Abstract
Purpose
This study examined associations between self-reported cognitive functioning and social support as well as social ties among women with breast cancer.
Methods
The study included 3351 women from the Women’s Health Initiative Life and Longevity After Cancer cohort who were diagnosed with breast cancer stages I–III. Social support was assessed using a modified Medical Outcomes Study (MOS) Social Support Survey, and marital status was obtained from the baseline questionnaire. We also assessed social ties (e.g., number of friends, relatives, living children) and cognitive function (Functional Assessment of Cancer Therapy-Cognitive Function [FACT-COG]) on the year-1-follow up questionnaire. Multivariable quantile regression was used to estimate the changes in median cognitive scores. Kruskal–Wallis tests were used to assess the association of cognitive function with social ties.
Results
The majority of participants were non-Hispanic White (93.3%), presently married (49%), with at least a 4-year college degree (53.2%), and had been diagnosed with localized breast cancer (79%). A 10-point higher social support score correlated to a 0.32 higher (better) median cognitive score (p < 0.001). Women who were presently married tended to have better cognition than women who were divorced/separated or widowed (p = 0.01). Significant associations were also present for having close relatives (p < 0.001) or friends (p < 0.001), with cognitive scores being higher in those with at least one close relative or friend compared to none.
Conclusion
Women reporting higher social support and greater numbers of friends or relatives have higher cognitive functioning. Compared to divorced or separated women, married women were likely to have higher cognitive functioning. These findings suggest that social support assessments have the potential to help identify women at higher risk of cognitive decline.
Similar content being viewed by others
Introduction
In the USA, approximately 60% of breast cancer survivors are 65 years and older [1]. Compared to younger breast cancer survivors, older breast cancer survivors experience more side effects from cancer treatments and a more complicated recovery due to advanced age and comorbidities [2, 3]. Cognitive changes are the most common complications older survivors experience after treatment [4], and include problems with memory, processing speed, concentration, multitasking, and word retrieval [5]. These cognitive problems significantly impact older survivors’ functional status, level of independence, decision-making capacity, treatment adherence, quality of life, and ultimately their survival [6]. Therefore, investigating factors associated with cognitive functioning in older cancer survivors is crucial to identify targets for treatment.
Social support is defined as the perception and the exchange of social resources between at least two individuals (e.g., family, friends, neighbors, and co-workers) [7]. Compared to their younger counterparts, older breast cancer survivors are more likely to have pre-existing chronic diseases and are more vulnerable to treatment toxicities, thus causing them to experience more distress throughout their survivorship period [8,9,10]. As a result, they are more likely to require ongoing assistance and have many needs including emotional, informational, and tangible support from family or friends [3, 11, 12]. Research, however, has shown that older survivors have fewer supportive relationships to rely on, compared to younger survivors, due to death or illness in their age cohort [12]. Such unmet social support needs among older survivors can lead to social isolation and loneliness, negatively impacting treatment adherence and illness-management behaviors, and ultimately psychological and physical functioning [12,13,14]. Poor psychological well-being, and diminished physical functioning commonly correlate with decreased brain health and lower cognitive functioning [15, 16]. Thus, having adequate social support for older survivors may be necessary for maintaining good health and cognitive functioning.
Several non-cancer studies have shown that social support is related to cognitive functioning in healthy older adults. For example, one recent Women’s Health Initiative (WHI) study found that social support was positively associated with the cognitive performance among older adults [17]. Other studies have also reported that higher levels of social support are associated with diminished cognitive decline in older adults [18, 19]. Similarly, older adults who received higher levels of emotional and informational support along with increased contact with family and friends (i.e., social ties) have shown better cognitive function [20]. Several other studies further indicated that having positive social support and social ties is associated with the reduced risk of subsequent neurocognitive illness (e.g., dementia, stroke, or other neurological conditions) among older adults [21,22,23,24,25].
Although the mechanisms underlying the associations between social support and cognitive function remains unknown, prior research offers some potential clues. For example, several studies have suggested that social support may lower risk of intermediate physical and psychological factors, including anxiety, depression, and inflammation [26,27,28], which may accelerate the risk of cognitive decline [26,27,28]. Similarly, other work suggests that individuals who build social ties within larger social networks have a lower risk of cognitive decline than those who report weak social ties [18, 19, 29, 30]. Several studies indicate that close social ties buffer against psychological distress, which in turn can decrease the risk of cognitive decline [31, 32].
