Abstract
Objectives
To discuss the effects of physical activity on cancer-related fatigue (CRF) in lung cancer patients, summarize the types of physical activity in the published reviews, assess the quality of the evidence, and provide suggestions for the clinical selection of exercise intervention.
Methods
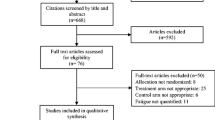
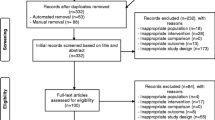
PubMed, EMBASE, Web of Science, and the Cochrane Database of Systematic Reviews were searched through 8 November 2021 to identify relevant systematic reviews and meta-analyses. We also performed a manual search of the reference lists of included articles as supplements. Two researchers independently performed literature screening, data extraction, and quality assessment. The umbrella review has been registered in the International Prospective Register of Systematic Review (PROSPERO) registry (CRD42021292548).
Results
From the 13 systematic reviews or meta-analyses identified, 10 physical activity interventions were included. The most mentioned intervention was aerobic combined with resistance exercise; however, no reduction of the symptoms of CRF was observed in lung cancer patients by this exercise intervention. Most of the patients who performed aerobic exercises alone showed improvement in CRF after the intervention. In addition, Tai Chi and breathing exercises have been shown to improve fatigue, but more high-quality research is still needed to support its effectiveness.
Conclusions
Aerobic exercise, respiratory muscle training, aerobic combined with balance training, and other exercise interventions have been shown to improve CRF in lung cancer patients. But it should be noted that according to the different treatment methods and disease stages of patients, individualized rehabilitation programs should be developed for patients. Due to the low methodological quality and evidence quality of some systematic reviews and meta-analyses included in this study, more high-quality clinical studies and systematic reviews are still needed for validation in the future. This umbrella review helps to identify effective ways of exercise to improve fatigue in lung cancer patients before dedicated evidence-based medical guidelines are established.



Similar content being viewed by others
Data Availability
Data will be available upon request for the purposes of data transparency.
Abbreviations
- CRF:
-
Cancer-Related Fatigue
- ACSM:
-
American College of Sports Medicine
- PROSPERO:
-
International Prospective Register of Systematic Review
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MeSH:
-
Medical Subject Headings
- AMSTAR:
-
A MeaSurement Tool to Assess Systematic Reviews
- GRADE:
-
Grading of Recommendations Assessment, Development, and Evaluation
- CERQual:
-
Confidence in the Evidence from Reviews of Qualitative research
- RCT:
-
Randomized Control Trial
- HIIT:
-
High Intensity Interval Training
- BFI:
-
Brief Fatigue Inventory
- FACT-F:
-
Functional Assessment of Cancer Therapy-Fatigue
- MFI-20:
-
Multidimensional Fatigue Inventory with 20 questions
- FACT-L:
-
Functional Assessment of Cancer Therapy-Lung
- VAS-F:
-
Visual Analogue Scale-Fatigue
- EORTC-QLQ-C30:
-
European organization for Research and Treatment of Cancer-Quality of Life Questionnaire C30
- FACIT-F:
-
Functional Assessment of Chronic Illness Therapy-Fatigue
- CRDQ:
-
Chronic Respiratory Disease Questionnaire
- MFSI-SF:
-
Multidimensional Fatigue Symptom Inventory- Short Form
- NR:
-
Not Reported
- CI:
-
Confidence Interval
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Lu T, Yang X, Huang Y, Zhao M, Li M, Ma K, Yin J, Zhan C, Wang Q (2019) Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag Res 11:943–953. https://doi.org/10.2147/cmar.S187317
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics, 2021. CA Cancer J Clin 71:7–33. https://doi.org/10.3322/caac.21654
