Abstract
Purpose
The availability of psychosocial support measures has a significant impact on the quality of life of terminally ill and dying patients and the burden experienced by their relatives. To date, no intervention has specifically focused on promoting interaction within the dyads of the following: (1) terminally ill adult children and their parents and (2) terminally ill parents and their adult children. A national Delphi study was conducted to provide appropriate recommendations for dyadic psychosocial support measures.
Methods
Recommendations were formulated from qualitative interview data on the experiences and wishes of patients and family caregivers within these two dyads. Experts from palliative and hospice care providers rated the relevance and feasibility of 21 recommendations on two 4-point Likert-type scales, respectively. Additional suggestions for improvement were captured via free text fields. Individual items were considered consented when ≥ 80% of participants scored 1 (strongly agree) or 2 (somewhat agree) regarding both relevance and feasibility.
Results
A total of 27 experts (35% response rate) completed two Delphi rounds. Following the first round, 13 recommendations were adjusted according to participants’ comments. After the second round, consensus was achieved for all 21 of the initially presented recommendations.
Conclusion
The Delphi-consented recommendations for parents and adult children at the end of life provide the first guidance for hands-on dyadic psychosocial support measures for parent–adult child relationships, specifically. The next step could involve the structured implementation of the recommendations, accompanied by scientific research.
This study was registered on October 27, 2017, with the German Clinical Trials Register (DRKS00013206).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and background
In our aging society, the number of people facing terminal illness with a limited life span is increasing. Within families, parents are increasingly faced with the challenge of caring for an adult child with terminal illness; likewise, adult children are continuing to cope with the limited life span of their aging parents. In the context of terminal illness, both the family setting and the interaction between patients and relatives have a vital impact on the quality of life of patients and the burden experienced by their relatives. Furthermore, the quality of life of patients and caregivers is associated with the availability of psychosocial support; when the development or availability of such measures is lacking, needs are often unmet [1,2,3,4,5,6,7,8]. In general, patients and caregivers—as well as specific subsets of patients and caregivers—are likely to have very different psychosocial needs [6, 9]. For this reason, it is necessary to develop supportive interventions tailored to specific populations [1, 7].
Regarding the desired levels of support in managing end-of-life situations, both adult child caregivers and the parents of ill adult children seek information on the patient’s illness and perceive such information as helpful, because it enables them to take some control over the situation [10,11,12,13]. The term “caregiver” is used in this article in a broad sense, encompassing family members who provide practical and/or emotional support. The literature highlights the importance of family-specific patterns of communication [14]. Exchange with other caregivers [15], friends, and family members about feelings and events, as well as professional psychosocial support, have been shown to be valued by parent caregivers of adult children [10]. Research has also demonstrated the role of psychosocial support interventions in opening dialogue between terminally ill parents and their adult children [16]. Furthermore, the exchange of happy memories has been found to help patients find peace when nearing death [17,18,19]. Finally, one of the few studies on long-distance adult child caregivers for their dying parents demonstrated that feelings of guilt were powerful and needed to be addressed [20].
Several dyadic psychosocial interventions for patients with life-limiting illnesses and their caregivers have been developed [21,22,23,24,25]. Many of these interventions have involved patients’ significant others, to beneficial effect. For instance, Moon and Adams [26] showed, in their literature review, that relationship quality, well-being, and quality of life improved following a dyadic intervention for early dementia patients and their caregivers. Nezu et al. [27] also reported positive effects for a problem-solving therapy intervention for distressed adult cancer patients and their significant others, including improvements in their relationship, quality of life, and coping ability. However, none of these interventions specifically focused on promoting interaction within dyads of adult children and parents in end-of-life situations.
Research question
The aim of the Delphi study was to provide practical recommendations for dyadic psychosocial support measures for the following: (1) terminally ill adult children and their parent caregivers and (2) terminally ill parents and their adult child caregivers. These recommendations were intended to support professionals and voluntary workers in inpatient and ambulatory hospice and palliative care providers.
Methods
Design
To develop and provide high-quality support for terminally ill and dying patients and their relatives, the specific needs of all parties must be known. The project “Dy@EoL—interaction at the end of life in dyads of parents and adult children” [28] formulated recommendations on the basis of empirical data on the experiences and desires of patients and family caregivers in each dyad.