To date, the association of social support with cognitive functioning has not been examined thoroughly among breast cancer survivors. Furthermore, it is unclear whether or how social ties relate to survivors’ cognitive function. To address these gaps, we examined the associations between social support and cognitive functioning among women with breast cancer in the WHI Life and Longevity After Cancer (LILAC) cohort. We hypothesized that higher social support would be associated with better cognitive functioning. We also explored whether specific social ties were associated with lower cognitive functioning.
Methods
Study design and participants
Details of the WHI and the WHI LILAC cohort have been described previously [33, 34]. Briefly, between 1993 and 1998, the WHI recruited postmenopausal women between the ages of 50 and 79 years from 40 clinical centers throughout the USA. Participants were randomized into one or more clinical trials (n = 68,132) or an observational study (n = 93,676). Participants were followed for up to 10 years within the WHI, and many continued follow-up in the WHI extension studies (including the LILAC study) that began in 2005. In 2013, the WHI LILAC study enrolled WHI participants who had been diagnosed with select cancers (breast, endometrial, ovarian, lung, and colorectal cancers, melanoma, lymphoma, and leukemia) after their enrollment in WHI. The goal of the WHI LILAC was to expand the existing WHI data to support studies of cancer outcomes, survivorship, and molecular epidemiology [35].
For the current analyses, WHI LILAC participants were included if they were diagnosed with breast cancer stage I–III and had complete information on the following variables: age, education, race, marital status, cancer site, cancer stage at diagnosis, self-reported cancer treatment, a symptom checklist, overall cancer worry, physical activity, and social support on the LILAC baseline questionnaire as well as social ties (number of living children, close friends, and close relatives) and cognitive functioning on the year-1 follow-up LILAC questionnaire. All participants in the WHI and the WHI LILAC provided written informed consent before any study activities.
Social support measure
Social support was measured on the LILAC baseline questionnaire using five survey questions from the Medical Outcome Study (MOS) Social Support Survey [36]. Each question asked how often the respondent believed that social support was available to them when they needed it, e.g., “[How often is someone available] to take you to the doctor if you need to go?; to have a good time with?; to hug you?; to prepare your meals if you are unable to for yourself?; to understand your problems?” Possible responses for each item ranged from 1 (none of time) to 5 (all of the time). Scores were transformed to a 0–100 scale during analyses, with higher scores indicating greater social support. Internal consistency for the score was high (Cronbach α > 0.94) and has been validated among cancer survivors [36,37,38].
Social ties measures
Social ties were measured by one question about marital status in the baseline LILAC survey and in three survey questions in the 1-year follow up questionnaire. In the baseline questionnaire, participants were asked about their current marital status. The response options were (1) married/living as married, (2) widowed, (3) divorced/separated, and (4) never married. In the 1-year follow up questionnaire, participants were asked: “How many living children do you have?”, “How many relatives do you have with whom you feel close?”, and “How many close friends do you have?”. Possible responses for each item included none, 1–2, 3–5, and 6 or more for living children, and none, 1–2, 3–5, 6–9, and 10 or more for relatives and close friends. We separately analyzed the association of cognitive function with each type of social tie.
Cognitive functioning measure
Cognitive functioning was assessed on the year-1 LILAC follow-up questionnaire with the 20-item perceived cognitive impairment subscale of the FACT-COG [39]. Participants were asked to rate the frequency of cognitive problems that they had perceived in the past 7 days using a 5-point Likert-type scale. Possible responses for each item ranged from 0 (never) to 4 (several times a day). Answers were reverse coded, and a total score (range 0–80) was calculated. Higher scores indicate better cognitive functioning. Cronbach’s alpha for this subscale ranged from 0.77 to 0.86 [40,41,42].
