Abstract
Purpose
The aim of this study is to establish the prevalence, associated factors, and clinical impact of delirium in newly referred palliative care patients and the percentage of delirium diagnoses missed by primary medical teams.
Methods
Newly referred palliative care patients were evaluated and were reviewed for possible associated factors of delirium. Univariable and multivariable analysis were used to identify associated factors. Median overall survival and survival curves were analyzed. The percentage of missed diagnosis in IPD patients was identified.
Results
We included 350 palliative care patients. Nearly all patients had cancer diagnosis (96.6%). The overall prevalence of delirium was 44.0%. The independent associated factors of delirium were age ≥ 63 years (adjusted odds ratio [aOR], 7.0; 95% CI, 2.2–22.9), palliative performance scale ≤ 20% (aOR, 54.5; 95% CI, 13.1–228.0), brain metastasis (aOR, 15.6; 95% CI, 3.7–66.7), urinary tract infection (aOR, 18.8; 95% CI, 4.7–75.5), sepsis (aOR, 59.0; 95% CI, 4.4–797.8), hyponatremia (aOR, 8.8; 95% CI, 2.6–29.8), and hypercalcemia (not applicable). Interestingly, opioids and benzodiazepines were not associated with delirium. Delirious patients had significantly shorter survival (median survival 11 days). Delirium diagnoses were missed for 76.1%.
Conclusion
Nearly half of the palliative care patients had delirium, which was associated with noticeably short survivals. We identified the independent factors associated with the delirium. Despite having a remarkably high prevalence rate and being a well-known poor prognostic factor, there was still a very high rate of missed delirium diagnoses. Effective, routine, delirium screening of palliative care patients needs to be emphasized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium is common in the palliative care population [1], with reported prevalences of 13–93% varying with multiple factors, such as comorbidities, study setting, and how far along patients are in their disease trajectories [2,3,4]. Delirium is characterized by acute disturbances to awareness, attention, and cognitive functions [5]. It is also associated with increased morbidity and mortality rates, higher symptom expression, prolonged hospitalization, negative financial consequences, and impediments to communication, all of which cause distress to patients and their families [6,7,8,9]. Unfortunately, delirium is frequently misdiagnosed for a range of reasons, including medical personnel’s lack of awareness and knowledge, the fluctuating nature of delirium symptoms and their resemblance to those of other psychiatric disorders, and inadequate regular screening for delirium [10,11,12,13].
As to a multifactorial model, delirium is the result of a combination of predisposing and precipitating factors [14]. However, the factors that are common to delirious palliative care patients have not been well characterized, with structured evidence of the predisposing and precipitating factors of delirium in palliative care patients being sparse [2, 4]. The most frequently occurring predisposing factors are older age, reduced performance status, and brain metastasis [3, 15,16,17], while the most prevalent precipitating factors are opioids, other psychoactive medications, electrolyte imbalance, and infections [18,19,20]. Comprehensive characterization of the causes of delirium could promote prompt investigations and appropriate interventions [21].
Our primary objectives were to identify the prevalence and associated factors of delirium among palliative care patients. The secondary objectives were to (1) examine the clinical impact of delirium on survival time and length of hospital stay and (2) determine the percentage of delirium diagnoses missed by the primary medical teams (PMTs) in a palliative care setting.
Materials and methods
Study population
The protocol was approved by the institution review board of the Faculty of Medicine Siriraj Hospital, Mahidol University; Reference number Si 421/2017. The participants were patients aged 18 years or older with advanced cancer or major organ failure who had been referred to the outpatient or inpatient department (OPD or IPD) of the palliative care center. However, due to ethical consideration, patients were excluded if the psychiatrist confirmed that they had a persistent symptom score of 7 or more in any item of the Edmonton Symptom Assessment System. Furthermore, patients diagnosed with dementia or mental retardation, had coma, or had a communication difficulty caused by an endotracheal intubation or a tracheostomy were excluded. Written informed consents were obtained from the patients or their proxies.
