Abstract
Purpose
It is important for palliative care providers to identify what factors are associated with a “good death” for patients with advanced cancer. We aimed to identify factors associated with a “good death” evaluated by the Good Death Scale (GDS) score among inpatients with advanced cancer in palliative care units (PCUs) in Japan.
Methods
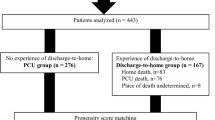
The study is a sub-analysis of a multicenter prospective cohort study conducted in Japan. All variables were recorded on a structured data collecting sheet designed for the study. We classified each patient into better GDS group or worse GDS group, and examined factors associated with better GDS using multivariate analysis.
Results
Between January and December 2017, 1896 patients were enrolled across 22 PCUs in Japan. Among them, a total of 1157 patients were evaluated. Five variables were significantly associated with a better GDS score in multivariate analysis: preferred place of death at PCU (odds ratio [OR] 2.85; 95% confidence interval [CI] 1.72–4.71; p < 0.01), longer survival time (OR 1.02; 95% CI 1.00–1.03; p < 0.01), not sudden death (OR 1.96; 95% CI 1.27–3.04; p < 0.01), better spiritual well-being in the last 3 days in life (OR 0.53; 95% CI 0.42–0.68; p < 0.01), and better communication between patient and family (OR 0.81; 95% CI 0.66–0.98; p = 0.03).
Conclusions
We identified factors associated with a “good death” using GDS among advanced cancer patients in Japanese PCUs. Recognition of factors associated with GDS could help to improve the quality of end-of-life care.

Similar content being viewed by others
Abbreviations
- (CCS):
-
Communication Capacity Scale
- (CI):
-
Confidence interval
- (DRS-R-98):
-
Delirium Rating Scale-revised-98
- (EASED):
-
East-Asian collaborative cross-cultural Study to Elucidate the Dying Process
- (ECOG PS):
-
Eastern Cooperative Oncology Group performance status
- (GDI):
-
Good Death Inventory
- (GDS):
-
Good Death Scale
- (IPOS):
-
Integrated Palliative Outcome Scale
- (STAS-J):
-
Japanese version of STAS
- (MDAS):
-
Memorial Delirium Assessment Scale
- (OR):
-
Odds ratio
- (PCU):
-
Palliative care unit
- (QOD):
-
Quality of dying
- (STAS):
-
Support Team Assessment Schedule
- (SWB):
-
Spiritual well-being
References
Morita T, Oyama Y, Cheng SY et al (2015) Palliative care physicians’ attitudes toward patient autonomy and a good death in East Asian countries. J Pain Symptom Manage 50(190–199):e191
Hirai K, Miyashita M, Morita T et al (2006) Good death in Japanese cancer care: a qualitative study. J Pain Symptom Manage 31:140–147
Miyashita M, Sanjo M, Morita T et al (2007) Good death in cancer care: a nationwide quantitative study. Ann Oncol 18:1090–1097
Miyashita M, Morita T, Sato K et al (2008) Good death inventory: a measure for evaluating good death from the bereaved family member’s perspective. J Pain Symptom Manage 35:486–498
Randall Curtis J, Patrick Donald L, Engelberg Ruth A et al (2002) A measure of the quality of dying and death: initial validation using after-death interviews with family members. J Pain Symptom Manage 24:17–31
Kodama M, Kobayashi M, Katayama K et al (2017) Development and linguistic validation of the Japanese version of the Good Death Scale (in Japanese). Palliat Care Res 12:311–316
Cheng SY, Lin WY, Cheng YH et al (2016) Cancer patient autonomy and quality of dying-a prospective nationwide survey in Taiwan. Psychooncology 25:179–186
Leung KK, Tsai JS, Cheng SY et al (2010) Can a good death and quality of life be achieved for patients with terminal cancer in a palliative care unit? J Palliat Med 13:1433–1438
Cheng SY, Dy S, Huang SB et al (2013) Comparison of proxy ratings of main family caregivers and physicians on the quality of dying of terminally ill cancer patients. Jpn J Clin Oncol 43:795–804
Cheng SY, Dy S, Fang PH et al (2013) Evaluation of inpatient multidisciplinary palliative care unit on terminally ill cancer patients from providers’ perspectives: a propensity score analysis. Jpn J Clin Oncol 43:161–169
Chen SY, Hu XY, Liu WJ (2008) Good death study of elderly patients with terminal cancer in Taiwan. J Palliat Med 22:626–632
Kastbom L, Milberg A, Karlsson M (2017) A good death from the perspective of palliative cancer patients. Support Care Cancer 25:933–939
Krikorian A, Maldonado C, Pastrana T (2020) Patient’s perspectives on the notion of a good death: a systematic review of the literature. J Pain Symptom Manage 59:152–164
Ikari T, Hiratsuka Y, Yamaguchi T et al (2021) “3-Day Surprise Question” to predict prognosis of advanced cancer patients with impending death: Multicenter prospective observational study. Cancer Med 10:1018–1026