Covariates
Factors that affect cognitive functioning were derived from published literature [43,44,45] and included age, race, ethnicity, education, cancer stage, self-reported cancer treatment, symptom distress, overall worry, and physical activity. Symptom severity was assessed using 24 items from the WHI symptom checklist, with scores ranging from 0 to 72, with higher scores indicating greater symptom severity. Overall worry was assessed using one survey question, with scores ranging from 1 (not at all) to 10 (a great deal), and a higher score indicating greater worry. Physical activity was derived from the WHI Physical Activity Questionnaire, which measured total duration (minutes/week) of and participation in mild to moderate or strenuous intensities of recreational physical activity [46]. The total minutes of moderate and strenuous exercise per week were calculated for each participant. This measure demonstrated moderate to substantial test–retest reliability [46].
Statistical analysis
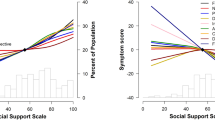
Descriptive statistics were used to summarize the patients’ demographic, clinical and symptom information. Continuous variables were reported as medians (first and third quartiles) and compared with FACT-COG scores using Spearman rank correlations. Categorical variables were reported as counts and percentages, with Fact-COG scores compared using Kruskal–Wallis tests. Linear regression was used to estimate the bivariate relationship between social support and patient cognitive functioning. However, normality assumptions for linear regression were not met by the data, and as a result, quantile regression was used to estimate changes in median FACT-COG scores. Multivariable quantile regression was used to assess whether social support explains the variation in cognitive function, after controlling for the effects of covariates. The final regression model included the primary exposure variable (social support), as well as covariates found to be significantly associated with the outcome of the FACT-COG total score (p < 0.05). Variables in the final regression model include the social support score and covariates (age at diagnosis, minutes of moderate/strenuous exercise per week, symptom count, and worry). Interactions with the social support score were checked for each covariate in the final model using Wald tests, and no interactions were significant. In addition, we conducted stratified analysis for the association of social support with FACT-COG scores in various demographic and clinical subgroups. Interaction effects were tested to evaluate whether the association between social support and FACT-COG scores were modified by race/ethnicity (Non-White or White), age (< 60, 60–69, 70–79, or > 80), marital status (never married, divorced/separated, widowed, or presently married), cancer stage (local or regional), and cancer treatments (chemotherapy, radiation, hormone, or others). Models included the main effects of social support and the variable of interest, along with the interaction term.
As an exploratory analysis, Kruskal–Wallis tests were used to assess the association of cognitive function with social ties (marital status and numbers of living children, close friends, and close relatives). Missing data were few (approximately 7% had missing data for variables in the multivariable quantile regression model), so complete case analysis was used for the multivariable modeling. We also conducted a sensitivity analysis with data imputation but there were no changes from the complete case results. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Sample characteristics
Among 3351 women included in the study cohort, the mean (SD) age was 70.2 (SD = 7.5) years. The average time between cancer diagnosis and FACT-COG completion was 9.4 (SD = 5.0) years. The majority of women were Non-Hispanic White (93.3%), presently married (49%), had at least a 4-year college degree (53.2%) and had localized breast cancer (79%). Approximately 70% did not receive chemotherapy but received radiation therapy, and nearly 67% received hormone therapy. Tables 1 and 2 displays characteristics of the study participants, and their correlations with cognitive functioning (FACT-COG). Better cognitive functioning was noted among women who were younger when diagnosed with breast cancer (r = − 0.084, p < 0.01), more engaged in moderate/strenuous exercise (r = 0.067, p < 0.01), and reported lower symptom severity (count: r = − 0.484, p < 0.01; severity: r = − 0.486, p < 0.01) as well as lower level of worry (r = -0.200, p < 0.01). However, no association was found between FACT-COG scores and race, ethnicity, education, cancer stage, or type of cancer treatments.
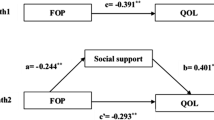
Primary analysis: association between social support and cognitive function
Results for the multivariable regression model are presented in Table 3. In this model, the symptom severity score was not included due to collinearity with symptom count. After adjusting for covariates (age at diagnosis, minutes of moderate/strenuous exercise per week, symptom count, and worry), a 10-point higher social support score corresponded to a 0.32 higher median FACT-COG score (β = 0.32, 95% CI: 0.16–0.47, p < 0.001). In addition, FACT-COG scores tended to decrease with increasing age at diagnosis (\(\beta\) = − 1.07, p < 0.001), increasing symptom counts (\(\beta\)= − 1.20, p < 0.001), and increasing worry (\(\beta\) = − 1.16, p < 0.001). There was no significant association between moderate/strenuous exercise and FACT-COG scores (p = 0.41).
