Abstract
Purpose
The aim of this systematic review was to investigate the clinical effectiveness of glass ionomer cements (GICs) compared to other restorative materials in the treatment of radiation-related caries.
Methods
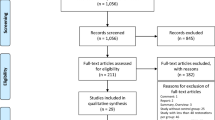
Two independent researchers searched literature databases (PubMed, Scopus, Web of Science, Cochrane Library, Lilacs/BBO) and the grey literature to identify clinical trials that compared GICs with other restorative materials for the treatment of radiation-related caries. The clinical criteria considered for the performance of the restorations were based on the parameters of marginal adaptation/anatomical form, secondary caries, retention, and cumulative failures of the restorations. The methodological quality and risk of bias were evaluated using the Cochrane Collaboration tool.
Results
From a total of 511, only four articles fulfilled the inclusion criteria. Conventional GIC restorations presented higher marginal adaptation failures than the resin-modified glass ionomer cements (RM-GICs) and composite restorations in all of the follow-up periods. Secondary caries was not observed in conventional GIC restorations throughout the follow-up periods, in three out of four of the included studies. RM-GICs and composite restorations showed significantly lower cumulative failure rates than conventional GICs at 6-, 12-, and 18-month follow-ups.
Conclusion
Due to insufficient scientific evidence, it was not possible to conclude that GICs are more effective than other restorative materials for the treatment of radiation-related caries.


Similar content being viewed by others
Data availability
The data used in this systematic review are publicly available and included in the manuscript.
Code availability
Not applicable.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/CAAC.21660
Semrau R (2017) The role of radiotherapy in the definitive and postoperative treatment of advanced head and neck cancer. Oncol Res Treat 40:347–352. https://doi.org/10.1159/000477128
Xiao C, Hanlon A, Zhang Q et al (2013) Symptom clusters in patients with head and neck cancer receiving concurrent chemoradiotherapy. Oral Oncol 49:360–366. https://doi.org/10.1016/j.oraloncology.10.004
Sroussi HY, Epstein JB, Bensadoun R-J et al (2017) Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med 6:2918–2931. https://doi.org/10.1002/cam4.1221
Elad S, Zadik Y, Yarom N (2017) Oral complications of nonsurgical cancer therapies. Atlas Oral Maxillofac Surg Clin North Am 25:133–147. https://doi.org/10.1016/J.CXOM.2017.04.006
Moore C, McLister C, Cardwell C, et al. (2020) Dental caries following radiotherapy for head and neck cancer: a systematic review. Oral Oncol 100:104484. https://doi.org/10.1016/j.oraloncology.2019.104484
Aguiar GP, Jham BC, Magalhães CS et al (2009) A review of the biological and clinical aspects of radiation caries. J Contemp Dent Pract 10:83–89
de Miranda RR, Silva ACA, Dantas NO et al (2019) Chemical analysis of in vivo–irradiated dentine of head and neck cancer patients by ATR-FTIR and Raman spectroscopy. Clin Oral Investig 23:3351–3358. https://doi.org/10.1007/s00784-018-2758-6
Madrid CC, de Pauli PM, Line SR et al (2017) Structural analysis of enamel in teeth from head-and-neck cancer patients who underwent radiotherapy. Caries Res 51:119–128. https://doi.org/10.1159/000452866
Velo MMAC, Farha ALH, da Silva Santos PS et al (2018) Radiotherapy alters the composition, structural and mechanical properties of root dentin in vitro. Clin Oral Investig 22:2871–2878. https://doi.org/10.1007/S00784-018-2373-6
Gupta N, Pal M, Rawat S et al (2015) Radiation-induced dental caries, prevention and treatment - a systematic review. Natl J Maxillofac Surg 6:160–166. https://doi.org/10.4103/0975-5950.183870
Hong CHL, Napeñas JJ, Hodgson BD et al (2010) A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer 18:1007–1021. https://doi.org/10.1007/s00520-010-0873-2
Yamagata K, Onizawa K, Yanagawa T et al (2006) A prospective study to evaluate a new dental management protocol before hematopoietic stem cell transplantation. Bone Marrow Transplant 38:237–242. https://doi.org/10.1038/sj.bmt.1705429
Palmier NR, Migliorati CA, Prado-Ribeiro AC et al (2020) Radiation-related caries: current diagnostic, prognostic, and management paradigms. Oral Surg Oral Med Oral Pathol Oral Radiol 130:52–62. https://doi.org/10.1016/j.oooo.2020.04.003