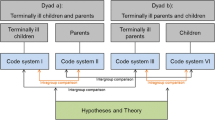
Three methodological steps were taken to formulate these recommendations (Fig. 1):
-
(I)
Three core themes regarding parent–adult child interaction at the end of life emerged from the Dy@EoL qualitative interviews with parents and adult children in dyads 1 and 2 (February 2018 to November 2019): (1) relationship with the dyad partner [29], (2) communication and information [30], and (3) support and relief [31]. Individual hypotheses (N = 22) describing the interaction specifics of parents and adult children at the end of life were derived from these empirical data for the three subject areas.
-
(II)
For the 22 individual hypotheses, the project team formulated recommendations for practical dyadic psychosocial support measures via written feedback and a workshop involving the project’s advisory board. The developed recommendations were pre-tested by one psychologist/palliative care researcher (S.S.; March to June 2020).
-
(III)
The recommendations were reviewed using a national Delphi process (June to July 2020). The aim of the Delphi process was the following: (a) evaluate the individual recommendations according to their relevance and feasibility in everyday hospice and palliative care practice and (b) sharpen the wording. The Delphi technique was employed because it enables consensus to be achieved from a wide range of knowledgeable participants when face-to-face discussion is unfeasible [32,33,34,35,36,37,38]. In total, 21 recommendations were presented, of which (a) 5 specifically addressed dyad 1, (b) 11 specifically addressed dyad 2, and (c) 5 pertained to both dyads. In the Delphi survey, each recommendation was presented alongside its associated hypothesis, as recommendations can only be fully understood in the context of their underlying logic. Experts were invited by e-mail to participate in the survey. The Delphi survey was designed and administered anonymously online, using the software EvaSys V8.0 (Electric Paper Evaluationssysteme GmbH, Lüneburg, Germany). Experts rated the relevance and feasibility (with respect to the provision of care) of each recommendation on two 4-point Likert-type scales, respectively, ranging from 1 (strongly agree) to 4 (strongly disagree). Experts could also provide open comments and suggestions for improvement in a free text field connected to each recommendation.
Participants
The advisory board consisted of 15 palliative care representatives from the fields of medicine, psycho(onco)logy, pastoral care, nursing, social work, and bereavement care, as well as hospice and palliative care networks. The invited experts (n = 77) for the Delphi study comprised advisory board members, all tenured professors for palliative medicine in Germany, and further representatives from palliative and/or hospice care, including researchers with expertise in parent–adult child interaction at the end of life. All experts were informed of the nature and aim of the study in an e-mail that included the link to the Delphi survey. The experts participated voluntarily and were not compensated for their participation; however, they were invited to participate in a draw of three 50€ vouchers for an online store.
Data processing and analyses
All free text comments collected from the Delphi study were independently analyzed by two researchers (F.A.H., L.G.) and used to refine the individual recommendations. Quantitative data from the survey were exported to Microsoft Excel 2010 and IBM SPSS Statistics 26 (SPSS Inc., Chicago, IL, USA), for the purpose of descriptive analysis. The Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care checklist [39] was used to ensure comprehensive reporting of the Delphi study.
In accordance with similar studies [36, 40, 41], each recommendation was considered consented when ≥ 80% of participants scored the item 1 (strongly agree) or 2 (somewhat agree) for both relevance and feasibility. Although the Delphi method does not require items that achieve a high level of agreement in the first round to be added to the second round [42], in the present study, the authors (F.A.H., L.G.) included some items with an initial high rating in the second round because the experts provided valuable free text comments that the authors wished to incorporate.
Results
Sample characteristics
For Delphi round 1, 77 experts were invited to participate, and 43% took part (n = 33/77). These 33 respondents were also asked to participate in the second round. In round 2, 82% of the invited participants (n = 27/33) completed the survey. Thus, the final response rate was 35% (n = 27/77) (see Table 1 for participants’ socio-demographic characteristics).
Consensus on recommendations
Delphi round 1
In Delphi round 1, 19 out of 21 (90.5%) of the presented recommendations achieved consensus with respect to both assessment criteria. The panelists disagreed on 2 (9.5%) items, and these items were adjusted for the second Delphi round according to participants’ free text comments (see Table 2).
