Abstract
Purpose
The sleep disturbance in cancer patients is more prevalent, and it significantly affects these patients’ recovery after the operation. However, the clinical characteristics regarding sleep quality are scarce. This study aimed to evaluate the quality of preoperative sleep quality and its risk factors in different cancer patients requiring elective surgery.
Patients and methods
Cancer patients who were scheduled for elective surgery were selected. The demographic data, basic preoperative diseases, and factors related to the preoperative hospital environment were also recorded. Self-made questionnaires (such as gender, age, and personal history), and the Anxiety Self-Assessment Scale were used to assess the patient's underlying condition. The modified Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the preoperative sleep status.
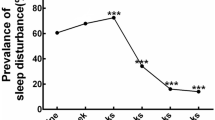
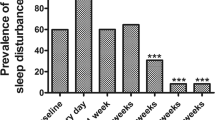
Results
A total of 297 patients completed the investigation. The incidence of preoperative sleep disturbance in cancer patients was 47.8%. Multiple logistic regression showed that patients with PSQI ≥ 7 were associated with females (odds ratios [95% confidence intervals]): 1.815 [1.031–3.193], p = 0.039), and the ward space was confined (3.127 [1.016–9.625], p = 0.047), which increased the possibility of sleep disturbance in cancer patients. Meanwhile, increased anxiety levels (1.323 [1.261–1.439], p < 0.001) significantly increased the likelihood of sleep disorders in cancer patients.
Conclusion
47.8% of sleep disturbance in cancer patients before surgery. Female patients, preoperative anxiety, and confined ward environment were independent risk factors of subjective sleep disturbance.


Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Davis MP, Goforth HW (2014) Long-term and short-term effects of insomnia in cancer and effective interventions. Cancer J 20(5):330–344
Chan-Chee C, Bayon V, Bloch J, Beck F, Giordanella JP, Leger D (2011) Epidemiology of insomnia in France. Rev Epidemiol Sante Publique 59(6):409–422
Davidson JR, MacLean AW, Brundage MD, Schulze K (2002) Sleep disturbance in cancer patients. Soc Sci Med 54(9):1309–1321
LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM (2009) Incidence and risk factors of insomnia in a population-based sample. Sleep 32(8):1027–1037
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Büttner-Teleagă A, Kim YT, Osel T, Richter K (2021) Sleep disorders in cancer-a systematic review. Int J Environ Res Public Health 18 (21)
Thorpy MJ (2012) Classification of sleep disorders. Neurotherapeutics 9(4):687–701
Vin-Raviv N, Akinyemiju TF, Galea S, Bovbjerg DH (2018) Sleep disorder diagnoses and clinical outcomes among hospitalized breast cancer patients: a nationwide inpatient sample study. Support Care Cancer 26(6):1833–1840
Ancoli-Israel S, Moore PJ, Jones V (2001) The relationship between fatigue and sleep in cancer patients: a review. Eur J Cancer Care (Engl) 10(4):245–255
Song C, Zhang R, Wang C, Fu R, Song W, Dou K, Wang S (2021) Sleep quality and risk of cancer: findings from the English longitudinal study of aging. Sleep 44 (3)
Wennberg AMV, Wu MN, Rosenberg PB, Spira AP (2017) Sleep disturbance, cognitive decline, and dementia: a review. Semin Neurol 37(4):395–406
Gallicchio L, Kalesan B (2009) Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 18(2):148–158
Marín JM (2017) Sleep and Cancer. Arch Bronconeumol 53(6):302–303
Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ (2005) Epidemiology of insomnia, depression, and anxiety. Sleep 28(11):1457–1464
Tian Y, Li LM (2017) Epidemiological study of sleep disorder in the elderly. Zhonghua Liu Xing Bing Xue Za Zhi 38(7):988–992
Takada M (2018) Hygiene in sleep: problems of sleeping habits in shift workers. Nihon Eiseigaku Zasshi 73(1):22–26
Zung WW (1971) A rating instrument for anxiety disorders. Psychosomatics 12(6):371–379
Buysse DJ, Reynolds CF., 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28 (2), 193-213
Xianchen WHWAHLTML (1996) Reliability and validity of Pittsburgh Sleep Quality Index. Chin J Psychiatry 02:103–107
Cao X, Zhou S, Yang B, Zhou J (2020) Relationship between dietary patterns and sleep disorders among health screening population in Changsha. Zhong Nan Da Xue Xue Bao Yi Xue Ban 45(10):1204–1214
LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM (2009) Incidence and risk factors of insomnia in a population-based sample. Sleep 32(8):1027–1037
Clevenger L, Schrepf A, DeGeest K, Bender D, Goodheart M, Ahmed A, Dahmoush L, Penedo F, Lucci Iii J, Thaker PH, Mendez L, Sood AK, Slavich GM, Lutgendorf SK (2013) Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer 119(17):3234–3241
Zheng W, Luo XN, Li HY, Ke XY, Dai Q, Zhang CJ, Cassidy RM, Zhang XY, Ning YP (2018) Gender differences in the prevalence and clinical correlates of sleep disturbance in general hospital outpatients. Psychiatry Res 269:134–139
