnour, Fatma Alzahraa H. Kamel, Maged A. Basha, Alshimaa R. Azab, Islam M. Hewidy, Mohamed Ezzat, and Noha M. Kamel. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All study procedures were conducted in line with the rules and principles of the Declaration of Helsinki of the World Medical Association. The study was approved by the Research Ethics Committee of Physical Therapy Faculty in Cairo University. This trial was registered in ClinicalTrials.gov (ID: NCT05311839).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The participants gave consent for publication of de-identified information through informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aboelnour, N.H., Kamel, F.H., Basha, M.A. et al. Combined effect of graded Thera-Band and scapular stabilization exercises on shoulder adhesive capsulitis post-mastectomy. Support Care Cancer 31, 215 (2023). https://doi.org/10.1007/s00520-023-07641-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07641-6