Abstract
Purpose
The present study investigated whether the level of cancer-related fatigue (CRF) after finishing oncology treatment was related to higher levels of persistent CRF and its relationship with both functional and psychological disturbances. Second, to identify potential predictors of persistent CRF.
Methods
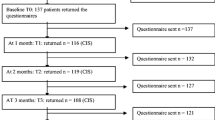
Eighty BC survivors were classified into non-fatigued (≤ 3.9) or fatigued (≥ 4), according to their Piper Fatigue Scale total score after finishing oncology treatment. The time course of fatigue and the impact on its domains, pain, mood state, perceived physical fitness, the level of physical activity, and quality of life were assessed at ≥ 5 years.
Results
Women classified as fatigued after finishing oncology treatment had not only a higher prevalence of persistent CRF (41.2%) at the reassessment, but also greater levels of pain (P = .006 to .048) and mood disturbances (P = .007 to .015), and lower levels of physical fitness condition (P = .002 to .039) and quality of life (P < .001 to < .05) over time. Regression analyses revealed that “sadness/depression,” “global health status,” “physical activity level,” and “type of treatment” were significant predictors of persistent CRF (r2 = .692).
Conclusion
Higher levels of CRF implied greater levels of persistent CRF and a lower functional and psychological profile over time. 69.2% of of persistent CRF was explained.




Similar content being viewed by others
Data availability
All authors certify that they have no affiliations or involvement with any organization or entity with financial or nonfinancial interests in the subject matter or materials discussed in this manuscript.
Code availability
N/A.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Gernier F, Joly F, Klein D, Mercier M, Velten M, Licaj I (2020) Cancer-related fatigue among long-term survivors of breast, cervical, and colorectal cancer: a French registry-based controlled study. Support Care Cancer 28:5839–5849
Moshina N, Falk RS, Hofvind S (2021) Long-term quality of life among breast cancer survivors eligible for screening at diagnosis: a systematic review and meta-analysis. Public Health 199:65–76
Mellblom AV, Kiserud CE, Rueegg CS, Ruud E, Loge JH, Fosså SD, Lie HC (2021) Self-reported late effects and long-term follow-up care among 1889 long-term Norwegian childhood, adolescent, and young adult cancer survivors (the NOR-CAYACS study). Support Care Cancer 29:2947–2957
Bower JE, Lamkin DM (2013) Inflammation and cancer-related fatigue: mechanisms, contributing factors, and treatment implications. Brain Behav Immun 30(Suppl):S48-57
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, Cleeland C, Dotan E, Eisenberger MA, Escalante CP et al (2015) Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw 13:1012–1039
Savina S, Zaydiner B (2019) Cancer-related fatigue: some clinical aspects. Asia Pac J Oncol Nurs 6:7–9
Cella D, Davis K, Breitbart W, Curt G (2001) Fatigue Coalition. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol. 19:3385–3391
Bower JE, Ganz PA, Desmond KA, Bernaards C, Rowland JH, Meyerowitz BE, Belin TR (2006) Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer 106:751–758
Schmidt ME, Chang-Claude J, Seibold P, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K (2015) Determinants of long-term fatigue in breast cancer survivors: results of a prospective patient cohort study: determinants of long-term fatigue in breast cancer survivors. Psychooncology 24:40–46
Huang X, Zhang Q, Kang X, Song Y, Zhao W (2010) Factors associated with cancer-related fatigue in breast cancer patients undergoing endocrine therapy in an urban setting: a cross-sectional study. BMC Cancer 10:453
Reinertsen KV, Cvancarova M, Loge JH, Edvardsen H, Wist E, Fosså SD (2010) Predictors and course of chronic fatigue in long-term breast cancer survivors. J Cancer Surviv 4:405–414
Meeske K, Smith AW, Alfano CM, McGregor BA, McTiernan A, Baumgartner KB, Malone KE, Reeve BB, Ballard-Barbash R, Bernstein L (2007) Fatigue in breast cancer survivors two to five years post diagnosis: a HEAL Study report. Qual Life Res 16:947–960
Goedendorp MM, Gielissen MFM, Verhagen CAH, Peters MEJW, Bleijenberg G (2008) Severe fatigue and related factors in cancer patients before the initiation of treatment. Br J Cancer 99:1408–1414