Bruera S, Chisholm G, Dos Santos R et al (2015) Frequency and factors associated with unexpected death in an acute palliative care unit: expect the unexpected. J Pain Symptom Manage 49:822–827
Yamaguchi T, Maeda I, Hatano Y et al (2021) Communication and behavior of palliative care physicians of patients with cancer near end of life in three east Asian countries. J Pain Symptom Manage 61:315–322
Sakurai H, Miyashita M, Imai K et al (2019) Validation of the integrated palliative care outcome scale (IPOS)—Japanese version. Jpn J Clin Oncol 49:257–262
Sakurai H, Miyashita M, Morita T et al (2021) Comparison between patient-reported and clinician-reported outcomes: validation of the Japanese version of the Integrated Palliative care Outcome Scale for staff. Palliat Support Care 5:1–7
Miyashita M, Yasuda M, Baba R et al (2010) Inter-rater reliability of proxy simple symptom assessment scale between physician and nurse: a hospital-based palliative care team setting. Eur J Cancer Care 19:124–130
Breitbart W, Rosenfeld B, Roth A et al (1997) The Memorial Delirium Assessment Scale. J Pain Symptom Manag 13:128–137
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Downing GM, Wainwright W (2006) Medical care of the dying. Victoria Hospice Society, 4th edn. Victoria, BC
Hiratsuka Y, Yamaguchi T, Maeda I et al (2020) The Functional Palliative Prognostic Index: a scoring system for functional prognostication of patients with advanced cancer. Support Care Cancer 28:6067–6074
Cheng SY, Dy S, Hu WY et al (2012) Factors affecting the improvement of quality of dying of terminally ill patients with cancer through palliative care: a ten-year experience. J Palliat Med 15:854–862
Wu CY, Chen PJ, Ho TL et al (2021) To hydrate or not to hydrate? The effect of hydration on survival, symptoms and quality of dying among terminally ill cancer patients. BMC Palliat Care 20:13
Glenys C, Kristian P, Rowan H et al (2015) Communication between family carers and health professionals about end-of-life care for older people in the acute hospital setting: a qualitative study. BMC Palliat Care 14:35
Ito S, Morita T, Uneno Y et al (2021) Incidence and associated factors of sudden unexpected death in advanced cancer patients: a multicenter prospective cohort study. Cancer Med 10:4939–4947
Hiratsuka Y, Suh Sang-Yeon, Maeda I et al (2021) Factors influencing spiritual well-being in terminally ill cancer inpatients in Japan. Support Care Cancer 29:2795–2802
Hiratsuka Y, Suh SY, Kim SH et al (2021) Factors related to spiritual well-being in the last days of life in three East Asian countries: an international multicenter prospective cohort study. Palliat Med 35:1564–1577
Jaw ST, Chih HW, Tai YC et al (2005) Fear of death and good death among the young and elderly with terminal cancers in Taiwan. J Pain Symptom Manage 29:344–351
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing. This study was performed in the East-Asian collaborative cross-cultural Study to Elucidate the Dying process (EASED). The participating study sites and site investigators in Japan were as follows: Satoshi Inoue, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Naosuke Yokomichi, M.D., Ph.D. (Department of Palliative and Supportive Care, Seirei Mikatahara General Hospital), Kengo Imai, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Tatsuya Morita, M.D. (Department of Palliative and Supportive Care, Seirei Mikatahara General Hospital), Hiroaki Tsukuura, M.D., Ph.D. (Department of Palliative Care, TUMS Urayasu Hospital), Toshihiro Yamauchi, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Akemi Shirado Naito, M.D. (Department of palliative care Miyazaki Medical Association Hospital), Akira Yoshioka, M.D., Ph.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Shuji Hiramoto, M.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Ayako Kikuchi, M.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Tetsuo Hori, M.D. (Department of Respiratory surgery, Mitsubishi Kyoto Hospital), Hiroyuki Kohara, M.D., Ph.D. (Hiroshima Prefectural Hospital), Hiromi Funaki, M.D. (Hiroshima Prefectural Hospital), Keiko Tanaka, M.D., Ph.D. (Department of Palliative Care Tokyo Metropolitan Cancer & Infectious Diseases Center Komagome Hospital), Kozue Suzuki, M.D. (Department of Palliative Care Tokyo Metropolitan Cancer & Infectious Diseases Center Komagome Hospital), Tina Kamei, M.D. (Department of Palliative Care, NTT Medical Center Tokyo), Yukari Azuma, M.D. (Home Care Clinic Aozora Shin-Matsudo), Teruaki Uno, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Jiro Miyamoto, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Hirofumi