The participants were assessed by a psychiatrist using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria for delirium [22] via a semi-structured interview. If delirium was diagnosed, the subtype (hyperactive, hypoactive, and mixed) was identified according to the psychomotor activity exhibited by the patient. All patients were reviewed for potential factors associated with delirium by reviewing their history of illness, treatment-related factors, physical examination findings, and laboratory investigations. All of them were followed up until death and the prevalence rate of delirium in patients with survival time 31–60, 15–30, 4–14, and 1–3 days were calculated.
To facilitate the analysis of the diagnoses made by the PMTs, the patients in the IPD group were grouped into those who were (1) referred for other symptoms and were not found to have delirium (“no delirium”); (2) referred for other symptoms, but were found to have delirium (“missed diagnosis”); (3) correctly diagnosed with delirium by the PMTs (“correct diagnosis”); and (4) referred with suspected delirium, but were not found to have a diagnosis of delirium (“incorrect diagnosis”). We included only the IPD patients in this analysis because they were seen within 24 h of referral. In contrast, the OPD patients had a lag time between their referral and appointment dates; they could have developed delirium during this period, which would have affected the correctness of their diagnoses.
Statistical analysis
The main study objectives were to determine the prevalence and the associated factors of delirium in patients referred to the palliative care center. Surveillance data from the Siriraj Palliative Care Center in 2016 demonstrated a delirium prevalence of 35%; this figure was used to calculate the sample size of the present study. With an allowable error of 5% at a 95% confidence interval (CI), nQuery Advisor version 5.0 yielded an evaluable sample size of 350 patients.
A post hoc power analysis was conducted to verify the adequacy of the sample size for multiple logistic regression analysis using the program G*Power (version 3.1.9.2) [23]. We considered a model with a single predictor (age ≥ 63 years), which was binomially distributed and identified as the weakest independent factor associated with delirium by our multivariable analysis. Using that, with a base rate of age 63 ≥ years to be delirium of 0.53, a two-tailed z test, an event rate under H0 of π1 = 0.56, an adjusted odds ratio for the predictor (age ≥ 63 years) of 7.044, and a total sample size of 350, the proportion of variance of age ≥ 63 years was explained by 7 independent predictors of delirium in the model of 11%; we therefore needed an “R2 other X” of 0.11. When using the Demidenko method for sample size calculation for logistic regression [24] (with variance correction), the post hoc power analysis showed a power of 0.9999, which suggested the study had adequate power to detect an association between 8 independent predictors and delirium.
Data were prepared and analyzed using PASW Statistics for Windows (version 18.0; SPSS Inc., Chicago, Ill., USA). The quantitative data were expressed as means and standard deviations, or as medians and interquartile ranges, as appropriate, while the qualitative data were summarized with frequencies and percentages. Normality of data distribution was verified with the Shapiro–Wilk test. To compare the demographics, clinical characteristics (comorbidities, precipitating variables, and medications used), and clinical impacts of the delirium and non-delirium patients, an unpaired t-test or the Mann–Whitney U test was used for the quantitative data, whereas Pearson’s chi-squared test, Yates’ continuity correction, or Fisher’s exact test was used for the qualitative data, as appropriate. A receiver operating characteristic curve was used to determine the optimal cutoff value of age and palliative performance scale (PPS) for the prediction of delirium. A univariable analysis was performed to identify the factors associated with delirium; the variables with a P value of < 0.05 were subsequently included in a backward multiple logistic regression analysis to identify the independent predictors of delirium. Odds ratios (ORs) were used to evaluate the strength and direction of the association between the factors and delirium.
Median overall survival and overall survival curves were analyzed using the Kaplan–Meier method. The survival times were calculated from the date of consultation to the date of death, while the endpoint was the 1-year follow-up; the patients who were still alive at the end of the 1-year observation period were censored. A log-rank test was performed to compare the overall survival curves of the delirium and non-delirium groups. All tests of significance were two-tailed, and P < 0.05 was considered statistically significant.