Hu JY, Chen XC, Li YQ et al (2005) Radiation-induced root surface caries restored with glass-ionomer cement placed in conventional and ART cavity preparations: results at two years. Aust Dent J 50:186–190
Mickenautsch S, Mount G, Yengopal V (2011) Therapeutic effect of glass-ionomers: an overview of evidence. Aust Dent J 56:10–15. https://doi.org/10.1111/j.1834-7819.2010.01304.x
Moberg M, Brewster J, Nicholson J, Roberts H (2019) Physical property investigation of contemporary glass ionomer and resin-modified glass ionomer restorative materials. Clin Oral Investig 23:1295–1308. https://doi.org/10.1007/s00784-018-2554-3
Ferracane JL (2011) Resin composite - state of the art. Dent Mater 27:29–38
Ilie N, Hickel R (2011) Resin composite restorative materials. Aust Dent J 56:59–66. https://doi.org/10.1111/j.1834-7819.2010.01296.x
Sarrett DC (2005) Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent Mater 21:9–20. https://doi.org/10.1016/j.dental.2004.10.001
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Wood RE, Maxymiw WG, McComb D (1993) A clinical comparison of glass ionomer (polyalkenoate) and silver amalgam restorations in the treatment of class 5 caries in xerostomic head and neck cancer patients. Oper Dent 18:94–102
Hu JY, Li YQ, Smales RJ, Yip KHK (2002) Restoration of teeth with more-viscous glass ionomer cements following radiation-induced caries. Int Dent J 52:445–448
McComb D, Erickson RL, Maxymiw WG, Wood RE (2002) A clinical comparison of glass ionomer, resin-modified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Oper Dent 27:430–437
De Moor RJG, Stassen IG, van ’t Veldt Y, et al (2011) Two-year clinical performance of glass ionomer and resin composite restorations in xerostomic head- and neck-irradiated cancer patients. Clin Oral Investig 15:31–38. https://doi.org/10.1007/s00784-009-0355-4
Silva ARS, Alves FA, Berger SB et al (2010) Radiation-related caries and early restoration failure in head and neck cancer patients. A polarized light microscopy and scanning electron microscopy study. Support care cancer Off J Multinatl Assoc Support Care Cancer 18:83–87. https://doi.org/10.1007/s00520-009-0633-3
Silva ARS, Alves FA, Antunes A et al (2009) Patterns of demineralization and dentin reactions in radiation-related caries. Caries Res 43:43–49. https://doi.org/10.1159/000192799
Soares CJ, Castro CG, Neiva NA et al (2010) Effect of gamma irradiation on ultimate tensile strength of enamel and dentin. J Dent Res 89:159–164. https://doi.org/10.1177/0022034509351251
Naves LZ, Novais VR, Armstrong SR et al (2012) Effect of gamma radiation on bonding to human enamel and dentin. Support care cancer Off J Multinatl Assoc Support Care Cancer 20:2873–2878. https://doi.org/10.1007/s00520-012-1414-y
Reed R, Xu C, Liu Y et al (2015) Radiotherapy effect on nano-mechanical properties and chemical composition of enamel and dentine. Arch Oral Biol 60:690–697. https://doi.org/10.1016/j.archoralbio.2015.02.020
de Barros da Cunha SR, Ramos PAMM, Haddad CMK, et al (2016) Effects of different radiation doses on the bond strengths of two different adhesive systems to enamel and dentin. J Adhes Dent 18:151–156. https://doi.org/10.3290/j.jad.a35841
Rodrigues RB, Soares CJ, Junior PCS et al (2018) Influence of radiotherapy on the dentin properties and bond strength. Clin Oral Investig 22:875–883. https://doi.org/10.1007/S00784-017-2165-4
Galetti R, Santos-Silva AR, oge., Antunes AN ogueir. da G, et al (2014) Radiotherapy does not impair dentin adhesive properties in head and neck cancer patients. Clin Oral Investig 18:1771–1778. https://doi.org/10.1007/s00784-013-1155-4
Bajwa NK, Pathak A (2014) Change in surface roughness of esthetic restorative materials after exposure to different immersion regimes in a cola drink. ISRN Dent 2014:1–6. https://doi.org/10.1155/2014/353926
Antonson SA, Yazici AR, Kilinc E et al (2011) Comparison of different finishing/polishing systems on surface roughness and gloss of resin composites. J Dent 39(Suppl 1):e9–17. https://doi.org/10.1016/j.jdent.2011.01.006
Alghilan MA, Blaine Cook N, Platt JA et al (2015) Susceptibility of restorations and adjacent enamel/dentine to erosion under different salivary flow conditions. J Dent 43:1476–1482. https://doi.org/10.1016/j.jdent.2015.10.007
Brito CR, Velasco LG, Bonini GA et al (2010) Glass ionomer cement hardness after different materials for surface protection. J Biomed Mater Res A 93:243–246. https://doi.org/10.1002/JBM.A.32524