Kober KM, Smoot B, Paul SM, Cooper BA, Levine JD, Miaskowski C (2016) Polymorphisms in cytokine genes are associated with higher levels of fatigue and lower levels of energy in women after breast cancer surgery. J Pain Symptom Manage 52:695-708.e4
Schmidt ME, Semik J, Habermann N, Wiskemann J, Ulrich CM, Steindorf K (2016) Cancer-related fatigue shows a stable association with diurnal cortisol dysregulation in breast cancer patients. Brain Behav Immun 52:98–105
LaVoy ECP, Fagundes CP, Dantzer R (2016) Exercise, inflammation, and fatigue in cancer survivors. Exerc Immunol Rev 22:82–93
Lee B-N, Dantzer R, Langley KE, Bennett GJ, Dougherty PM, Dunn AJ, Meyers CA, Miller AH, Payne R, Reuben JM et al (2004) A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. NeuroImmunoModulation 11:279–292
Cantarero-Villanueva I, Fernández-Lao C, Fernández-DE-Las-Peñas C, Díaz-Rodríguez L, Sanchez-Cantalejo E, Arroyo-Morales M (2011) Associations among musculoskeletal impairments, depression, body image and fatigue in breast cancer survivors within the first year after treatment: fatigue in breast cancer survivors within the first year after treatment. Eur J Cancer Care (Engl) 20:632–639
Kim SH, Son BH, Hwang SY, Han W, Yang J-H, Lee S, Yun YH (2008) Fatigue and depression in disease-free breast cancer survivors: prevalence, correlates, and association with quality of life. J Pain Symptom Manage 35:644–655
Tabrizi FM, Alizadeh S (2017) Cancer related fatigue in breast cancer survivors: in correlation to demographic factors. Maedica (Buchar) 12:106–111
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR (2000) Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol 18:743–753
Piper BF, Dibble SL, Dodd MJ, Weiss MC, Slaughter RE, Paul SM (1998) The revised Piper Fatigue Scale: psychometric evaluation in women with breast cancer. Oncol Nurs Forum 25:677–684
O’ Regan P, Hegarty J (2017) The importance of self-care for fatigue amongst patients undergoing chemotherapy for primary cancer. Eur J Oncol Nurs. 28:47–55
Chang YJ, Lee JS, Lee CG, Lee WS, Lee KS, Bang S-M, Wang XS, Mendoza TR, Cleeland CS, Yun YH (2007) Assessment of clinical relevant fatigue level in cancer. Support Care Cancer 15:891–896
Cantarero-Villanueva I, Fernández-Lao C, Díaz-Rodríguez L, Cuesta-Vargas AI, Fernández-de-las-Peñas C, Piper BF, Arroyo-Morales M (2014) The Piper Fatigue Scale-Revised: translation and psychometric evaluation in Spanish-speaking breast cancer survivors. Qual Life Res 23:271–276
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8:1153–1157
Badia X, Muriel C, Gracia A, Manuel-Núñez-Olarte J, Perulero N, Gálvez R, Carulla JS, Cleeland C (2003) Validación española del cuestionario Brief Pain Inventory en pacientes con dolor de causa neoplásica. Med Clin (Barc) 120:52–59
Sanz J (2001) Un instrumento para evaluar la eficacia de los procedimientos de inducción de estado de ánimo: “La Escala de Valoración del Estado de Ánimo” (EVEA). Análisis y modificación de conducta 27:71–110
Español-Moya MN, Ramírez-Vélez R (2014) Validación del cuestionario International Fitness Scale (IFIS) en sujetos colombianos de entre 18 y 30 años de edad. Rev Esp Salud Publica 88:271–278
Molina L, Sarmiento M, Peñafiel J, Donaire D, Garcia-Aymerich J, Gomez M, Ble M, Ruiz S, Frances A, Schröder H et al (2017) Validation of the regicor short physical activity questionnaire for the adult population. PLoS One 12:e0168148
Elosua R, Marrugat J, Molina L, Pons S, Pujol E (1994) Validation of the Minnesota leisure time physical activity questionnaire in Spanish men. Am J Epidemiol 139:1197–1209
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, Obrien WL, Bassett DR, Schmitz KH, Emplaincourt PO et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498–S516
Zawisza K, Tobiasz-Adamczyk B, Nowak W, Kulig J, Jedrys J (2010) Validity and reliability of the quality of life questionnaire (EORTC QLQ C30) and its breast cancer module (EORTC QLQ BR23). Ginekol Pol 81:262–267
Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, Franzini L, Williams A, de Haes HC, Hopwood P et al (1996) The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol 14:2756–2768