Katayama, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Hideyuki Kashiwagi, M.D., MBA. (Aso Iizuka Hospital / Transitional and Palliative Care), Eri Matsumoto, M.D. (Aso Iizuka Hospital / Transitional and Palliative Care), Takeya Yamaguchi, M.D. (Japan Community Health care Organization Kyushu Hospital / Palliative Care), Tomonao Okamura, M.D., MBA. (Aso Iizuka Hospital / Transitional and Palliative Care), Hoshu Hashimoto, M.D., MBA. (Inoue Hospital / Internal Medicine), Shunsuke Kosugi, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Nao Ikuta, M.D. (Department of Emergency Medicine, Osaka Red Cross Hospital), Yaichiro Matsumoto, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Takashi Ohmori, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Takehiro Nakai, M.D. (Immuno-Rheumatology Center, St Luke's International Hospital), Takashi Ikee, M.D. (Department of Cardiorogy, Aso Iizuka Hospital), Yuto Unoki, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Kazuki Kitade, M.D. (Department of Orthopedic Surgery, Saga-Ken Medical Centre Koseikan), Shu Koito, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Nanao Ishibashi, M.D. (Environmental Health and Safety Division, Environmental Health Department, Ministry of the Environment), Masaya Ehara, M.D. (TOSHIBA), Kosuke Kuwahara, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Shohei Ueno, M.D. (Department of Hematology / Oncology, Japan Community Healthcare Organization Kyushu Hospital), Shunsuke Nakashima, M.D. (Oshima Clinic), Yuta Ishiyama, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Akihiro Sakashita, M.D., Ph.D. (Department of Palliative Medicine, Kobe University School of Medicine), Ryo Matsunuma, M.D. (Department of Palliative Medicine, Kobe University Graduate School of Medicine), Hana Takatsu, M.D. (Division of Palliative Care, Konan Medical Center), Takashi Yamaguchi, M.D., Ph.D. (Division of Palliative Care, Konan Medical Center), Satoko Ito, M.D. (Hospice, The Japan Baptist Hospital), Toru Terabayashi, M.D. (Hospice, The Japan Baptist Hospital), Jun Nakagawa, M.D. (Hospice, The Japan Baptist Hospital), Tetsuya Yamagiwa, M.D., Ph.D. (Hospice, The Japan Baptist Hospital), Akira Inoue, M.D., Ph.D. (Department of Palliative Medicine Tohoku University School of Medicine), Mitsunori Miyashita, R.N., Ph.D. (Department of Palliative Nursing, Health Sciences, Tohoku University Graduate School of Medicine), Saran Yoshida, Ph.D. (Graduate School of Education, Tohoku University), Hiroaki Watanabe, M.D. (Department of Palliative Care, Komaki City Hospital), Takuya Odagiri, M.D. (Department of Palliative Care, Komaki City Hospital), Tetsuya Ito, M.D.,Ph.D. (Department of Palliative Care, Japanese Red Cross Medical Center), Masayuki Ikenaga, M.D. (Hospice, Yodogawa Christian Hospital), Keiji Shimizu, M.D., Ph.D. (Department of Palliative Care Internal Medicine, Osaka General Hospital of West Japan Railway Company), Akira Hayakawa, M.D., Ph.D. (Hospice, Yodogawa Christian Hospital), Rena Kamura, M.D. (Hospice, Yodogawa Christian Hospital), Takeru Okoshi, M.D., Ph.D. (Okoshi Nagominomori Clinic), Tomohiro Nishi, M.D. (Kawasaki Municipal Ida Hospital, Kawasaki Comprehensive Care Center), Kazuhiro Kosugi, M.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yasuhiro Shibata, M.D. (Kawasaki Municipal Ida Hospital, Kawasaki Comprehensive Care Center), Takayuki Hisanaga, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Takahiro Higashibata, M.D., Ph.D. (Department of General Medicine and Primary Care, Palliative Care Team, University of Tsukuba Hospital), Ritsuko Yabuki, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Shingo Hagiwara, M.D., Ph.D. (Department of Palliative Medicine, Yuai Memorial Hospital), Miho Shimokawa, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Satoshi Miyake, M.D., Ph.D. (Professor, Department of Clinical Oncology Graduate School of Medical and Dental Sciences Tokyo Medical and Dental University (TMDU)), Junko Nozato, M.D. (Specially Appointed Assistant Professor, Department of Internal Medicine, Palliative Care, Medical Hospital, Tokyo Medical and Dental University), Hiroto Ishiki, M.D. (Department of Palliative Medicine, National Cancer Center Hospital), Tetsuji Iriyama, M.D. (Specially Appointed Assistant Professor, Department of Internal Medicine, Palliative Care, Medical Hospital, Tokyo Medical and Dental University), Keisuke Kaneishi, M.D., Ph.D. (Department of Palliative Care Unit, JCHO Tokyo Shinjuku Medical Center), Mika Baba, M.D., Ph.D. (Department of Palliative medicine Suita Tokushukai Hospital), Tomofumi Miura, M.D., Ph.