Results of the effect modification analyses are presented in Table 4. In these models, we noted that the subgroups of non-white women (American Indian, Asian/Pacific Islander, Black, Hispanic/Latina, Other), women age < 60 at diagnosis, and women who were never married showed insignificant associations between social support and FACT-COG scores, although these groups all had small sample sizes relative to the other subgroups. The associations remained statistically significant for all other subgroups (all p < 0.05). While there were some differences in the parameter estimates across the subgroups, no variables (race/ethnicity, age at diagnosis, marital status, cancer stage, self-reported cancer treatments) had a significant modification of the effect of social support on FACT-COG scores (interaction p values all > 0.05).
Exploratory analysis: association between social tie variables and cognitive function
Table 5 shows that FACT-COG scores were significantly associated with marital status (p = 0.01), number of children (p = 0.01), number of relatives (p < 0.001), and number of friends (p < 0.001). Cognitive scores tended to be lower among those with more living children (median = 71 for none; median = 66 for 6 or more), but were higher with more relatives (median = 70 for none; median = 73 for 10 or more) or friends (median = 69 for none; median = 72 for 10 or more). Women who were presently married (median = 71) or never married (median = 72) had higher median cognitive scores, while women who were widowed had the lowest scores (Median = 69).
Discussion
To our knowledge, this is one of the few studies to examine the association of social support with cognitive functioning among a sample of US older female breast cancer survivors. In support of our hypothesis, our findings indicate that survivors with higher social support demonstrated higher perceived cognitive functioning than those women with lower social support. We also found that perceived cognitive functioning was significantly associated with marital status, and the number of living children, relatives and friends.
Our findings are in line with previous studies. Past research has found that social support is associated with better cognitive functioning in older adults[17, 19, 47], and is protective against memory decline [18]. One possible explanation for these associations is that social support can alleviate psychological distress, leading to improved cognitive function (or fewer declines) [48]. Similarly, several studies found that social support decreases the levels of psychological distress (anxiety, depression) among breast cancer patients[49, 50]. Future studies should include repeated measures of cognitive functioning and social support to further explore the dynamics of social support and cognitive function in breast cancer survivors, along with mechanisms that might explain this association.
These study findings also contribute to the increasing literature focused on the association of cognitive functioning with social relationships (e.g., social support and social ties). Recent systematic reviews have reported that older populations showed a greater decline in their cognition when their social relationships were functionally (e.g., social support) and structurally (e.g., social ties) poor [47, 51]. This previous research is consistent with our finding that cognitive functioning is associated with structural aspects (e.g., marital status and the number of friends, relatives, or children) as well as functional aspects (e.g., social support) of social relationships. In contrast to association of cognitive function with the number of friends and relatives, survivors with more than six living children showed lower levels of cognitive function compared to those with no children in this current study. A possible explanation for this negative association is that conflicts that occur in larger size family can lead to increased emotional distress [52, 53], resulting in cognitive decline [54]. Another possible explanation can be that women who have undergone childbirth more often may have relatively poor health conditions (e.g., changes in blood lipids and blood pressure, insulin resistance, weight gain) during and after pregnancy than those who have fewer births; in turn, those with poor health conditions may have poorer cognitive health later in life [55,56,57,58]. Further studies need to include more comprehensive aspects of social factors that may be associated with the cognitive function of breast cancer survivors. Increased understanding of this association will help identify survivors at risk of cognitive decline and assist in developing prevention and early intervention strategies for those with cognitive problems.