Natioinal Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Cancer-related fatigue. Version 2.2022. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf
Jung JY, Lee JM, Kim MS, Shim YM, Zo JI, Yun YH (2018) Comparison of fatigue, depression, and anxiety as factors affecting posttreatment health-related quality of life in lung cancer survivors. Psychooncology 27:465–470. https://doi.org/10.1002/pon.4513
Huang X, Zhou W, Zhang Y (2015) Features of fatigue in patients with early-stage non-small cell lung cancer. J Res Med Sci 20:268–272
Sarna L, Cooley ME, Brown JK, Chernecky C, Elashoff D, Kotlerman J (2008) Symptom severity 1 to 4 months after thoracotomy for lung cancer. Am J Crit Care 17:455–467
Nowicki A, Piekarska J, Farbicka E (2017) The assessment of cancer-related fatigue syndrome in patients with lung cancer during palliative chemotherapy. Adv Respir Med 85:69–76. https://doi.org/10.5603/arm.2017.0013
Mustian KM, Alfano CM, Heckler C, Kleckner AS, Kleckner IR, Leach CR, Mohr D, Palesh OG, Peppone LJ, Piper BF, Scarpato J, Smith T, Sprod LK, Miller SM (2017) Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA oncol 3:961–968. https://doi.org/10.1001/jamaoncol.2016.6914
Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51:2375–2390. https://doi.org/10.1249/mss.0000000000002116
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377:108–109. https://doi.org/10.1016/s0140-6736(10)60903-8
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Langer G, Meerpohl JJ, Perleth M, Gartlehner G, Kaminski-Hartenthaler A, Schunemann H (2012) GRADE guidelines: 1. Introduction - GRADE evidence profiles and summary of findings tables. Z Evid Fortbild Qual Gesundhwes 106:357–368. https://doi.org/10.1016/j.zefq.2012.05.017
Cavalheri V, Burtin C, Formico VR, Nonoyama ML, Jenkins S, Spruit MA, Hill K (2019) Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database of Syst Rev. https://doi.org/10.1002/14651858.CD009955.pub3
Chen YJ, Li XX, Ma HK, Zhang X, Wang BW, Guo TT, Xiao Y, Bing ZT, Ge L, Yang KH, Han XM (2020) Exercise training for improving patient-reported outcomes in patients with advanced-stage cancer: a systematic review and meta-analysis. J Pain Symptom Manage 59:734. https://doi.org/10.1016/j.jpainsymman.2019.09.010
Codima A, Silva WD, Borges APD, de Castro G (2021) Exercise prescription for symptoms and quality of life improvements in lung cancer patients: a systematic review. Supportive Care in Cancer 29:445–457. https://doi.org/10.1007/s00520-020-05499-6
Crandall K, Maguire R, Campbell A, Kearney N (2014) Exercise intervention for patients surgically treated for non-small cell lung cancer (NSCLC): a systematic review. Surg Oncol 23:17–30. https://doi.org/10.1016/j.suronc.2014.01.001
Dittus KL, Gramling RE, Ades PA (2017) Exercise interventions for individuals with advanced cancer: a systematic review. Prev Med 104:124–132. https://doi.org/10.1016/j.ypmed.2017.07.015
Henshall CL, Allin L, Aveyard H (2019) A systematic review and narrative synthesis to explore the effectiveness of exercise-based interventions in improving fatigue, dyspnea, and depression in lung cancer survivors. Cancer Nurs 42:295–306. https://doi.org/10.1097/ncc.0000000000000605
Heywood R, McCarthy AL, Skinner TL (2018) Efficacy of exercise interventions in patients with advanced cancer: a systematic review. Arch Phys M 99:2595–2620. https://doi.org/10.1016/j.apmr.2018.04.008
Machado P, Pimenta S, Oliveiros B, Ferreira JP, Martins RA, Cruz J (2021) Effect of exercise training on quality of life after colorectal and lung cancer surgery: a meta-analysis. Cancers 13. https://doi.org/10.3390/cancers13194975
Paramanandam VS, Dunn V (2015) Exercise for the management of cancer-related fatigue in lung cancer: a systematic review. Eur J Cancer 24:4–14. https://doi.org/10.1111/ecc.12198
Peddle-McIntyre CJ, Singh F, Thomas R, Newton RU, Galvão DA, Cavalheri V (2019) Exercise training for advanced lung cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012685.pub2