For the first core theme, “relationship with dyad partner,” all recommendations except for R-1.5 achieved consensus in both evaluation criteria (see Table 3 on levels of agreement). R-1.5 achieved consensus with respect to relevance for everyday practice, but only 75.8% consensus in terms of feasibility. Participant feedback indicated concern that the actors who would be tasked with realizing this recommendation were not specified. Furthermore, the limited time involved in end-of-life situations was seen to hinder the suggested biography work. Finally, participants commented that they were missing information on how the ill parent and adult child caregiver would be supported in allowing and voicing accusations from and towards the dyadic other.
With respect to the second core theme, “communication and information,” one (R-2.5) of the six recommendations only achieved 75.8% approval with respect to feasibility and, thus, did not achieve consensus in the first round. Participants endorsed the inclusion of an explanation that psychosocial support would only be offered when family communication patterns were perceived as burdensome and the patient and/or caregiver expressed a need for change. Depending on the situation, only one dyad partner or both dyad partners would be offered support.
All recommendations for the third core theme, “support and relief,” achieved consensus with respect to both evaluation criteria.
In addition to the unconsented recommendations R-1.5 and R-2.5, 11 (R-1.1, R-1.2. R-1.3, R-1.4, R-1.6, R-2.1, R-2.2, R.2.4, R-2.6, R-3.7, R-3.9) of the 19 consented recommendations were adapted for the second Delphi round, in order to incorporate participants’ valuable feedback for improvement.
Participants’ suggestions regarding the first core theme, “relationship with dyad partner” (R-1.1, R-1.2. R-1.3, R-1.4, R-1.6), primarily pertained to exploring the experience of losing a loved one, non-judgmental responding to patients’ and family caregivers’ perceptions of their relationship, and the potential opportunities involved in exploring role reversal and individual needs.
Regarding the second core theme, “communication and information” (R-2.2, R.2.4, R-2.6), participants’ remarks emphasized their need for clarification on the professions of those who would be offering support to patients/caregivers, particularly with respect to supporting patients/caregivers in accepting that communication may change in the terminal illness situation and that, at some point, patients may not wish to talk about dying and death.
Only two recommendations pertaining to the third core theme, “support and relief” (R-3.7, R-3.9), were included in the second Delphi round. Participants’ strongest suggestions were to support caregiving adult children in developing different attitudes towards their feelings of guilt around their limited ability to care for their ill parents and to elicit additional resources to help patients and caregivers.
Some comments cut across the individual recommendations and were incorporated into an introductory text that framed the recommendations. These comments concerned the importance of considering individual differences between patients (with respect to, e.g., their expected remaining lifetime and perceptions of what is burdensome), the application of the recommendations only when patients/caregivers expressed a need for action, the framework conditions in which the recommendations would be applied (e.g. ambulatory vs. inpatient settings), and clarification that the recommendations were directed at psychosocial professionals, palliative care teams, and family doctors.
Delphi round 2
Thirteen recommendations (R-1.1, R-1.2, R-1.3, R-1.4, R-1.5, R-1.6, R-2.1, R-2.2, R.2.4, R-2.5, R-2.6, R-3.7, R-3.9) were modified according to participants’ comments (see Appendix 1 for the consented Delphi statements) and presented in the second Delphi round. All of these recommendations achieved consensus, with an average agreement rate of 98% and 94% regarding relevance and feasibility, respectively. Hence, consensus on all 21 recommendations was achieved within the two-round Delphi process; none of the initial recommendations was dropped.
Discussion
In this Delphi study, we consented 21 recommendations for psychosocial measures to support interaction within two adult child–parent dyads. The majority of the recommendations were immediately consented in the first round, and all achieved ≥ 80% agreement regarding their relevance. We suggest that this result is due to the methodological approach of the Dy@EoL project: hypotheses were deduced from interviews with affected parents and adult children in both dyads. In addition, the recommendations were developed in collaboration with an advisory board and grounded in participants’ clinical practice. Several lines of evidence have suggested that fit, relevance, and quality of research can be enhanced by involving those for whom the support measures are designed and those who will be tasked with their delivery [43,44,45].
