Abstract
Purpose
This study is to identify and synthesize the available evidence of bowel symptom experiences of patients with rectal cancer after sphincter-preserving surgery (SPS).
Methods
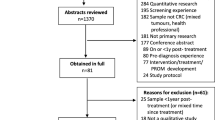
This qualitative meta-synthesis was conducted following the Joanna Briggs Institute (JBI) qualitative systematic review methodology and reported following the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) guidelines. Seven databases were searched on 22 December 2021. The selected studies were reviewed by two independent reviewers, and disagreements were resolved by discussion or with a third reviewer.
Results
Seven qualitative articles were included in the meta-synthesis with 192 total rectal cancer patients. The review summarized 53 qualitative findings into three synthesized findings: (a) Patients experienced bowel symptoms and triggered additional physiological problems, and they underestimated bowel symptoms; (b) patients had many negative emotions, and their daily life and social interaction were disturbed; and (c) patients adopted strategies to adapt or control their bowel symptoms. According to the ConQual evidence grading approach, the confidence of the synthesized findings was rated as moderate to low.
Conclusions
The bowel symptoms of patients with rectal cancer after SPS have troubled their lives. Timely acquisition of symptom-related knowledge and enhancement of their coping abilities are important for the control and management of bowel symptoms. Healthcare professionals should clearly understand the bowel symptoms that patients may experience after SPS and provide supportive care for patients to improve patients’ self-management abilities and quality of life.
Trial registration
PROSPERO: CRD42021242610.

Similar content being viewed by others
Data availability
Not applicable.
References
Martellucci J (2016) Low anterior resection syndrome: a treatment algorithm. Dis Colon Rectum 59(1):79–82. https://doi.org/10.1097/DCR.0000000000000495
Nguyen TH, Chokshi RV (2020) Low anterior resection syndrome. Curr Gastroenterol Rep 22(10):48. https://doi.org/10.1007/s11894-020-00785-z
Keane C, Fearnhead NS, Bordeianou LG, Christensen P, Basany EE, Laurberg S et al (2020) International consensus definition of low anterior resection syndrome. Dis Colon Rectum 63(3):274–284. https://doi.org/10.1097/DCR.0000000000001583
Hughes DL, Cornish J, Morris C, LTM (2017) Group functional outcome following rectal surgery-predisposing factors for low anterior resection syndrome. Int J Colorectal Dis 32(5):691–697. https://doi.org/10.1007/s00384-017-2765-0
Bohlok A, Mercier C, Bouazza F, Galdon MG, Moretti L, Donckier V et al (2020) The burden of low anterior resection syndrome on quality of life in patients with mid or low rectal cancer. Support Care Cancer 28(3):1199–1206. https://doi.org/10.1007/s00520-019-04901-2
Lai X, Wong FK, Ching SS (2013) Review of bowel dysfunction of rectal cancer patients during the first five years after sphincter-preserving surgery: a population in need of nursing attention. Eur J Oncol Nurs 17(5):681–692. https://doi.org/10.1016/j.ejon.2013.06.001
Li ZY, Hou XT, Pang D, Lu Q, Yang P, Jin SL (2017) The relationship between bowel symptoms and quality of life among patients with mid and low rectal cancer after sphincter preserving surgery. Chin Nurs Manag 17(8):1101–1106. https://doi.org/10.3969/j.issn.1672-1756.2017.08.022
Pieniowski EHA, Palmer GJ, Juul T, Lagergren P, Johar A, Emmertsen KJ et al (2019) Low anterior resection syndrome and quality of life after sphincter-sparing rectal cancer surgery: a long-term longitudinal follow-up. Dis Colon Rectum 62(1):14–20. https://doi.org/10.1097/DCR.0000000000001228
NICE (2021) Colorectal cancer. NICE Guidance. https://www.nice.org.uk/guidance/ng151. Accessed 28 Dec 2021