Results
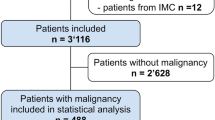
Between July 2017 and October 2018, 743 newly referred, palliative care patients were consecutively recruited. However, 393 of those were not enrolled. Sixty-three were excluded because they had a persistent symptom score of 7 or more in the Edmonton Symptom Assessment System (28 patients with pain, 25 with dyspnea, and 10 with depression). A further 43 patients were excluded due to having coma (28 patients), dementia (10), or communication difficulties resulting from endotracheal intubation or tracheostomy (5). Moreover, the consent of 33 patients to be involved in the research was not able to be obtained because of their altered state of consciousness and the absence of their proxies. The 254 remaining patients declined to participate in the study.
In all, 350 palliative care patients were enrolled. The prevalences of delirium in all 350 patients, the 140 OPD patients, and the 210 IPD patients were 44.0%, 26.4%, and 55.7%, respectively. The prevalences of delirium in patients with survival time 31–60, 15–30, 4–14, and 1–3 days were 32.7% (17/52), 44.6% (25/56), 72.4% (55/76), and 88.9% (32/36), respectively. In the delirium group, most patients had the mixed subtype (53.9%), followed by the hypoactive (38.3%) and hyperactive (7.8%) subtypes.
The results of the univariable analysis of the demographics, clinical characteristics, medication usage, and clinical impacts are detailed in Table 1. We found that age and the PPS values of the delirium and non-delirium groups had statistically significant differences both (P values were < 0.001). The optimal cut-off values of age and PPS for delirium were then calculated. The areas under receiver operating characteristic curves, sensitivities, specificities, and accuracies of age and PPS are presented in Fig. 1. The results of the subsequent multivariable analysis of the independent predictors of overall delirium are listed in Table 2. The unadjusted OR and adjusted OR of hypercalcemia and patients with no apparent precipitating cause were not applicable because there was no event in the non-delirium group for these factors.
The area under the receiver operating characteristic curve (AUC) of age and PPS for predicting delirium. The optimal cut-off value for age was ≥ 63 years, AUC = 0.633 (95% CI: 0.575–0.691) sensitivity = 67.5% (95% CI 59.8–74.4%), specificity = 53.1% (95% CI 46.1–59.9%), and accuracy = 59.4% (95% CI 54.2–64.4%). The optimal cut-off value for PPS was ≤ 20%, AUC = 0.862 (95% CI: 0.825–0.900), sensitivity = 59.1% (95% CI 51.2–66.5%), specificity = 96.4% (95% CI 92.8–98.3%), and accuracy = 80.0% (95% CI 75.5–83.9%). Abbreviation: CI confidence interval
The median overall survival time was 34 days (95% CI, 25.7–42.2 days), while the overall survival rate was 8.6%. The median overall survival time and overall survival rate of the delirium group was 11 days (95% CI, 7.2–14.8 days) and 1.3%, respectively, compared with 62 days (95% CI, 5.3–72.4 days) and 14.3% for the non-delirium group. The survival data of the delirium and non-delirium groups were compared using a log-rank test, which revealed a significantly higher survival time for the non-delirium group (P < 0.001; Fig. 2).
For 210 patients in the IPD group, 93 (44.3%) patients had no delirium, 28 (13.3%) had a correct diagnosis of delirium, 89 (42.4%) had a missed delirium diagnosis, and no patient had an incorrect diagnosis. In other words, of the total of 117 delirious IPD patients, the PMTs had missed the delirium diagnosis in 76.1% (89/117) and made a correct diagnosis for 23.9% (28/117).
Discussion
To our knowledge, this is the first study to examine the overall prevalence of delirium in newly referred palliative care patients in both OPD and IPD settings simultaneously [4, 25]. We found the overall prevalence was as high as 44%, with the IPD patients having a higher rate than the OPD patients. It is known that IPD patients tend to be in the later stages of disease and have more severe medical conditions, resulting in a higher prevalence of delirium. Our research also found that the prevalence of delirium increased as death approached, with 88.9% of patients being delirious on their last few days of life. Other studies have similarly reported that terminal delirium occurred in 88–93% of patients [2, 18, 26]. This remarkably high prevalence rate underscores the need for discussions to be conducted as early as possible about the goals of care, advance care planning, and the need to take care of unfinished business. Mixed delirium was the most prevalent subtype in our population, followed by hypoactive and hyperactive delirium; this concurs with most of the previous studies [6, 27,28,29].