The agreement on feasibility was relatively lower, with two recommendations not consented in the first round but achieving consensus in the second. The partial lack of specification of the professional groups (e.g., palliative care teams, psycho-oncologists, or family doctors) at whom the recommendations were directed and who would administer the recommended measures as well as the limited time involved in end-of-life situations were perceived as limiting factors for implementation in palliative and hospice care practice. All other recommendations gained approval in the first round. We argue that this is due to the fact that our recommendations had a “modest aim” [1]: they did not describe a comprehensive intervention program but instead represented practical tips for multi-professional palliative care teams to better support adult child–parent dyads at the end of life. The Delphi survey was necessary to close the remaining gap between research and practice. Overall, research and practice dovetailed in the project, and apparently, this had a positive effect on the consensus-building process.
Strengths and limitations
Current psychosocial support measures represent an important aspect of hospice and palliative care. The recommendations developed in the present study provide additional guidance for the specific situations faced by parents and adult children at the end of life. These recommendations are not to be understood as guidelines, but rather practical, hands-on support. The recommendations were specifically developed for application in ambulatory and inpatient German healthcare contexts. This may limit the generalizability of the results to other countries. Furthermore, the application and scope of the recommendations depend on the life expectancy of the patient and the accompanying caregiving period. In the context of longer caregiving periods, it may be useful to repeatedly assess patients’ and relatives’ feelings of burden and support needs. A further limiting factor of the present study is the relatively low response rate (35%). Nevertheless, participants’ clinical expertise, long-standing experience, and multi-professionalism represent an absolute strength. The number of experts from psychosocial professions participating in the Delphi survey was particularly high. These participants may feel more addressed than other experts as recommendations explicitly present psychosocial support. Reasons for non-participation and dropout could not be gleaned.
Conclusions
Interview data from the Dy@EoL study supported previous findings on support experiences and needs in end-of-life situations within dyads of parents and adult children [10, 16,17,18,19,20] and revealed further dyad-specific experiences and needs. The consented recommendations in the described Delphi study present the first practical support grounded in empirical data collected from parents and adult children within both patient–caregiver dyads for managing their psychosocial needs. The recommendations provide useful guidance for the development of manifold dyadic psychosocial support measures targeting parent–child relationships, specifically. The German recommendations were published as a pocket-sized brochure, in cooperation with the German Association for Palliative Medicine [46], and are freely accessible online for application in healthcare practice. The next step could involve the structured implementation of the recommendations, accompanied by scientific research.
Data availability
The datasets analyzed in this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Change history
07 November 2021
Updated due to the missing funding information.
References
Harding R, Higginson IJ (2003) What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness. Palliat Med 17(1):63–74. https://doi.org/10.1191/0269216303pm667oa
Osse BHP, Vernooij-Dassen MJFJ, Schadé E, Grol RPTM (2006) Problems experienced by the informal caregivers of cancer patients and their needs for support. Cancer Nurs 29(5):378–388. https://doi.org/10.1097/00002820-200609000-00005
Soothill K, Morris SM, Thomas C, Harman JC, Francis B, McIllmurray MB (2003) The universal, situational, and personal needs of cancer patients and their main carers. Eur J Oncol Nurs 7(1):5–13. https://doi.org/10.1054/ejon.2002.0226