Pengo MF, Won CH, Bourjeily G (2018) Sleep in women across the life span. Chest 154(1):196–206
Ayaki M, Tsubota K, Kawashima M, Kishimoto T, Mimura M, Negishi K (2018) Sleep disorders are a prevalent and serious comorbidity in dry eye. Invest Ophthalmol Vis Sci 59 (14), Des143-des150
Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Riemann D (2003) Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety 17(3):162–172
Roehrs T, Kapke A, Roth T, Breslau N (2006) Sex differences in the polysomnographic sleep of young adults: a community-based study. Sleep Med 7(1):49–53
Kocevska D, Lysen TS, Dotinga A, Koopman-Verhoeff ME, Luijk M, Antypa N, Biermasz NR, Blokstra A, Brug J, Burk WJ, Comijs HC, Corpeleijn E, Dashti HS, de Bruin EJ, de Graaf R, Derks IPM, Dewald-Kaufmann JF, Elders PJM, Gemke R, Grievink L, Hale L, Hartman CA, Heijnen CJ, Huisman M, Huss A, Ikram MA, Jones SE, Velderman MK, Koning M, Meijer AM, Meijer K, Noordam R, Oldehinkel AJ, Groeniger JO, Penninx B, Picavet HSJ, Pieters S, Reijneveld SA, Reitz E, Renders CM, Rodenburg G, Rutters F, Smith MC, Singh AS, Snijder MB, Stronks K, Ten Have M, Twisk JWR, Van de Mheen D, van der Ende J, van der Heijden KB, van der Velden PG, van Lenthe FJ, van Litsenburg RRL, van Oostrom SH, van Schalkwijk FJ, Sheehan CM, Verheij RA, Verhulst FC, Vermeulen MCM, Vermeulen RCH, Verschuren WMM, Vrijkotte TGM, Wijga AH, Willemen AM, Ter Wolbeek M, Wood AR, Xerxa Y, Bramer WM, Franco OH, Luik AI, Van Someren EJW, Tiemeier H (2021) Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat Hum Behav 5(1), 113–122.
Ulander M, Rångtell F, Theorell-Haglöw J (2021) Sleep measurements in women. Sleep Med Clin 16(4):635–648
Norris W, Baird WL (1967) Pre-operative anxiety: a study of the incidence and aetiology. Br J Anaesth 39(6):503–509
Kumar A, Dubey PK, Ranjan A (2019) Assessment of anxiety in surgical patients: an observational study. Anesth Essays Res 13(3):503–508
Tulloch I, Rubin JS (2019) Assessment and management of preoperative anxiety. J Voice 33(5):691–696
Cox RC, Olatunji BO (2016) A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord 37:104–129
Zung WWK (1971) A rating instrument for anxiety disorders. Psychosomatics 12(6):371–379
Tou S, Tou W, Mah D, Karatassas A, Hewett P (2013) Effect of preoperative two-dimensional animation information on perioperative anxiety and knowledge retention in patients undergoing bowel surgery: a randomized pilot study. Colorectal Dis 15(5):e256–e265
Xie H, Kang J, Mills GH (2009) Clinical review: The impact of noise on patients’ sleep and the effectiveness of noise reduction strategies in intensive care units. Crit Care 13(2):208
Walder B, Francioli D, Meyer JJ, Lançon M, Romand JA (2000) Effects of guidelines implementation in a surgical intensive care unit to control nighttime light and noise levels. Crit Care Med 28(7):2242–2247
Wesselius HM, van den Ende ES, Alsma J, Ter Maaten JC, Schuit SCE, Stassen PM, de Vries OJ, Kaasjager K, Haak HR, van Doormaal FF, Hoogerwerf JJ, Terwee CB, van de Ven PM, Bosch FH, van Someren EJW, Nanayakkara PWB (2018) Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med 178(9):1201–1208
Frisk U, Nordström G (2003) Patients’ sleep in an intensive care unit–patients’ and nurses’ perception. Intensive Crit Care Nurs 19(6):342–349
Sun W, Yu Y, Yuan J, Li C, Liu T, Lin D, Lau A, Zhong C, Xu T, Shan G (2015) Sleep duration and quality among different occupations–China national study. PLoS ONE 10(3):e0117700
Shim JY, Lee S, Lee IH, Jeong YM (2021) The impact of sleep quality and education level on the relationship between depression and suicidal ideation in parents of adolescents. Healthcare (Basel) 9 (9)
Palagini L, Mauri M, Faraguna U, Carli L, Tani C, Dell’Osso L, Mosca M, Riemann D (2016) Insomnia symptoms, perceived stress and coping strategies in patients with systemic lupus erythematosus. Lupus 25(9):988–996
Kalmbach DA, Anderson JR, Drake CL (2018) The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res 27(6):e12710
Acknowledgements
Thanks for the guidance and help from Wenzhou Medical University.
Funding
This work was supported by the Major Science and Technology Projects of Wenzhou Science and Technology Bureau (No. 2021Y0335) and Clinical Research Application Project of Health Department of Zhejiang Province (No2022KY894).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Zihan Wang, Wenwen Du, and Shenhui Jin. The first draft of the manuscript was written by Zihan Wang, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Clinical Research Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University. No. KY2021-102.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors declare that all content of the article can be published.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Du, W., Jin, S. et al. Analysis of preoperative sleep quality and related influencing factors in cancer patients. Support Care Cancer 31, 4 (2023). https://doi.org/10.1007/s00520-022-07483-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07483-8