While the univariable analysis identified 18 factors associated with delirium, the final model only utilized 8 variables. We confirmed that older age, a lower performance status, and brain metastasis were independent predisposing factors associated with delirium, which is consistent with the findings of earlier work [15,16,17, 30, 31]. Urinary tract infection, sepsis, and hyponatremia were independently associated precipitating factors of delirium [30, 32,33,34]. While hypercalcemia was also an independent associated factor, its OR was not able to be calculated because there was no event in the non-delirium group. We found that nearly one-fifth of the delirious patients had hypercalcemia; on the other hand, there were no hypercalcemic patients without delirium. As hypercalcemia is a correctable precipitating cause of delirium [31], we suggest that serum calcium should be checked in delirious patients. In addition, a considerable number of patients did not have any apparent precipitating cause. Such patients should still be promptly treated for their delirium symptoms, and they might need palliative sedation in cases of refractory agitated delirium [35, 36].
Interestingly, in contrast to most of the previous studies [18, 19, 26, 30], we found that psychoactive medications were not associated with delirium. This may be because our study recruited only newly referred palliative care patients, for whom the median morphine equivalent daily dose was only 11.25 mg. There has been reported to be a decreasing trend in the dosage of opioids prescribed for referred palliative care patients [37, 38]. One study reported that cognitive dysfunction was associated with opioid doses exceeding a 400 mg morphine equivalent daily dose, which is far greater than the amount used for our population [39]. Benzodiazepines were also not associated with delirium for the same reason.
As with previous studies [18, 40], our results showed that patients in the delirium group had a shorter survival time (median: 11 days) than those in the non-delirium group. This highlights that delirium is a very poor prognostic factor. However, in contrast with previous studies, the patients in the delirium group had a shorter length of stay than those in the non-delirium group [8, 41]. This may be because the delirium patients in our study had a shorter survival time and, thus, a shorter length of stay, than the non-delirium patients.
We found that the PMTs missed delirium diagnoses in most of the cases (76.1%). This level is similar to the findings of previous studies that investigated the degree to which delirium diagnoses were missed [10, 42]. The data confirms that delirium assessments are still underperformed and that measures to raise awareness of this condition are needed.
Clinical implications
Delirium is highly prevalent in newly referred palliative care population, causes substantial distress to patients and their families, and significantly associated with shorter survival. Therefore, delirium screening in this population needs to be emphasized. Multiple predisposing and precipitating factors of delirium in this population were identified. This could facilitate in proper investigations and timely interventions.
Study limitations
There are some limitations to our study. For one thing, we excluded patients with persistent symptoms such as pain, dyspnea, and depression. As it is possible that those patients might have had high symptom expression due to delirium, excluding them may have resulted in a lower prevalence rate than otherwise. However, in our usual clinical assessments of patients with a high physical symptom score, we routinely give an instant treatment such as an oxygen supplement or immediate — release opioids. This routine procedure resulted in only 63 patients out of 743 (8.48%) being excluded, which we believe would not lead to a significant selection bias. Another concern is that we excluded 10 patients with dementia, due to the complexity on the diagnosis of delirium on top of dementia. Nevertheless, this small number should neither affect the overall prevalence rate nor association with other factors. The results of this research might therefore not be applicable to dementia patients. Lastly, the refusal rate of participation in this study was quite high (254/743, 34.19%). However, in the recruitment process, ineligible patients were all excluded before invitation so this also would not lead to a significant selection bias. Most of them just refused because of time constraints.
Conclusions
The overall prevalence of delirium among the referred palliative care patients was as high as 44%, and the rate rose as death drew nearer. Older age, a lower PPS, brain metastasis, urinary tract infection, sepsis, hyponatremia, and hypercalcemia were independent factors associated with delirium. Delirium was significantly associated with a shorter survival, with a median survival time of only 11 days. Despite the high delirium prevalence rate and the condition being a very poor prognostic factor, there was still a markedly high rate of missed diagnoses of delirium. Effective, routine, delirium screening of palliative care patients needs to be given much greater emphasis.