Neelakantan P, John S, Anand S et al (2011) Fluoride release from a new glass-ionomer cement. Oper Dent 36:80–85. https://doi.org/10.2341/10-219-LR
Seppä L, Forss H, Øgaard B (1993) The effect of fluoride application on fluoride release and the antibacterial action of glass lonomers. J Dent Res 72:1310–1314. https://doi.org/10.1177/00220345930720090901
Preston AJ, Higham SM, Agalamanyi EA, Mair LH (1999) Fluoride recharge of aesthetic dental materials. J Oral Rehabil 26:936–940. https://doi.org/10.1046/J.1365-2842.1999.00502.X
Kumari PD, Khijmatgar S, Chowdhury A et al (2019) Factors influencing fluoride release in atraumatic restorative treatment (ART) materials: a review. J Oral Biol Craniofacial Res 9:315–320
Thariat J, Ramus L, Darcourt V et al (2012) Compliance with fluoride custom trays in irradiated head and neck cancer patients. Support Care Cancer 20:1811–1814. https://doi.org/10.1007/S00520-011-1279-5
Sohn HO, Park EY, Jung YS et al (2021) Effects of the professional oral care management program on patients with head and neck cancer after radiotherapy: a 12-month follow-up. J Dent Sci 16:453–459. https://doi.org/10.1016/j.jds.2020.09.010
Piwowarczyk A, Ottl P, Lauer HCBA (2002) Laboratory strength of glass ionomer cement, compomers, and resin composites. J Prosthodont 11:86–91
Yap AU, Cheang PHCP (2002) Mechanical properties of two restorative reinforced glass-ionomer cements. J Oral Rehabil 29:682–688. https://doi.org/10.1046/J.1365-2842.2002.00908.X
Iazzetti G, Burgess J, Gardiner D (2001) Selected mechanical properties of fluoride-releasing restorative materials. Oper Dent 26:21–26
Mc Lean JW (1994) Evolution of glass-ionomer cements: a personal view. J Esthet Dent 6:195–206. https://doi.org/10.1111/J.1708-8240.1994.TB00860.X
Francois P, Fouquet V, Attal JP, Dursun E (2020) Commercially available fluoride-releasing restorative materials: a review and a proposal for classification. Materials (Basel) 13:2313. https://doi.org/10.3390/ma13102313
Yap AU, Wattanapayungkul P, Chung SM (2003) Influence of the polymerization process on composite resistance to chemical degradation by food-simulating liquids. Oper Dent 28:723–727
Nomoto R, McCabe JF (2001) Effect of mixing methods on the compressive strength of glass ionomer cements. J Dent 29:205–210. https://doi.org/10.1016/S0300-5712(01)00010-0
Dowling AH, Fleming GJP (2009) Are encapsulated anterior glass-ionomer restoratives better than their hand-mixed equivalents? J Dent 37:133–140. https://doi.org/10.1016/j.jdent.2008.10.006
Al-Taee L, Deb S, Banerjee A (2020) An in vitro assessment of the physical properties of manually- mixed and encapsulated glass-ionomer cements. BDJ Open 6:12. https://doi.org/10.1038/s41405-020-0040-x
Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P (1996) Atraumatic restorative treatment (ART): rationale, technique, and development. J Public Health Dent 56(3 Spec No):135–140. https://doi.org/10.1111/j.1752-7325.1996.tb02423.x
Schriks MCM, Van Amerongen WE (2003) Atraumatic perspectives of ART: Psychological and physiological aspects of treatment with and without rotary instruments. Community Dent Oral Epidemiol 31:15–20
Molina GF, Faulks D, Mazzola I et al (2018) Three-year survival of ART high-viscosity glass-ionomer and resin composite restorations in people with disability. Clin Oral Investig 22:461–467. https://doi.org/10.1007/s00784-017-2134-y
Molina GF, Faulks D, Mulder J, Frencken JE (2019) High-viscosity glass-ionomer vs. composite resin restorations in persons with disability: five-year follow-up of clinical trial. Braz Oral Res 33:e099. https://doi.org/10.1590/1807-3107BOR-2019.VOL33.0099
Moshaverinia M, Navas A, Jahedmanesh J et al (2019) Comparative evaluation of the physical properties of a reinforced glass ionomer dental restorative material. J Prosthet Dent 122:154–159. https://doi.org/10.1016/J.PROSDENT.2019.03.012
Author information
Authors and Affiliations
Contributions
Jullyana M. P. Dezanetti, Bruna L. do Nascimento, and Juliana S. R. Orsi performed the systematic review methodology process. Jullyana M. P. Dezanetti and Evelise M. Souza designed the study and wrote the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dezanetti, J.M.P., Nascimento, B.L., Orsi, J.S.R. et al. Effectiveness of glass ionomer cements in the restorative treatment of radiation-related caries — a systematic review. Support Care Cancer 30, 8667–8678 (2022). https://doi.org/10.1007/s00520-022-07168-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07168-2