Abstract
Purpose
It is unclear how NCCN guidelines recommend “supportive care” and “best supportive care” in oncology practice. We examined the usage of “supportive care” and “best supportive care” in NCCN guidelines and compared between solid tumor and hematologic malignancy guidelines.
Methods
We reviewed all updated NCCN Guidelines for Treatment of Cancer in October 2019. We documented the frequency of occurrence, definition, and timing of introduction of each term. We compared between solid tumor and hematologic malignancy guidelines.
Results
We identified a total of 37 solid tumor and 16 hematologic guidelines. Thirty-seven (70%) guidelines mentioned “supportive care” and 36 (68%) mentioned “best supportive care.” Hematologic guidelines were significantly more likely than solid tumor guidelines to use the term “supportive care” (median occurrence 19 vs. 2; P = 0.001) and to describe “supportive care” as management of cancer-related complications (N = 11/15, 73% vs. N = 2/22, 9%; P < 0.001). Domains of specialist palliative care were infrequently mentioned (N = 10/37, 27%). In contrast, solid tumor guidelines were significantly more likely than hematologic guidelines to mention “best supportive care” (median occurrence 6 vs. 0; P = 0.016). This term was rarely defined and mostly used in the advanced disease setting.
Conclusion
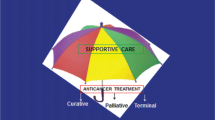
“Supportive care” and “best supportive care” were frequently used in NCCN guidelines, with significant variations in usage between solid tumor and hematologic oncologists. “Supportive care” was mostly limited to management of cancer-related complications and treatment adverse effects in NCCN guidelines, highlighting the need to go beyond the traditional biomedical model to more a patient-centered care model with greater integration of palliative care.
Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Torre LA, Siegel RL, Ward EM, Jemal A (2016) Global cancer incidence and mortality rates and trends–an update. Cancer Epidemiol Biomarkers Prev 25:16–27
Shah-Manek B, Wong W, Ravelo A, DiBonaventura M (2018) Oncologists’ perceptions of drug affordability using NCCN evidence blocks: results from a national survey. J Manag Care Spec Pharm 24:565–571
Ernecoff NC, Check D, Bannon M et al (2020) Comparing specialty and primary palliative care interventions: analysis of a systematic review. J Palliat Med 23:389–396
World Health Organization (2018) Latest global cancer data: cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018. https://www.who.int/cancer/PRGlobocanFinal.pdf. Accessed 25 November 2019
Hui D, De La Cruz M, Mori M et al (2013) Concepts and definitions for “supportive care”, “best supportive care”, “palliative care”, and “hospice care” in the published literature, dictionaries, and textbooks. Support Care Cancer 21:659–685
Lee RT, Ramchandran K, Sanft T, Von Roenn J (2015) Implementation of supportive care and best supportive care interventions in clinical trials enrolling patients with cancerdagger. Ann Oncol 26:1838–1845
Hui D (2014) Definition of supportive care: does the semantic matter? Curr Opin Oncol 26:372–379
Cellerino R, Tummarello D, Guidi F, Isidori P, Raspugli M, Biscottini B, Fatati G (1991) A randomized trial of alternating chemotherapy versus best supportive care in advanced non-small-cell lung cancer. J Clin Oncol 9:1453–1461
Jack B, Boland A, Dickson R, Stevenson J, McLeod C (2010) Best supportive care in lung cancer trials is inadequately described: a systematic review. Eur J Cancer Care (Engl) 19:293–301
Cherny N (2011) Best supportive care: a euphemism for no care or a standard of good care? Semin Oncol 38:351–357
Sanz Rubiales A, Sanchez-Gutierrez ME, Flores Perez LA, Del Valle Rivero ML (2020) How is best supportive care provided in clinical trials for patients with advanced cancer? A review of registered protocols of clinical trials. Curr Oncol 27:e100–e105
Paz-Ares L, de Marinis F, Dediu M et al (2012) Maintenance therapy with pemetrexed plus best supportive care versus placebo plus best supportive care after induction therapy with pemetrexed plus cisplatin for advanced non-squamous non-small-cell lung cancer (PARAMOUNT): a double-blind, phase 3, randomised controlled trial. Lancet Oncol 13:247–255
Kang JH, Lee SI, Lim DH et al (2012) Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone. J Clin Oncol 30:1513–1518
Mo L, Urbauer DL, Bruera E, Hui D (2021) Recommendations for palliative and hospice care in NCCN guidelines for treatment of cancer. Oncologist 26:77–83
Hui D, Hannon BL, Zimmermann C, Bruera E (2018) Improving patient and caregiver outcomes in oncology: team-based, timely, and targeted palliative care. CA Cancer J Clin 68:356–376
Brudno JN, Kochenderfer JN (2019) Recent advances in CAR T-cell toxicity: mechanisms, manifestations and management. Blood Rev 34:45–55
Fu JB, Tennison JM, Rutzen-Lopez IM, Silver JK, Morishita S, Dibaj SS, Bruera E (2018) Bleeding frequency and characteristics among hematologic malignancy inpatient rehabilitation patients with severe thrombocytopenia. Support Care Cancer 26:3135–3141
Fontana L, Strasfeld L (2019) Respiratory virus infections of the stem cell transplant recipient and the hematologic malignancy patient. Infect Dis Clin North Am 33:523–544