Data availability
The data that support the findings of this study are available on request from the corresponding author, ST. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Code availability
Not applicable
References
Grassi L, Caraceni A, Mitchell AJ, Nanni MG, Berardi MA, Caruso R, Riba M (2015) Management of delirium in palliative care: a review. Curr Psychiatry Rep 17(3):550. https://doi.org/10.1007/s11920-015-0550-8
Seiler A, Schubert M, Hertler C, Schettle M, Blum D, Guckenberger M, Weller M, Ernst J, von Kanel R, Boettger S (2019) Predisposing and precipitating risk factors for delirium in palliative care patients. Palliat Support Care:1–10. https://doi.org/10.1017/s1478951519000919
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383(9920):911–922. https://doi.org/10.1016/s0140-6736(13)60688-1
Hosie A, Davidson PM, Agar M, Sanderson CR, Phillips J (2013) Delirium prevalence, incidence, and implications for screening in specialist palliative care inpatient settings: a systematic review. Palliat Med 27(6):486–498. https://doi.org/10.1177/0269216312457214
Blazer DG, van Nieuwenhuizen AO (2012) Evidence for the diagnostic criteria of delirium: an update. Curr Opin Psychiatry 25(3):239–243. https://doi.org/10.1097/YCO.0b013e3283523ce8
Bruera E, Bush SH, Willey J, Paraskevopoulos T, Li Z, Palmer JL, Cohen MZ, Sivesind D, Elsayem A (2009) Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer 115(9):2004–2012. https://doi.org/10.1002/cncr.24215
DeCrane SK, Culp KR, Wakefield B (2012) Twelve-month fall outcomes among delirium subtypes. J Healthc Qual 34(6):13–20. https://doi.org/10.1111/j.1945-1474.2011.00162.x
O’Keeffe S, Lavan J (1997) The prognostic significance of delirium in older hospital patients. J Am Geriatr Soc 45(2):174–178. https://doi.org/10.1111/j.1532-5415.1997.tb04503.x
Bush SH, Tierney S, Lawlor PG (2017) Clinical assessment and management of delirium in the palliative care setting. Drugs 77(15):1623–1643. https://doi.org/10.1007/s40265-017-0804-3
de la Cruz M, Fan J, Yennu S, Tanco K, Shin S, Wu J, Liu D, Bruera E (2015) The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support Care Cancer 23(8):2427–2433. https://doi.org/10.1007/s00520-015-2610-3
Kennelly SP, Morley D, Coughlan T, Collins R, Rochford M, O’Neill D (2013) Knowledge, skills and attitudes of doctors towards assessing cognition in older patients in the emergency department. Postgrad Med J 89(1049):137–141. https://doi.org/10.1136/postgradmedj-2012-131226
Marchington KL, Carrier L, Lawlor PG (2012) Delirium masquerading as depression. Palliat Support Care 10(1):59–62. https://doi.org/10.1017/s1478951511000599
Braiteh F, El Osta B, Palmer JL, Reddy SK, Bruera E (2007) Characteristics, findings, and outcomes of palliative care inpatient consultations at a comprehensive cancer center. J Palliat Med 10(4):948–955. https://doi.org/10.1089/jpm.2006.0257
Inouye SK (2000) Prevention of delirium in hospitalized older patients: risk factors and targeted intervention strategies. Ann Med 32(4):257–263. https://doi.org/10.3109/07853890009011770
Ljubisavljevic V, Kelly B (2003) Risk factors for development of delirium among oncology patients. Gen Hosp Psychiatry 25(5):345–352. https://doi.org/10.1016/s0163-8343(03)00070-7
Martinez JA, Belastegui A, Basabe I, Goicoechea X, Aguirre C, Lizeaga N, Urreta I, Emparanza JI (2012) Derivation and validation of a clinical prediction rule for delirium in patients admitted to a medical ward: an observational study. BMJ Open 2(5). https://doi.org/10.1136/bmjopen-2012-001599