Song SJ, Yu JH, Ruan Y, Liu X, Xiu LJ, Yue XQ (2018) Ameliorative effects of Tai Chi on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support Cancer Ther 26:2091–2102. https://doi.org/10.1007/s00520-018-4136-y
Yang M, Liu L, Gan CE, Qiu LH, Jiang XJ, He XT, Zhang JE (2020) Effects of home-based exercise on exercise capacity, symptoms, and quality of life in patients with lung cancer: a meta-analysis. Eur J Oncol Nurs 49:101836. https://doi.org/10.1016/j.ejon.2020.101836
Zhou L, Chen Q, Zhang J (2021) Effect of exercise on fatigue in patients with lung cancer: a systematic review and meta-analysis of randomized trials. J Palliat Med 24:932–943. https://doi.org/10.1089/jpm.2020.0504
Janssen SM, Abbink JJ, Lindeboom R, Vliet Vlieland TP (2017) Outcomes of pulmonary rehabilitation after treatment for non-small cell lung cancer stages I to IIIa: an observational study. J Cardiopulm Rehabil Prev 37:65–71. https://doi.org/10.1097/hcr.0000000000000227
Litterini AJ, Jette DU (2011) Exercise for managing cancer-related fatigue. Phys Ther 91:301–304. https://doi.org/10.2522/ptj.20100273
Jones LW, Eves ND, Peterson BL, Garst J, Crawford J, West MJ, Mabe S, Harpole D, Kraus WE, Douglas PS (2008) Safety and feasibility of aerobic training on cardiopulmonary function and quality of life in postsurgical nonsmall cell lung cancer patients: a pilot study. Cancer 113:3430–3439. https://doi.org/10.1002/cncr.23967
Riesenberg H, Lübbe AS (2010) In-patient rehabilitation of lung cancer patients–a prospective study. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 18:877–882. https://doi.org/10.1007/s00520-009-0727-y
Andersen AH, Vinther A, Poulsen LL, Mellemgaard A (2011) Do patients with lung cancer benefit from physical exercise? Acta Oncol 50:307–313. https://doi.org/10.3109/0284186x.2010.529461
Hwang CL, Yu CJ, Shih JY, Yang PC, Wu YT (2012) Effects of exercise training on exercise capacity in patients with non-small cell lung cancer receiving targeted therapy. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 20:3169–3177. https://doi.org/10.1007/s00520-012-1452-5
Egegaard T, Rohold J, Lillelund C, Persson G, Quist M (2019) Pre-radiotherapy daily exercise training in non-small cell lung cancer: a feasibility study. Rep Pract Oncol Radiother 24:375–382. https://doi.org/10.1016/j.rpor.2019.06.003
Peddle CJ, Jones LW, Eves ND, Reiman T, Sellar CM, Winton T, Courneya KS (2009) Effects of presurgical exercise training on quality of life in patients undergoing lung resection for suspected malignancy: a pilot study. Cancer Nurs 32:158–165. https://doi.org/10.1097/NCC.0b013e3181982ca1
Dhillon HM, Bell ML, van der Ploeg HP, Turner JD, Kabourakis M, Spencer L, Lewis C, Hui R, Blinman P, Clarke SJ, Boyer MJ, Vardy JL (2017) Impact of physical activity on fatigue and quality of life in people with advanced lung cancer: a randomized controlled trial. Ann Oncol 28:1889–1897. https://doi.org/10.1093/annonc/mdx205
Peddle-McIntyre CJ, Bell G, Fenton D, McCargar L, Courneya KS (2012) Feasibility and preliminary efficacy of progressive resistance exercise training in lung cancer survivors. Lung Cancer 75:126–132. https://doi.org/10.1016/j.lungcan.2011.05.026
Spruit MA, Janssen PP, Willemsen SC, Hochstenbag MM, Wouters EF (2006) Exercise capacity before and after an 8-week multidisciplinary inpatient rehabilitation program in lung cancer patients: a pilot study. Lung Cancer 52:257–260. https://doi.org/10.1016/j.lungcan.2006.01.003
Temel JS, Greer JA, Goldberg S, Vogel PD, Sullivan M, Pirl WF, Lynch TJ, Christiani DC, Smith MR (2009) A structured exercise program for patients with advanced non-small cell lung cancer. J Thorac Oncol 4:595–601. https://doi.org/10.1097/JTO.0b013e31819d18e5
Quist M, Rørth M, Langer S, Jones LW, Laursen JH, Pappot H, Christensen KB, Adamsen L (2012) Safety and feasibility of a combined exercise intervention for inoperable lung cancer patients undergoing chemotherapy: a pilot study. Lung Cancer 75:203–208. https://doi.org/10.1016/j.lungcan.2011.07.006