Ludwig H (2002) Anemia of hematologic malignancies: what are the treatment options? Semin Oncol 29:45–54
Yilmaz M, Atilla FD, Sahin F, Saydam G (2020) The effect of malnutrition on mortality in hospitalized patients with hematologic malignancy. Support Care Cancer 28:1441–1448
Koizumi K, Tayama J, Ishioka T, Nakamura-Thomas H, Suzuki M, Hara M, Makita S, Hamaguchi T (2018) Anxiety, fatigue, and attentional bias toward threat in patients with hematopoietic tumors. PLoS One 13:e0192056
Jordan K, Aapro M, Kaasa S et al (2018) European Society for Medical Oncology (ESMO) position paper on supportive and palliative care. Ann Oncol 29:36–43
El-Jawahri A, LeBlanc T, VanDusen H et al (2016) Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: a randomized clinical trial. JAMA 316:2094–2103
Porta-Sales J, Guerrero-Torrelles M, Moreno-Alonso D, Sarra-Escarre J, Clapes-Puig V, Trelis-Navarro J, Sureda-Balari A, Fernandez De Sevilla-Ribosa A (2017) Is early palliative care feasible in patients with multiple myeloma? J Pain Symptom Manage 54:692–700
Epstein AS, Goldberg GR, Meier DE (2012) Palliative care and hematologic oncology: the promise of collaboration. Blood Rev 26:233–239
Smith TJ, Temin S, Alesi ER et al (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30:880–887
El-Jawahri AR, Abel GA, Steensma DP et al (2015) Health care utilization and end-of-life care for older patients with acute myeloid leukemia. Cancer 121:2840–2848
Temel JS, Greer JA, El-Jawahri A et al (2017) Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol 35:834–841
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733–742
Hui D, Didwaniya N, Vidal M, Shin SH, Chisholm G, Roquemore J, Bruera E (2014) Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer 120:1572–1578
Hui D, Park M, Liu D, Reddy A, Dalal S, Bruera E (2015) Attitudes and beliefs toward supportive and palliative care referral among hematologic and solid tumor oncology specialists. Oncologist 20:1326–1332
Hui D, Cerana MA, Park M, Hess K, Bruera E (2016) Impact of oncologists’ attitudes toward end-of-life care on patients’ access to palliative care. Oncologist 21:1149–1155
Ruiz M, Reynolds P, Marranzini R, Khan A, Ketterer J, Brahim A (2018) Role of early palliative care interventions in hematological malignancies and bone marrow transplant patients: barriers and potential solutions. Am J Hosp Palliat Care 35:1456–1460
LeBlanc TW, O’Donnell JD, Crowley-Matoka M, Currow DC, Abernethy AP (2015) Perceptions of palliative care among hematologic malignancy specialists: a mixed-methods study. J Oncol Pract 11:e230–e238
Barni S, Maltoni M, Tuveri G et al (2011) Attitude of Italian medical oncologists toward palliative care for patients with advanced cancer: results of the SIO project. Support Care Cancer 19:381–389
Cherny RI, Catane R, European Society of Medical Oncology Taskforce on Palliative and Supportive Care (2003) Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survery by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer 98:2502–2510
Lesnock JL, Arnold RM, Meyn LA, Buss MK, Quimper M, Krivak TC, Edwards RP, Chang JC (2013) Palliative care education in gynecologic oncology: a survey of the fellows. Gynecol Oncol 130:431–435
Buss MK, Lessen DS, Sullivan AM, Von Roenn J, Arnold RM, Block SD (2011) Hematology/oncology fellows’ training in palliative care: results of a national survey. Cancer 117:4304–4311
Feld E, Singhi EK, Phillips S, Huang LC, Shyr Y, Horn L (2019) Palliative care referrals for advanced non-small-cell lung cancer (NSCLC): patient and provider attitudes and practices. Clin Lung Cancer 20:e291–e298
Hui D, De La Rosa A, Chen J, Dibaj S, Delgado Guay M, Heung Y, Liu D, Bruera E (2020) State of palliative care services at US cancer centers: an updated national survey. Cancer 126:2013–2023
Zafar SY, Currow DC, Cherny N, Strasser F, Fowler R, Abernethy AP (2012) Consensus-based standards for best supportive care in clinical trials in advanced cancer. Lancet Oncol 13:e77–e82
Funding
This work was supported in part by National Institutes of Health (NIH) / National Cancer Institute grants (R01CA214960‐01A1; R01CA225701‐01A1; R01CA231471-01A1 to D.H.) and a National Institute of Nursing Research grant (1R21NR016736‐01 to D.H.). This work was also supported in part by a National Institutes of Health Cancer Center Support grant (P30CA016672 to D.U.).
Author information
Authors and Affiliations
Contributions
Study concept and design: David Hui and Li Mo. Data acquisition/analysis and interpretation: all authors. Manuscript preparation/critical revision for important intellectual content: David Hui and Li Mo. Final approval: all authors.
Corresponding author
Ethics declarations
Ethics approval
The Institutional Review Board at MD Anderson Cancer Center reviewed the protocol and provided approval to proceed without the need for full committee review.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mo, L., Urbauer, D.L., Bruera, E. et al. Recommendations for supportive care and best supportive care in NCCN clinical practice guidelines for treatment of cancer: Differences between solid tumor and hematologic malignancy guidelines. Support Care Cancer 29, 7385–7392 (2021). https://doi.org/10.1007/s00520-021-06245-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06245-2