Roberts KE, Panjwani AA, Marziliano A, Applebaum AJ, Lichtenthal WG (2018) End-of-life care and cancer: psychosocial needs of patients and the bereaved. In: Hopewood P, Milroy MJ (eds) Quality cancer care: survivorship before, during and after treatment. Springer, Cham, pp 243–268
Oechsle K, Ullrich A, Marx G, Benze G, Heine J, Dickel L-M, Zhang Y, Wowretzko F, Wendt KN, Nauck F, Bokemeyer C, Bergelt C (2019) Psychological burden in family caregivers of patients with advanced cancer at initiation of specialist inpatient palliative care. BMC Palliat Care 18(1):102. https://doi.org/10.1186/s12904-019-0469-7
Aoun SM, Deas K, Howting D, Lee G (2015) Exploring the support needs of family caregivers of patients with brain cancer using the CSNAT: a comparative study with other cancer groups. PLoS ONE 10(12):e0145106. https://doi.org/10.1371/journal.pone.0145106
Williams A-l, Bakitas M (2012) Cancer family caregivers: A new direction for interventions. J Palliat Med 15(7):775–783. https://doi.org/10.1089/jpm.2012.0046
Teo I, Baid D, Ozdemir S, Malhotra C, Singh R, Harding R, Malhotra R, Yang MG, Neo SH-S, Cheung YB, Neo PSH, Kanesvaran R, Kumarakulasinghe NB, Lee LH, Koh GCH, Finkelstein EA (2020) Family caregivers of advanced cancer patients: self-perceived competency and meaning-making. BMJ Support Palliat Care 10(4):435–442. https://doi.org/10.1136/bmjspcare-2019-001979
Clayton JM, Butow PN, Tattersall MHN (2005) The needs of terminally ill cancer patients versus those of caregivers for information regarding prognosis and end-of-life issues. Cancer 103(9):1957–1964. https://doi.org/10.1002/cncr.21010
Benkel I, Molander U (2015) Parents’ experiences of when an adult child is seriously ill—“it does not matter that it is a grown-up person, they are still your child.” J Health Sci 3:165–173. https://doi.org/10.17265/2328-7136/2015.04.005
Benkel I, Molander U (2017) A qualitative study of the experiences of parents with an adult child who has a severe disease: existential questions will be raised. Inquiry-J Health Care Organ Provis Financ 54. https://doi.org/10.1177/0046958017727107
Herbst FA, Gawinski L, Schneider N, Stiel S (2019) Adult child-parent dyadic interactions at the end of life: a scoping review. BMJ Support Palliat Care 10(2):175–185. https://doi.org/10.1136/bmjspcare-2019-001894
Mazanec P, Daly BJ, Ferrell BR, Prince-Paul M (2011) Lack of communication and control: experiences of distance caregivers of parents with advanced cancer. Oncol Nurs Forum 38(3):307–313. https://doi.org/10.1188/11.ONF.307-313
Dean M, McClement S, Bond JB Jr, Daeninck PJ, Nelson F (2005) Parental experiences of adult child death from cancer. J Palliat Med 8(4):751–765. https://doi.org/10.1089/jpm.2005.8.751
Poindexter CC (2002) “Twists and turns”: case study of an HIV caregiving journey. J HIV/AIDS Soc Serv 1(1):113–135. https://doi.org/10.1300/J187v01n01_09
Chan CLW, Ho AHY, Leung PPY, Chochinov HM, Neimeyer RA, Pang SMC, Tse DMW (2012) The blessings and the curses of filial piety on dignity at the end of life: lived experience of Hong Kong Chinese adult children caregivers. J Ethn Cult Divers Soc Work 21(4):277–296. https://doi.org/10.1080/15313204.2012.729177
National Institute on Aging. National Institutes of Health. U.S. Department of Health and Human Services (2016) End of life: helping with comfort and care. https://order.nia.nih.gov/sites/default/files/2017-07/End_of_Life_508.pdf. Accessed 03 Feb 2021
University of Rochester Medical Center (2021) Adult and children's health encyclopedia: hospice or palliative care: management. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=34&contentid=23505-1. Accessed 03 Feb 2021
Egan KA, Horvath GLS (2006) Family caregiving in the last years of life: positive experiences in the midst of suffering. Home Healthc Nurse 24(9):554–558. https://doi.org/10.1097/00004045-200610000-00003
Casañas i Comabella C (2017) Distance caregiving in palliative care: a mixed methods study exploring the role of ehealth. Dissertation, Oxford Brookes University
Badr H, Smith CB, Goldstein NE, Gomez J, Redd WH (2015) Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer 121(1):150–158. https://doi.org/10.1002/cncr.29009
Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, LoRusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T (2013) Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncol 22(3):555–563. https://doi.org/10.1002/pon.3036
von Heymann-Horan A, Bidstrup P, Guldin M-B, Sjøgren P, Andersen EAW, von der Maase H, Kjellberg J, Timm H, Johansen C (2018) Effect of home-based specialised palliative care and dyadic psychological intervention on caregiver anxiety and depression: a randomised controlled trial. Br J Cancer 119(11):1307–1315. https://doi.org/10.1038/s41416-018-0193-8
von Heymann-Horan A, Bidstrup PE, Johansen C, Rottmann N, Andersen EAW, Sjøgren P, von der Maase H, Timm H, Kjellberg J, Guldin M-B (2019) Dyadic coping in specialized palliative care intervention for patients with advanced cancer and their caregivers: Effects and mediation in a randomized controlled trial. Psycho-Oncol 28(2):264–270. https://doi.org/10.1002/pon.4932
von Heymann-Horan AB, Puggaard LB, Nissen KG, Benthien KS, Bidstrup P, Coyne J, Johansen C, Kjellberg J, Nordly M, Sjøgren P, Timm H, von der Maase H, Guldin M-B (2018) Dyadic psychological intervention for patients with cancer and caregivers in home-based specialized palliative care: the Domus model. Palliat Support Care 16(2):189–197. https://doi.org/10.1017/s1478951517000141
Moon H, Adams KB (2012) The effectiveness of dyadic interventions for people with dementia and their caregivers. Dementia 12(6):821–839. https://doi.org/10.1177/1471301212447026
Nezu AM, Nezu CM, Felgoise SH, McClure KS, Houts PS (2003) Project Genesis: Assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol 71(6):1036–1048. https://doi.org/10.1037/0022-006x.71.6.1036
Stiel S, Stelzer E-M, Schneider N, Herbst FA (2018) Exploring end-of-life interaction in dyads of parents and adult children: a protocol for a mixed-methods study. BMC Palliat Care 17(1):68. https://doi.org/10.1186/s12904-018-0322-4
Herbst FA, Gawinski L, Schneider N, Stiel S (2021) “Mums are sacred, and mums don’t die”: a mixed-methods study of adult child-parent dyadic relationships at the end of life. J Psychosoc Oncol. https://doi.org/10.1080/07347332.2021.1902452
Gawinski L, Stiel S, Schneider N, Herbst FA (2021) Communication in dyads of adult children at the end of life with their parents and parents at the end of life with their adult children: findings from a mixed-methods study. Psycho-Oncol. https://doi.org/10.1002/pon.5728
Herbst FA, Gawinski L, Schneider N, Stiel S (2021) “She can’t support me because she’s so old”: a mixed-methods study of support experiences and needs in adult child-parent dyads at the end of life. Omega-J Death Dying. https://doi.org/10.1177/00302228211008748
Jünger S, Payne S, Brearley S, Ploenes V, Radbruch L (2012) Consensus building in palliative care: a Europe-wide Delphi study on common understandings and conceptual differences. J Pain Symptom Manage 44(2):192–205. https://doi.org/10.1016/j.jpainsymman.2011.09.009
De Vet E, Brug J, De Nooijer J, Dijkstra A, De Vries NK (2005) Determinants of forward stage transitions: a Delphi study. Health Educ Res 20(2):195–205. https://doi.org/10.1093/her/cyg111
Biondo PD, Nekolaichuk CL, Stiles C, Fainsinger R, Hagen NA (2008) Applying the Delphi process to palliative care tool development: lessons learned. Support Care Cancer 16(8):935–942. https://doi.org/10.1007/s00520-007-0348-2
Atkinson NL, Gold RS (2001) Online research to guide knowledge management planning. Health Educ Res 16(6):747–763. https://doi.org/10.1093/her/16.6.747
Knighting K, O’Brien MR, Roe B, Gandy R, Lloyd-Williams M, Nolan M, Jack BA (2016) Gaining consensus on family carer needs when caring for someone dying at home to develop the Carers’ Alert Thermometer (CAT): a modified Delphi study. J Adv Nurs 72(1):227–239. https://doi.org/10.1111/jan.12752
McKenna HP (1994) The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs 19(6):1221–1225. https://doi.org/10.1111/j.1365-2648.1994.tb01207.x
Hsu C-C, Sandford B (2007) The Delphi technique: making sense of consensus. Pract Assess Res Eval 12:10. https://doi.org/10.7275/pdz9-th90
Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG (2017) Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med 31(8):684–706. https://doi.org/10.1177/0269216317690685
Sullivan R, Ugalde A, Sinclair C, Breen LJ (2019) Developing a research agenda for adult palliative care: a modified Delphi study. J Palliat Med 22(5):480–488. https://doi.org/10.1089/jpm.2018.0462