Landers M, McCarthy G, Livingstone V, Savage E (2014) Patients’ bowel symptom experiences and self-care strategies following sphincter-saving surgery for rectal cancer. J Clin Nurs 23(15–16):2343–2354. https://doi.org/10.1111/jocn.12516
Chen TY, Emmertsen KJ, Laurberg S (2020) Bowel dysfunction after rectal cancer treatment: a study comparing the specialist’s versus patient’s perspective. BMJ Open 4(1):e003374. https://doi.org/10.1136/bmjopen-2013-003374
Jimenez-Gomez LM, Espin-Basany E, Marti-Gallostra M, Sanchez-Garcia JL, Vallribera-Valls F, Armengol-Carrasco M (2016) Low anterior resection syndrome: a survey of the members of the American Society of Colon and Rectal Surgeons (ASCRS), the Spanish Association of Surgeons (AEC), and the Spanish Society of Coloproctology (AECP). Int J Colorectal Dis 31(4):813–823. https://doi.org/10.1007/s00384-016-2511-z
McDaniel RW, Rhodes VA (1995) Symptom experience. Semin OncolNurs 11(4):232–234. https://doi.org/10.1016/s0749-2081(05)80002-6
Lobchuk MM (2003) The memorial symptom assessment scale: modified for use in understanding family caregivers’ perceptions of cancer patients’ symptom experiences. J Pain Symptom Manage 26(1):644–654. https://doi.org/10.1016/s0885-3924(03)00205-7
Jordan Z, Pittman P (2006) A short history of a big idea: The Joanna Briggs Institute. Ausmed Publications, Australia
Hannes K, Lockwood C, Pearson A (2010) A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual Health Res 20(12):1736–1743. https://doi.org/10.1177/1049732310378656
Aromataris E, Munn Z (2020) JBI manual for evidence synthesis. JBI. https://synthesismanual.jbi.global. Accessed 12 Nov 2021
Tong A, Flemming K, McInnes E, Oliver S, Craig J (2012) Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 12:181. https://doi.org/10.1186/1471-2288-12-181
Munn Z, Porritt K, Lockwood C, Aromataris E, P. A, (2014) Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol 14:2–7. https://doi.org/10.1186/1471-2288-14-108
Desnoo L, Faithfull S (2006) A qualitative study of anterior resection syndrome: the experiences of cancer survivors who have undergone resection surgery. Eur J Cancer Care (Engl) 15(3):244–251. https://doi.org/10.1111/j.1365-2354.2005.00647.x
Landers M, McCarthy G, Savage E (2012) Bowel symptom experiences and management following sphincter saving surgery for rectal cancer: a qualitative perspective. Eur J Oncol Nurs 16(3):293–300. https://doi.org/10.1016/j.ejon.2011.07.002
Taylor C, Bradshaw E (2013) Tied to the toilet: lived experiences of altered bowel function (anterior resection syndrome) after temporary stoma reversal. J Wound Ostomy Continence Nurs 40(4):415–421. https://doi.org/10.1097/WON.0b013e318296b5a4
Lu LC, Huang XY, Chen CC (2017) The lived experiences of patients with post-operative rectal cancer who suffer from altered bowel function: a phenomenological study. Eur J Oncol Nurs 31:69–76. https://doi.org/10.1016/j.ejon.2017.10.004
Reinwalds M, Blixter A, Carlsson E (2017) A descriptive, qualitative study to assess patient experiences following stoma reversal after rectal cancer surgery. Ostomy Wound Manage 63(12):29–37
Reinwalds M, Blixter A, Carlsson E (2018) Living with a resected rectum after rectal cancer surgery-struggling not to let bowel function control life. J Clin Nurs 27(3–4):623–634. https://doi.org/10.1111/jocn.14112
Tsui H, Huang XY (2021) Experiences of losing bowel control after lower anterior resection with sphincter saving surgery for rectal cancer: a qualitative study. Cancer Nurs. https://doi.org/10.1097/NCC.0000000000001036
Remes-Troche JM, De-Ocampo S, Valestin J, Rao SSC (2010) Rectoanal reflexes and sensorimotor response in rectal hyposensitivity. Dis Colon Rectum 53(7):1047–1054. https://doi.org/10.1007/DCR.0b013e3181dcb2d6