Gofton TE, Graber J, Carver A (2012) Identifying the palliative care needs of patients living with cerebral tumors and metastases: a retrospective analysis. J Neurooncol 108(3):527–534. https://doi.org/10.1007/s11060-012-0855-y
Lawlor PG, Gagnon B, Mancini IL, Pereira JL, Hanson J, Suarez-Almazor ME, Bruera ED (2000) Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med 160(6):786–794
Gaudreau JD, Gagnon P, Harel F, Roy MA, Tremblay A (2005) Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 23(27):6712–6718. https://doi.org/10.1200/jco.2005.05.140
Lin RY, Heacock LC, Fogel JF (2010) Drug-induced, dementia-associated and non-dementia, non-drug delirium hospitalizations in the United States, 1998–2005: an analysis of the national inpatient sample. Drugs Aging 27(1):51–61. https://doi.org/10.2165/11531060-000000000-00000
Lawlor PG, Bush SH (2015) Delirium in patients with cancer: assessment, impact, mechanisms and management. Nat Rev Clin Oncol 12(2):77–92. https://doi.org/10.1038/nrclinonc.2014.147
Association AP (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160. https://doi.org/10.3758/brm.41.4.1149
Demidenko E (2007) Sample size determination for logistic regression revisited. Stat Med 26(18):3385–3397. https://doi.org/10.1002/sim.2771
Watt CL, Momoli F, Ansari MT, Sikora L, Bush SH, Hosie A, Kabir M, Rosenberg E, Kanji S, Lawlor PG (2019) The incidence and prevalence of delirium across palliative care settings: a systematic review. Palliat Med 33(8):865–877. https://doi.org/10.1177/0269216319854944
Webber C, Watt CL, Bush SH, Lawlor PG, Talarico R, Tanuseputro P (2020) The occurrence and timing of delirium in acute care hospitalizations in the last year of life: a population-based retrospective cohort study. Palliat Med 34(8):1067–1077. https://doi.org/10.1177/0269216320929545
Klankluang W, Pukrittayakamee P, Atsariyasing W, Siriussawakul A, Chanthong P, Tongsai S, Tayjasanant S (2019) Validity and reliability of the memorial delirium assessment scale-Thai version (MDAS-T) for assessment of delirium in palliative care patients. Oncologist. https://doi.org/10.1634/theoncologist.2019-0399
Meagher D (2009) Motor subtypes of delirium: past, present and future. Int Rev Psychiatry 21(1):59–73. https://doi.org/10.1080/09540260802675460
Stagno D, Gibson C, Breitbart W (2004) The delirium subtypes: a review of prevalence, phenomenology, pathophysiology, and treatment response. Palliat Support Care 2(2):171–179
Bush SH, Bruera E (2009) The assessment and management of delirium in cancer patients. Oncologist 14(10):1039–1049. https://doi.org/10.1634/theoncologist.2009-0122
Delgado-Guay MO, Yennurajalingam S, Bruera E (2008) Delirium with severe symptom expression related to hypercalcemia in a patient with advanced cancer: an interdisciplinary approach to treatment. J Pain Symptom Manage 36(4):442–449. https://doi.org/10.1016/j.jpainsymman.2007.11.004
Tsuruta R, Oda Y (2016) A clinical perspective of sepsis-associated delirium. J Intensive Care 4:18. https://doi.org/10.1186/s40560-016-0145-4
Sagawa R, Akechi T, Okuyama T, Uchida M, Furukawa TA (2009) Etiologies of delirium and their relationship to reversibility and motor subtype in cancer patients. Jpn J Clin Oncol 39(3):175–182. https://doi.org/10.1093/jjco/hyn157
Castillo JJ, Vincent M, Justice E (2012) Diagnosis and management of hyponatremia in cancer patients. Oncologist 17(6):756–765. https://doi.org/10.1634/theoncologist.2011-0400
de Graeff A, Dean M (2007) Palliative sedation therapy in the last weeks of life: a literature review and recommendations for standards. J Palliat Med 10(1):67–85. https://doi.org/10.1089/jpm.2006.0139