The findings of this study highlight the importance of social support among older adults with breast cancer. Healthcare providers need to encourage older survivors to participate in social activities to build supportive social relationships in order to improve or maintain overall health and cognitive functioning. It is important to inform survivors of how to ask for social support. Doing so will help buffer the impacts of cancer and cancer treatments and improve overall survivorship experiences. It is also important to educate survivors’ informal social networks (e.g., family or friends) about the positive impacts of support and survivors’ difficulties in asking for needed social support [3, 59]. Thus, in order to provide adequate social support to older cancer survivors, more research on social support interventions is needed.
The strengths of this study include the large number of study participants with extensive demographic, psychosocial, and cancer diagnosis and treatment data. However, this study has several limitations. First, social support, social ties, and cognitive functioning were only measured at one time point in the LILAC cohort, so we could not investigate a causal relationship between social support and cognitive function. Second, the social support measure included in LILAC provided limited data on the types of social support (e.g., tangible assistance, esteem support, network support). Future studies are needed that include data on the types of social support and additional social factors (e.g., social activity or social integration) to better understand if (and how) cognitive functioning is associated with these variables. Third, the included study participants were predominantly Non-Hispanic White (93.3%). This could limit the generalizability of these findings to other racial and ethnic groups. Future studies are needed that include participants with diverse racial/ethnic backgrounds. Lastly, this study used one subscale of the FACT-COG. Thus, we were unable to determine whether the obtained cognitive scores were clinically meaningful, because the published values are derived from the FACT-COG total score. [60, 61] Future studies that include full batteries of FACT-COG would help strengthen these study findings.
Conclusion
In summary, among post-menopausal older women with breast cancer, those with higher social support had better cognitive functioning than those with lower social support. Compared to divorced/separated women, married women were likely to have higher cognitive functioning. Also, those with a greater number of close friends or relatives had better cognitive functioning than those with no or one friend or relative. These findings suggest that provision of social support and availability of social ties during a time when women are at risk of social isolation could help prevent cognitive decline in aging breast cancer survivors. The current research contributes to the existing literature that suggests the importance of social support and social ties as factors associated with cognitive health.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LILAC:
-
Life and Longevity After Cancer cohort
- WHI:
-
Women’s Health Initiative
References
American Cancer Society (2020) Cancer treatments & survivorship facts and figures: 2019-2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-andsurvivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2019-2021.pdf
Robb C et al (2007) Impact of breast cancer survivorship on quality of life in older women. Crit Rev Oncol Hematol 62(1):84–91
Yoo GJ et al (2010) Older women, breast cancer, and social support. Support Care Cancer: Off J Multinat Assoc Support Care Cancer 18(12):1521–1530
Ahles TA et al (2022) Relationship between cognitive functioning and frailty in older breast cancer survivors. J Geriatr Oncol 13(1):27–32
Asher A (2011) Cognitive dysfunction among cancer survivors. Am J Phys Med Rehabil 90(5 Suppl 1):S16-26
Pergolotti M et al (2020) Embracing the complexity: older adults with cancer-related cognitive decline —Young International Society of Geriatric Oncology position paper. J Geriatr Oncol 11(2):237–243
Shumaker SA, Brownell A (1984) Toward a theory of social support: closing conceptual gaps. J Soc Issues 40(4):11–36
Hewitt M, Rowland JH, Yancik R (2003) Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci 58(1):82–91
Puts MT et al (2012) A systematic review of unmet needs of newly diagnosed older cancer patients undergoing active cancer treatment. Support Care Cancer 20(7):1377–1394
Shahrokni A et al (2016) Long-term toxicity of cancer treatment in older patients. Clin Geriatr Med 32(1):63–80
Yancik R et al (2001) Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. JAMA 285(7):885–892