Wei C (2016) Advances in total anorectal reconstruction after abdominoperineal resection. Chin J Gen Surg 25:598–603. https://doi.org/10.3978/j.issn.1005-6947.2016.04.022
Thomas G, van Heinsbergen M, van der Heijden J, Slooter G, Konsten J, Maaskant S (2019) Awareness and management of low anterior resection syndrome: a Dutch national survey among colorectal surgeons and specialized nurses. Eur J Surg Oncol: J Eur Soc Surg Oncol British Assoc Surg Oncol 45(2):174–179. https://doi.org/10.1016/j.ejso.2018.11.001
Lee KH, Kim JS, Kim JY (2019) Efficacy of biofeedback therapy for objective improvement of pelvic function in low anterior resection syndrome. Annals of Surgical Treatment and Research 97(4):194–201. https://doi.org/10.4174/astr.2019.97.4.194
Kalkdijk-Dijkstra AJ, van der Heijden JAG, van Westreenen HL, Broens PMA, Trzpis M, Pierie JPEN et al (2020) Pelvic floor rehabilitation to improve functional outcome and quality of life after surgery for rectal cancer: study protocol for a randomized controlled trial (FORCE trial). Trials 21(1):112. https://doi.org/10.1186/s13063-019-4043-7
Mekhael M, Kristensen HØ, Larsen HM, Juul T, Emmanuel A, Krogh K et al (2021) Transanal irrigation for neurogenic bowel disease, low anterior resection syndrome, faecal incontinence and chronic constipation: a systematic review. J Clin Med 10(4):753. https://doi.org/10.3390/jcm10040753
Sun XC, Zhong WF, Lu JJ, Zhuang WZ (2021) Influence of psychological nursing intervention on psychological state, treatment compliance, and immune function of postoperative patients with rectal cancer. J Oncol 2021:1071490. https://doi.org/10.1155/2021/1071490
HovdenakJakobsen I, Juul T, Thaysen HV, Johansen C, Laurberg S (2019) Laurberg Differences in baseline characteristics and 1-year psychological factors between participants and non-participants in the randomized, controlled trial regarding patient-led follow-up after rectal cancer (FURCA). Acta Oncol 58(5):627–633. https://doi.org/10.1080/0284186X.2019.1581948
Wang SM, Tian HQ, Xue RR (2021) Using psychological interventions in the nursing care of rectal cancer patients. Am J Transl Res 13(6):7282–7287
Hou X-T, Pang D, Lu Q, Yang P, Jin S-L (2017) Bowel dysfunction and self-management for bowel symptoms after sphincter-preserving surgery. Cancer Nurs 40(4):9–16. https://doi.org/10.1097/ncc.0000000000000393
Li C, Li ZY, Lu Q, Zhou YJ, Qin XY, Wu AW et al (2023) The effectiveness of a self-management program of bowel dysfunction in patients with mid and low rectal cancer after sphincter-preserving surgery: a pilot randomized controlled trial. Cancer Nurs 46(1):67–76. https://doi.org/10.1097/NCC.0000000000001065
van de Velde D, de Zutter F, Satink T, Costa U, Janquart S, Senn D, de Vriendt P (2019) Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 9(7):e027775. https://doi.org/10.1136/bmjopen-2018-027775
Grady PA, Gough LL (2014) Self-management: a comprehensive approach to management of chronic conditions. Am J Public health 104(8):25–31
The Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party (2014) JBI grades of recommendation. JBI. https://jbi.global/sites/default/files/2019-05/JBI-grades-of-recommendation_2014.pdf. Accessed 15 Nov 2021
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Conceptualization, methodology, and supervision were performed by Li Cong, Tang Haiyan, Zhang Yue, Zhang Qiuwen, Yang Wantong, Yu Hongxia, and Pang Dong. The first draft of the manuscript was written by Li Cong, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, C., Tang, H., Zhang, Y. et al. Experiences of bowel symptoms in patients with rectal cancer after sphincter-preserving surgery: a qualitative meta-synthesis. Support Care Cancer 31, 23 (2023). https://doi.org/10.1007/s00520-022-07473-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07473-w