Coats V, Maltais F, Simard S, Fréchette E, Tremblay L, Ribeiro F, Saey D (2013) Feasibility and effectiveness of a home-based exercise training program before lung resection surgery. Can Respir J 20:e10-16. https://doi.org/10.1155/2013/291059
Salhi B, Haenebalcke C, Perez-Bogerd S, Nguyen MD, Ninane V, Malfait TL, Vermaelen KY, Surmont VF, Van Maele G, Colman R, Derom E, van Meerbeeck JP (2015) Rehabilitation in patients with radically treated respiratory cancer: a randomised controlled trial comparing two training modalities. Lung Cancer 89:167–174. https://doi.org/10.1016/j.lungcan.2015.05.013
Cavalheri V, Jenkins S, Cecins N, Gain K, Phillips MJ, Sanders LH, Hill K (2017) Exercise training for people following curative intent treatment for non-small cell lung cancer: a randomized controlled trial. Braz J Phys Ther 21:58–68. https://doi.org/10.1016/j.bjpt.2016.12.005
Granger CL, Irving L, Antippa P, Edbrooke L, Parry SM, Krishnasamy M, Denehy L (2018) CAPACITY: a physical activity self-management program for patients undergoing surgery for lung cancer, a phase I feasibility study. Lung Cancer 124:102–109. https://doi.org/10.1016/j.lungcan.2018.07.034
Ozalevli S, Ilgin D, Kul Karaali H, Bulac S, Akkoclu A (2010) The effect of in-patient chest physiotherapy in lung cancer patients. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 18:351–358. https://doi.org/10.1007/s00520-009-0659-6
Hoffman AJ, Brintnall RA, Brown JK, Eye A, Jones LW, Alderink G, Ritz-Holland D, Enter M, Patzelt LH, Vanotteren GM (2013) Too sick not to exercise: using a 6-week, home-based exercise intervention for cancer-related fatigue self-management for postsurgical non-small cell lung cancer patients. Cancer Nurs 36:175–188. https://doi.org/10.1097/NCC.0b013e31826c7763
Hoffman AJ, Brintnall RA, Brown JK, von Eye A, Jones LW, Alderink G, Ritz-Holland D, Enter M, Patzelt LH, VanOtteren GM (2014) Virtual reality bringing a new reality to postthoracotomy lung cancer patients via a home-based exercise intervention targeting fatigue while undergoing adjuvant treatment. Cancer Nurs 37:23–33. https://doi.org/10.1097/NCC.0b013e318278d52f
Hoffman AJ, Brintnall RA, Given BA, von Eye A, Jones LW, Brown JK (2017) Using perceived self-efficacy to improve fatigue and fatigability in postsurgical lung cancer patients: a pilot randomized controlled trial. Cancer Nurs 40:1–12. https://doi.org/10.1097/ncc.0000000000000378
Henke CC, Cabri J, Fricke L, Pankow W, Kandilakis G, Feyer PC, de Wit M (2014) Strength and endurance training in the treatment of lung cancer patients in stages IIIA/IIIB/IV. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 22:95–101. https://doi.org/10.1007/s00520-013-1925-1
Messaggi-Sartor M, Marco E, Martinez-Tellez E, Rodriguez-Fuster A, Palomares C, Chiarella S, Muniesa JM, Orozco-Levi M, Barreiro E, Guell MR (2019) Combined aerobic exercise and high-intensity respiratory muscle training in patients surgically treated for non-small cell lung cancer: a pilot randomized clinical trial. Eur J Phys Rehabil Med 55:113–122. https://doi.org/10.23736/S1973-9087.18.05156-0
Kuehr L, Wiskemann J, Abel U, Ulrich CM, Hummler S, Thomas M (2014) Exercise in patients with non-small cell lung cancer. Med Sci Sports Exer 46:656–663. https://doi.org/10.1249/MSS.0000000000000158
Molassiotis A, Charalambous A, Taylor P, Stamataki Z, Summers Y (2015) The effect of resistance inspiratory muscle training in the management of breathlessness in patients with thoracic malignancies: a feasibility randomised trial. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 23:1637–1645. https://doi.org/10.1007/s00520-014-2511-x
Zhang LL, Wang SZ, Chen HL, Yuan AZ (2016) Tai Chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage 51:504–511. https://doi.org/10.1016/j.jpainsymman.2015.11.020