Kadambi S et al (2020) Social support for older adults with cancer: Young International Society of Geriatric Oncology review paper. Journal of geriatric oncology 11(2):217–224
Gallant MP (2013) Social networks, social support, and health-related behavior. In: Martin LR, DiMatteo MR (eds) The Oxford Handbook of Health Communication, Behavior Change, and Treatment Adherence. Oxford University Press, p 0
Wright K (2015) Social Networks, interpersonal social support, and health outcomes: a health communication perspective. Front Commun. https://doi.org/10.3389/fcomm.2016.00010
Crouch A, Champion VL, Von Ah D (2022) Comorbidity, cognitive dysfunction, physical functioning, and quality of life in older breast cancer survivors. Support Care Cancer 30(1):359–366
Lange M et al (2019) Cancer-related cognitive impairment: an update on state of the art, detection, and management strategies in cancer survivors. Ann Oncol 30(12):1925–1940
Moreno GL et al (2021) The influence of social support on cognitive health in older women: a Women’s Health Initiative study. J Women Aging 34:1–17
Ertel KA, Glymour MM, Berkman LF (2008) Effects of social integration on preserving memory function in a nationally representative US elderly population. Am J Public Health 98(7):1215–1220
Hughes TF et al (2008) The association between social resources and cognitive change in older adults: evidence from the charlotte county healthy aging study. J Gerontol: Series B 63(4):P241–P244
La Fleur CG, Salthouse TA (2016) which aspects of social support are associated with which cognitive abilities for which people? J Gerontol: Series B 72(6):1006–1016
Khondoker M et al (2017) Positive and negative experiences of social support and risk of dementia in later life: an investigation using the english longitudinal study of ageing. J Alzheimers Dis 58(1):99–108
Litke R et al (2021) Modifiable risk factors in Alzheimer disease and related dementias: a review. Clin Ther 43(6):953–965
Zunzunegui MV et al (2003) Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J Gerontol B Psychol Sci Soc Sci 58(2):S93-s100
Crooks VC et al (2008) Social network, cognitive function, and dementia incidence among elderly women. Am J Public Health 98(7):1221–1227
Fratiglioni L et al (2000) Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet 355(9212):1315–1319
Hughes S et al (2014) Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinol 42:38–44
Perez-Tejada J et al (2019) Predictors of psychological distress in breast cancer survivors: A biopsychosocial approach. Eur J Cancer Care 28(6):e13166
Oh GH et al (2020) The effect of perceived social support on chemotherapy-related symptoms in patients with breast cancer: A prospective observational study. J Psychosom Res 130:109911
Ellwardt L, van Tilburg TG, Aartsen MJ (2015) The mix matters: complex personal networks relate to higher cognitive functioning in old age. Soc Sci Med 125:107–115
Wilson RS et al (2007) Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry 64(2):234–240
Kawachi I, Berkman LF (2001) Social ties and mental health. J Urban Health 78(3):458–467
Holt-Lunstad J, Smith TB, Layton JB (2010) Social Relationships and mortality risk: a meta-analytic review. PLoS Med 7(7):e1000316
Paskett ED et al (2018) The Women’s Health Initiative (WHI) Life and Longevity After Cancer (LILAC) Study: description and baseline characteristics of participants. Cancer Epidemiol Biomarkers Prev 27(2):125–137
(1998) Design of the Women’s Health Initiative Clinical Trial and Observational Study. The Women’s Health Initiative Study Group. Control Clin Trials 19(1):61–109
Paskett ED et al (2018) The Women’s Health Initiative (WHI) Life and Longevity After Cancer (LILAC) Study: Description and Baseline Characteristics of Participants. Cancer Epidemiol Biomark Prev 27(2):125–137
Sherbourne CD, Stewart AL (1991) The MOS social support survey. Soc Sci Med 32(6):705–714
Ganz PA et al (2002) Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst 94(1):39–49
Michael YL et al (2009) Influence of stressors on breast cancer incidence in the Women’s Health Initiative. Health Psychol: Off J Div Health Psychol, Am Psychol Assoc 28(2):137–146
Wagner LI, Sweet J, Butt Z, Lai JS, Cella D (2009) measuring patient self-reported cognitive function: development of the functional assessment of cancer therapy–cognitive function instrument. J Support Oncol 7:W32–W39
Lai J-S et al (2009) Evaluating the dimensionality of perceived cognitive function. J Pain Symptom Manage 37(6):982–995
Wagner LI et al (2009) Measuring patient self-reported cognitive function: development of the functional assessment of cancer therapy-cognitive function instrument. J Support Oncol 7(6):W32–W39