Klietz M, Berndt JM, Wegner F, Schneider N, Höglinger GU, Eggers C, Stiel S (2020) Consensus-based recommendations for advance directives of people with Parkinson’s disease in regard to typical complications by German movement disorder specialists. J Clin Med 9(2):449. https://doi.org/10.3390/jcm9020449
Woitha K, Van Beek K, Ahmed N, Jaspers B, Mollard JM, Ahmedzai SH, Hasselaar J, Menten J, Vissers K, Engels Y (2014) Validation of quality indicators for the organization of palliative care: a modified RAND Delphi study in seven European countries (the Europall project). Palliat Med 28(2):121–129. https://doi.org/10.1177/0269216313493952
Froggatt K, Preston N, Turner M, Kerr C (2015) Patient and public involvement in research and the Cancer Experiences Collaborative: benefits and challenges. BMJ Support Palliat Care 5(5):518–521. https://doi.org/10.1136/bmjspcare-2013-000548
Köpke S, Giordano A, Veronese S, Rahn AC, Kleiter I, Basedow-Rajwich B, Fornari A, Battaglia MA, Drulovic J, Kooij L, Koops J, Mens J, Meza Murillo ER, Milanov I, Milo R, Patti F, Pekmezovic T, Sastre-Garriga J, Vosburgh J, Voltz R, Bay J, Oliver DJ, Solari A (2019) Patient and caregiver involvement in the formulation of guideline questions: findings from the European Academy of Neurology guideline on palliative care of people with severe multiple sclerosis. Eur J Neurology 26(1):41–50. https://doi.org/10.1111/ene.13760
Tong E, Lo C, Moura S, Antes K, Buchanan S, Kamtapersaud V, Devins GM, Zimmermann C, Gallinger S, Rodin G (2019) Development of a psychoeducational intervention for people affected by pancreatic cancer. Pilot Feasibility Stud 5(1):80. https://doi.org/10.1186/s40814-019-0466-x
Herbst FA, Gawinski, Stiel S, Schneider N (2020) Zum Umgang mit Belastungen am Lebensende – Empfehlungen für psychosoziale Unterstützungsmaßnahmen für Eltern und erwachsene Kinder. https://www.dgpalliativmedizin.de/diverses/dgpveroeffentlichungen.html. Accessed 03 Feb 2021
Acknowledgements
The authors gratefully thank all experts and members of the multi-professional advisory board for their participation in the Delphi study. The authors also acknowledge Valerie Appleby for her copyediting of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The present Delphi survey represents one part of the study “Dy@EoL—interaction at the end of life in dyads of parents and adult children,” financed by the German Federal Ministry of Education and Research (BMBF) (grant nr 01GY1711). The funding body played no role in the study design; the collection, analysis, or interpretation of data; or the drafting of this article.
Author information
Authors and Affiliations
Contributions
F.A.H. (female), a medical anthropologist working as a senior researcher, led the study, collected and analyzed the data, and wrote the manuscript. L.G. (female), an anthropologist working as a junior researcher, collected and analyzed the data. F.A.H. and L.G. developed the hypotheses and recommendations. N.S. supervised the research process. S.S. (female), a psychologist working as a senior researcher, wrote the grant application, developed the Dy@EoL study design, and scrutinized the hypotheses, recommendations, and Delphi survey. All authors revised the manuscript critically and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval
The Dy@Eol study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Hannover Medical School: no. 7610, 04/10/2017.
Consent to participate and for publication
Individual written informed consent to participate and for the results of the study to be published was obtained from all patients and family caregivers who participated in the qualitative interviews. Prior to accessing the anonymous Delphi survey, experts were informed that the survey data would be treated anonymously and in accordance with data protection guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Herbst, F.A., Gawinski, L., Schneider, N. et al. Consensus-based recommendations for psychosocial support measures for parents and adult children at the end of life: results of a Delphi study in Germany. Support Care Cancer 30, 669–676 (2022). https://doi.org/10.1007/s00520-021-06452-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06452-x