Jiang MY, Wang M, Song CA (2013) Influence of shadowboxing on improving cancer-related fatigue and sleeping quality of patients with advanced lung cancer. Chinese Nurs Res 27:420–421
Quist M, Sommer MS, Vibe-Petersen J, Stærkind MB, Langer SW, Larsen KR, Trier K, Christensen M, Clementsen PF, Missel M, Henriksen C, Christensen KB, Lillelund C, Langberg H, Pedersen JH (2018) Early initiated postoperative rehabilitation reduces fatigue in patients with operable lung cancer: a randomized trial. Lung Cancer 126:125–132. https://doi.org/10.1016/j.lungcan.2018.10.025
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P (2015) Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 13:132–140. https://doi.org/10.1097/xeb.0000000000000055
Capozzi LC, Daun JT, Ester M, Mosca S, Langelier D, Francis GJ, Chang E, Mina DS, Fu JB, Culos-Reed SN (2021) Physical activity for individuals living with advanced cancer: evidence and recommendations. Semin Oncol Nurs 37:151170. https://doi.org/10.1016/j.soncn.2021.151170
Carli F, Ferreira V (2018) Prehabilitation: a new area of integration between geriatricians, anesthesiologists, and exercise therapists. Aging Clin Exp Res 30:241–244. https://doi.org/10.1007/s40520-017-0875-8
Vagvolgyi A, Rozgonyi Z, Kerti M, Vadasz P, Varga J (2017) Effectiveness of perioperative pulmonary rehabilitation in thoracic surgery. J Thorac Dis 9:1584–1591. https://doi.org/10.21037/jtd.2017.05.49
Peddle CJ, Jones LW, Eves ND, Reiman T, Sellar CM, Winton T, Courneya KS (2009) Effects of presurgical exercise training on quality of life in patients undergoing lung resection for suspected malignancy: a pilot study. Cancer Nurs 32:158–165. https://doi.org/10.1097/NCC.0b013e3181982ca1
Fagundes CP, Shi Q, Vaporciyan AA, Rice DC, Popat KU, Cleeland CS, Wang XS (2015) Symptom recovery after thoracic surgery: measuring patient-reported outcomes with the MD Anderson Symptom Inventory. J Thorac Cardiovasc 150:613–619.e612. https://doi.org/10.1016/j.jtcvs.2015.05.057
Hoffman AJ, Brintnall RA, Given BA, von Eye A, Jones LW, Brown JK (2017) Using perceived self-efficacy to improve fatigue and fatigability in postsurgical lung cancer patients: a pilot randomized controlled trial. Cancer Nurs 40:1–12. https://doi.org/10.1097/ncc.0000000000000378
Bower JE (2014) Cancer-related fatigue – mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 11:597–609. https://doi.org/10.1038/nrclinonc.2014.127
Endo Y, Nourmahnad A, Sinha I (2020) Optimizing skeletal muscle anabolic response to resistance training in aging. Front Physiol 11:874. https://doi.org/10.3389/fphys.2020.00874
McKendry J, Stokes T, McLeod JC, Phillips SM (2021) Resistance exercise, aging, disuse, and muscle protein metabolism. Compr Physiol 11:2249–2278. https://doi.org/10.1002/cphy.c200029
Schmidt ME, Wiskemann J, Armbrust P, Schneeweiss A, Ulrich CM, Steindorf K (2015) Effects of resistance exercise on fatigue and quality of life in breast cancer patients undergoing adjuvant chemotherapy: a randomized controlled trial. Int J Cancer 137:471–480. https://doi.org/10.1002/ijc.29383
Steindorf K, Schmidt ME, Klassen O, Ulrich CM, Oelmann J, Habermann N, Beckhove P, Owen R, Debus J, Wiskemann J, Potthoff K (2014) Randomized, controlled trial of resistance training in breast cancer patients receiving adjuvant radiotherapy: results on cancer-related fatigue and quality of life. Ann Oncol 25:2237–2243. https://doi.org/10.1093/annonc/mdu374
Dieli-Conwright CM, Courneya KS, Demark-Wahnefried W, Sami N, Lee K, Sweeney FC, Stewart C, Buchanan TA, Spicer D, Tripathy D, Bernstein L, Mortimer JE (2018) Aerobic and resistance exercise improves physical fitness, bone health, and quality of life in overweight and obese breast cancer survivors: a randomized controlled trial. J Breast Cancer 20:124. https://doi.org/10.1186/s13058-018-1051-6
Yang L, Winters-Stone K, Rana B, Cao C, Carlson LE, Courneya KS, Friedenreich CM, Schmitz KH (2021) Tai Chi for cancer survivors: a systematic review toward consensus-based guidelines. Cancer Med 10:7447–7456. https://doi.org/10.1002/cam4.4273