Maltoni M, Scarpi E, Rosati M, Derni S, Fabbri L, Martini F, Amadori D, Nanni O (2012) Palliative sedation in end-of-life care and survival: a systematic review. J Clin Oncol 30(12):1378–1383. https://doi.org/10.1200/jco.2011.37.3795
Haider A, Zhukovsky DS, Meng YC, Baidoo J, Tanco KC, Stewart HA, Edwards T, Joy MP, Kuriakose L, Lu Z, Williams JL, Liu DD, Bruera E (2017) Opioid prescription trends among patients with cancer referred to outpatient palliative care over a 6-year period. J Oncol Pract 13(12):e972–e981. https://doi.org/10.1200/jop.2017.024901
Yennurajalingam S, Lu Z, Reddy SK, Rodriguez EC, Nguyen K, Waletich-Flemming MJ, Lim K-H, Memon A, Nguyen N-N, Rofheart KW, Wang G, Barla SR, Wu J, Williams JL, Bruera E (2019) Patterns of opioid prescription, use, and costs among patients with advanced cancer and inpatient palliative care between 2008 and 2014. J oncol pract 15(1):e74–e83. https://doi.org/10.1200/JOP.18.00205
Kurita GP, Sjøgren P, Ekholm O, Kaasa S, Loge JH, Poviloniene I, Klepstad P (2011) Prevalence and predictors of cognitive dysfunction in opioid-treated patients with cancer: a multinational study. J Clin Oncol 29(10):1297–1303. https://doi.org/10.1200/jco.2010.32.6884
Scarpi E, Maltoni M, Miceli R, Mariani L, Caraceni A, Amadori D, Nanni O (2011) Survival prediction for terminally ill cancer patients: revision of the palliative prognostic score with incorporation of delirium. Oncologist 16(12):1793–1799. https://doi.org/10.1634/theoncologist.2011-0130
Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK (2001) The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med 27(12):1892–1900. https://doi.org/10.1007/s00134-001-1132-2
Kishi Y, Kato M, Okuyama T, Hosaka T, Mikami K, Meller W, Thurber S, Kathol R (2007) Delirium: patient characteristics that predict a missed diagnosis at psychiatric consultation. Gen Hosp Psychiatry 29(5):442–445. https://doi.org/10.1016/j.genhosppsych.2007.05.006
Acknowledgements
The authors gratefully acknowledge the help provided by Panate Pukrittayakamee, Wanlop Atsariyasing, Tashita Pinsanthia, and Rachaneekorn Ramlee with documentation and collaboration.
Funding
This study was facilitated by the Integrated Perioperative Geriatric Excellent Research Center, and it was supported by a grant from the Routine to Research Unit, Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand (grant number [IO] R016035032).
Author information
Authors and Affiliations
Contributions
Conception/design: Watanachai Klankluang, Supakarn Tayjasanant, Arunotai Siriussawakul
Collection and/or assembly of data: Watanachai Klankluang, Chairat Sriphirom, Pratamaporn Chanthong
Data analysis and interpretation: Sasima Tongsai, Watanachai Klankluang, Supakarn Tayjasanant
Manuscript writing: Watanachai Klankluang, Supakarn Tayjasanant, Sasima Tongsai
Final approval of manuscript: Watanachai Klankluang, Supakarn Tayjasanant, Sasima Tongsai, Chairat Sriphirom, Arunotai Siriussawakul, Pratamaporn Chanthong
Corresponding author
Ethics declarations
Ethics approval
The protocol was approved by the institution review board of the Faculty of Medicine Siriraj Hospital, Mahidol University; Reference number Si 421/2017.
Consent to participate
Written informed consents were obtained from the patients or their proxies.
Consent for publication
Written informed consents were obtained from the patients or their proxies.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klankluang, W., Tongsai, S., Sriphirom, C. et al. The prevalence, associated factors, clinical impact, and state of diagnosis of delirium in palliative care patients. Support Care Cancer 29, 7949–7956 (2021). https://doi.org/10.1007/s00520-021-06367-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06367-7