Mela CF, Kopalle PK (2002) The impact of collinearity on regression analysis: the asymmetric effect of negative and positive correlations. Appl Econ 34:667–677
Jean-Pierre P, Figueroa-Moseley CD, Kohli S, Fiscella K, Palesh OG, Morrow GR (2007) Assessment of cancer-related fatigue: implications for clinical diagnosis and treatment. Oncologist 12(Suppl 1):11–21
Okuyama T, Wang XS, Akechi T, Mendoza TR, Hosaka T, Cleeland CS, Uchitomi Y (2003) Validation study of the Japanese version of the brief fatigue inventory. J Pain Symptom Manage 25:106–117
Maass SWMC, Brandenbarg D, Boerman LM, Verhaak PFM, de Bock GH, Berendsen AJ (2021) Fatigue among long-term breast cancer survivors: a controlled cross-sectional study. Cancers (Basel) 13:1301
Schmidt ME, Chang-Claude J, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K (2012) Fatigue and quality of life in breast cancer survivors: temporal courses and long-term pattern. J Cancer Surviv 6:11–19
Falk Dahl CA, Reinertsen KV, Nesvold I-L, Fosså SD, Dahl AA (2010) A study of body image in long-term breast cancer survivors. Cancer 116:3549–3557
Romito F, Cormio C, Giotta F, Colucci G, Mattioli V (2012) Quality of life, fatigue and depression in Italian long-term breast cancer survivors. Support Care Cancer 20:2941–2948
Romito F, Montanaro R, Corvasce C, Di Bisceglie M, Mattioli V (2008) Is cancer-related fatigue more strongly correlated to haematological or to psychological factors in cancer patients? Support Care Cancer 16:943–946
Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, Veerman JL, Delwiche K, Iannarone ML, Moyer ML et al (2016) Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 354:i3857
Duijts SFA, Faber MM, Oldenburg HSA, van Beurden M, Aaronson NK (2011) Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors–a meta-analysis. Psychooncology 20:115–126
Peuckmann V, Ekholm O, Rasmussen NK, Møller S, Groenvold M, Christiansen P, Eriksen J, Sjøgren P (2007) Health-related quality of life in long-term breast cancer survivors: nationwide survey in Denmark. Breast Cancer Res Treat 104:39–46
Weber D, O’Brien K (2017) Cancer and cancer-related fatigue and the interrelationships with depression, stress, and inflammation. J Evid Based Complement Altern Med 22:502–512
Chrousos GP (1995) The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med 332(20):1351–1362. https://doi.org/10.1056/NEJM199505183322008
Reiche EMV, Nunes SOV, Morimoto HK (2004) Stress, depression, the immune system, and cancer. Lancet Oncol 5(10):617–625. https://doi.org/10.1016/S1470-2045(04)01597-9
Acknowledgements
We are grateful to all individuals who wanted to participate in this study.
Funding
This work was supported by the Spanish Ministry of Economy and Competitiveness [Plan Estatal de I + D + I 2013–2016]; Fondo de Investigación Sanitaria del Instituto de Salud Carlos III [PI14/01627]; Fondos Estructurales de la Unión Europea (FEDER). This study took place thanks to the additional funding from the University of Granada, Plan Propio de Investigación 2016. Excellence actions: Units of Excellence; Scientific Excellence Unit on Exercise and Health (UCEES).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Francisco Álvarez Salvago, José Daniel Jimenez García, Agustín Aibar Almazán, Fidel Hita Contreras, and Antonio Martínez Amat. The first draft of the manuscript was written by Francisco Álvarez Salvago, Jose Daniel Jimenez García, and Agustín Aibar Almazán and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in the line with the principles of The Declaration of Helsinki. Approval was granted by the Biomedical Research Ethical Committee of Granada (CEIm) (1038-N-16 I.P).
Consent to participate
Participants were welcomed for assessments by a physiotherapist, who gave detailed information about the study. Once they signed written informed consent, the researcher carried out the first assessment.
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Álvarez-Salvago, F., Jiménez-García, J.D., Martínez-Amat, A. et al. Time course and predictors of persistent cancer-related fatigue in long-term breast cancer survivors: a prospective observational study. Support Care Cancer 31, 35 (2023). https://doi.org/10.1007/s00520-022-07516-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07516-2