Cheung DST, Takemura N, Lam TC, Ho JCM, Deng W, Smith R, Yan Y, Lee AWM, Lin CC (2021) Feasibility of aerobic exercise and Tai-Chi interventions in advanced lung cancer patients: a randomized controlled trial. Integr Cancer Ther 20:15347354211033352. https://doi.org/10.1177/15347354211033352
Wang F, Lee EK, Wu T, Benson H, Fricchione G, Wang W, Yeung AS (2014) The effects of Tai Chi on depression, anxiety, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med 21:605–617. https://doi.org/10.1007/s12529-013-9351-9
Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, Song R (2018) Tai Chi and qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv 12:256–267. https://doi.org/10.1007/s11764-017-0665-5
Zeng Y, Luo T, Xie H, Huang M, Cheng AS (2014) Health benefits of qigong or Tai Chi for cancer patients: a systematic review and meta-analyses. Complementary therapies in medicine 22:173–186. https://doi.org/10.1016/j.ctim.2013.11.010
Hilfiker R, Meichtry A, Eicher M, Nilsson Balfe L, Knols RH, Verra ML, Taeymans J (2018) Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med 52:651–658. https://doi.org/10.1136/bjsports-2016-096422
Marzorati C, Monzani D, Mazzocco K, Pavan F, Monturano M, Pravettoni G (2019) Dimensionality and measurement invariance of the Italian version of the EORTC QLQ-C30 in postoperative lung cancer patients. Frontiers in psychology 10:2147. https://doi.org/10.3389/fpsyg.2019.02147
Shahid A, Wilkinson K, Marcu S, Shapiro CM (2011) Brief fatigue inventory. In: STOP, THAT and One Hundred Other Sleep Scales. Springer, New York, NY, pp 75–77. https://doi.org/10.1007/978-1-4419-9893-4_11
Storey DJ, Waters RA, Hibberd CJ, Rush RW, Cargill AT, Wall LR, Fallon MT, Strong VA, Walker J, Sharpe M (2007) Clinically relevant fatigue in cancer outpatients: the Edinburgh Cancer Centre symptom study. Ann Oncol 18:1861–1869. https://doi.org/10.1093/annonc/mdm349
Shahid A, Wilkinson K, Marcu S, Shapiro CM (2011) Multidimensional Fatigue Inventory (MFI). In: STOP, THAT and One Hundred Other Sleep Scales. Springer, New York, NY, pp 241–243. https://doi.org/10.1007/978-1-4419-9893-4_57
Minton O, Stone P (2009) A systematic review of the scales used for the measurement of cancer-related fatigue (CRF). Ann Oncol 20:17–25. https://doi.org/10.1093/annonc/mdn537
Saito H, Shiraishi A, Nomori H, Matsui H, Yoshida K, Matsue Y, Fujii T, Kawama K (2020) Impact of age on the recovery of six-minute walking distance after lung cancer surgery: a retrospective cohort study. Gen Thorac Cardiovasc Surg 68:150–157. https://doi.org/10.1007/s11748-019-01191-7
Fusar-Poli P, Radua J (2018) Ten simple rules for conducting umbrella reviews. Evid Based Ment Health 21:95–100. https://doi.org/10.1136/ebmental-2018-300014
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. The authors’ responsibilities were as follows—Yi Zhu, Weiqian Hou: study design; Weiqian Hou, Liwen Zhai, Yao Yang: literature search and literature screening; Weiqian Hou, Liwen Zhai: data extraction; Weiqian Hou, Liwen Zhai, Conghui Li, Yao Yang: assessment of quality and data synthesis; Weiqian Hou, Liwen Zhai: drafting of the manuscript; Yi Zhu, Yujie Yang, Shanshan Gu: revision of the manuscript; Yi Zhu: supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study is an umbrella review of published material; therefore, ethics approval was not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Weiqian Hou and Liwen Zhai are the co-first authors.
Supplementary information
ESM 1
(DOCX 818 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hou, W., Zhai, L., Yang, Y. et al. Is physical activity effective against cancer-related fatigue in lung cancer patients? An umbrella review of systematic reviews and meta-analyses. Support Care Cancer 31, 161 (2023). https://doi.org/10.1007/s00520-023-07627-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07627-4