Von Ah, D. and E.F. Tallman, (2015) Perceived cognitive function in breast cancer survivors: evaluating relationships with objective cognitive performance and other symptoms using the functional assessment of cancer therapy—cognitive function instrument. J Pain Symptom Manage 49(4):697–706
Mayo SJ et al (2021) Cancer-related cognitive impairment in patients with non-central nervous system malignancies: an overview for oncology providers from the MASCC Neurological Complications Study Group. Support Care Cancer 29(6):2821–2840
Janelsins MC et al (2018) Longitudinal trajectory and characterization of cancer-related cognitive impairment in a nationwide cohort study. J Clin Oncol 36(32):3231–3239
Merriman JD et al (2013) Proposed mechanisms for cancer- and treatment-related cognitive changes. Semin Oncol Nurs 29(4):260–269
Meyer A-M et al (2009) Test-retest reliability of the Women’s Health Initiative physical activity questionnaire. Med Sci Sports Exerc 41(3):530–538
Kelly ME et al (2017) The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev 6(1):259
Fratiglioni L, Paillard-Borg S, Winblad B (2004) An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol 3(6):343–353
Escalera C et al (2019) Social support as a moderator in the relationship between intrusive thoughts and anxiety among Spanish-speaking Latinas with breast cancer. Psychooncol 28(9):1819–1828
Kornblith AB et al (2001) Social support as a buffer to the psychological impact of stressful life events in women with breast cancer. Cancer 91(2):443–454
Kuiper JS et al (2016) Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol 45(4):1169–1206
Lewandowski AS et al (2010) Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain 11(11):1027–1038
Dunbar SB et al (2008) Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs 23(3):258
Li M et al (2020) Family relationships and cognitive function among community-dwelling U.S. Chinese older adults. Res Aging 43(1):37–46
Dior UP et al (2013) Association between number of children and mortality of mothers: results of a 37-year follow-up study. Ann Epidemiol 23(1):13–18
Doblhammer G (2000) Reproductive history and mortality later in life: a comparative study of England and Wales and Austria. Popul Stud (Camb) 54(2):169–176
Grundy E, Tomassini C (2005) Fertility history and health in later life: a record linkage study in England and Wales. Soc Sci Med 61(1):217–228
Gagnon A et al (2009) Is there a trade-off between fertility and longevity? A comparative study of women from three large historical databases accounting for mortality selection. Am J Hum Biol 21(4):533–540
Yoo GJ et al (2010) Emotion work: disclosing cancer. Support Care Cancer 18(2):205–215
Henneghan AM et al (2021) Measuring self-reported cancer-related cognitive impairment: recommendations from the Cancer Neuroscience Initiative Working Group. J Natl Cancer Inst 113(12):1625–1633
Cheung YT et al (2014) Minimal clinically important difference (MCID) for the functional assessment of cancer therapy: cognitive function (FACT-Cog) in breast cancer patients. J Clin Epidemiol 67(7):811–820
Funding
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through 75N92021D00001, 75N92021D00002, 75N92021D00003, 75N92021D00004, 75N92021D00005. The WHI Life and Longevity after Cancer (LILAC) study is funded by UM1 CA173642 and a grant to EDP from the Breast Cancer Research Foundation. NT is supported by NCI K08CA245208. KC time was supported by American Cancer Society RSG-16–167-01-CPPB and National Institutes of Health, National Cancer Institute Grants R01CA230440, R01CA253028.
Author information
Authors and Affiliations
Contributions
Conceptualization: YY, NM, LM, and NT; data analysis: ME; supervision and validation: NM, PE; writing — original draft: YY; writing — review and editing: YY, ME, NM, LM, NT, KC, WJ, SN, SA, FS, PK, PE.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the Declaration of Helsinki and approval of this study was granted by each institution’s Institutional Review Board (IRB). Informed consent was obtained from all participants included in the study.
Consent to participate
All of the patients signed a written informed consent prior to study participation.
Consent for publication
All of the authors read the final version of the paper and approved its submission for publication.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., McLaughlin, E.M., Naughton, M.J. et al. Social Support, social ties, and cognitive function of women with breast cancer: findings from the Women’s Health Initiative (WHI) Life and Longevity After Cancer (LILAC) Study. Support Care Cancer 31, 48 (2023). https://doi.org/10.1007/s00520-022-07505-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07505-5