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yoshihisa Matsumoto, M.D., Ph.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Ayumi Okizaki, Ph.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yuki Sumazaki Watanabe, M.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yuko uehara, M.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Eriko Satomi, M.D. (Department of palliative medicine, National Cancer Center Hospital), Kaoru Nishijima, M.D. (Department of Palliative Medicine, Kobe University Graduate School of Medicine), Junichi Shimoinaba, M.D. (Department of Hospice Palliative Care, Eikoh Hospital), Ryoichi Nakahori, M.D. (Department of Palliative Care, Fukuoka Minato Home Medical Care Clinic), Takeshi Hirohashi, M.D. (Eiju General Hospital), Jun Hamano, M.D., Ph.D. (Assistant Professor, Faculty of Medicine, University of Tsukuba), Natsuki Kawashima, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Takashi Kawaguchi, Ph.D. (Tokyo University of Pharmacy and Life Sciences Department of Practical Pharmacy), Megumi Uchida, M.D., Ph.D. (Dept. of Psychiatry and Cognitive-Behavioral Medicine, Nagoya City University Graduate School of Medical Sciences), Ko Sato, M.D., Ph.D. (Hospice, Ise Municipal General Hospital), Yoichi Matsuda, M.D., Ph.D. (Department of Anesthesiology & Intensive Care Medicine / Osaka University Graduate School of Medicine), Yutaka Hatano, M.D., Ph.D. (Hospice, Gratia Hospital), Satoru Tsuneto, M.D., Ph.D. (Professor, Department of Human Health Sciences, Graduate School of Medicine, Kyoto University Department of Palliative Medicine, Kyoto University Hospital), Sayaka Maeda, M.D. (Department of Palliative Medicine, Kyoto University Hospital), Yoshiyuki Kizawa M.D., Ph.D., FJSIM, DSBPMJ. (Designated Professor and Chair, Department of Palliative Medicine, Kobe University School of Medicine), Hiroyuki Otani, M.D. (Palliative Care Team, and Palliative and Supportive Care, National Kyushu Cancer Center), Isseki Maeda, MD., Ph.D. (Department of Palliative Care, Senri-Chuo Hospital).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Tomoo Ikari: conceptualization, project implementation writing draft, and writing review and editing.
Yusuke Hiratsuka: conceptualization, project administration, formal analysis, data curation, methodology, investigation, writing draft, and writing review and editing.
Shao-Yi Cheng: investigation, supervision and writing review and editing.
Mitsunori Miyashita: supervision and writing review and editing.
Tatsuya Morita: investigation, supervision and writing review and editing.
Masanori Mori: conceptualization, investigation, methodology, project administration, resources, supervision, and writing review and editing.
Yu Uneno: investigation and writing review and editing.
Koji Amano: investigation and writing review and editing.
Yuko Uehara: investigation and writing review and editing.
Takashi Yamaguchi: investigation and writing review and editing.
Isseki Maeda: investigation and writing review and editing.
Akira Inoue: investigation and writing review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the ethical standards of the Declaration of Helsinki. The ethical guidelines for medical and health research involving human subjects presented by the Japanese Ministry of Health, Labor, and Welfare, and were approved by the local Institutional Review Boards of all participating institutions. Japanese law does not require individual informed consent from participants in a non-invasive observational trial such as the present study.
Consent to participate
We used an opt-out method rather than acquiring written or oral informed consent; all patients could find information on the study through the instructions posted on the ward or institutional website, and they had the opportunity to decline participation.
Consent for publication
All authors read and approved the final manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key message
The multicenter prospective cohort study identified five factors associated with good death in patients admitted to palliative care units; preferred place of death at palliative care units, longer survival time, not sudden death, better spiritual well-being in the last 3 days in life, and better communication between patient and family.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ikari, T., Hiratsuka, Y., Cheng, SY. et al. Factors associated with good death of patients with advanced cancer: a prospective study in Japan. Support Care Cancer 30, 9577–9586 (2022). https://doi.org/10.1007/s00520-022-07363-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07363-1