Abstract
Purpose
The aim of the study was to determine the diagnostic accuracy of patient-reported dry mouth using an oral moisture-checking device in terminally ill cancer patients.
Methods
The study was conducted following the STARD guidelines, and the participants were recruited prospectively from the Palliative Care Unit, Kyoto Medical Center, Japan, between 1 January 2017 and 30 November 2018. Patients reporting dry mouth were asked to rate oral dryness on a 5-point rating scale. The outcome was oral dryness at the lingual mucosa, measured using an oral moisture-checking device. Receiver operating characteristic (ROC) curves were plotted, and the sensitivity, specificity, positive and negative predictive values (PPV and NPV), positive and negative likelihood ratios (LR), and overall diagnostic accuracy were calculated.
Results
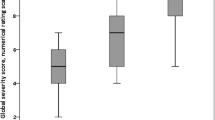
Of 103 participants, the prevalence of oral dryness was 65.0%. ROC analysis indicated that patient-reported dry mouth was a poor predictor of oral dryness, with an area under the curve of 0.616 (95% confidence interval: 0.508–0.723), a sensitivity of 46.3%, a specificity of 75.8%, a PPV of 55.9%, an NPV of 68.1, a positive LR of 1.9, a negative LR of 0.7, and an overall diagnostic accuracy of 64.1%, with a cut-off value of 3 points.
Conclusion
In conclusion, patient-reported dry mouth is not a useful parameter for the assessment of oral dryness in terminally ill cancer patients.

Similar content being viewed by others
References
Davies AN (2015) Oxford text palliative care 5th. Oral care. Oxford University Press, London, pp 448–456
Matsuo K, Watanabe R, Kanamori D, Nakagawa K, Fujii W, Urasaki Y, Murai M, Mori N, Higashiguchi T (2016) Associations between oral complications and days to death in palliative care patients. Support Care Cancer 24:157–161. https://doi.org/10.1007/s00520-015-2759-9
Nakajima N (2017) Characteristics of oral problems and effects of oral care in terminally ill patients with cancer. Am J Hosp Palliat Care 34:430–434. https://doi.org/10.1177/1049909116633063
Ohno T, Morita T, Tamura F, Hirano H, Watanabe Y, Kikutani T (2016) The need and availability of dental services for terminally ill cancer patients: a nationwide survey in Japan. Support Care Cancer 24:19–22. https://doi.org/10.1007/s00520-015-2734-5
Sweeney MP, Bagg J, Baxter WP, Aitchison TC (1998) Oral disease in terminally ill cancer patients with xerostomia. Oral Oncol 34:123–126. https://doi.org/10.1016/s1368-8375(97)00076-6
Davies A (1997) The management of xerostomia: a review. Eur J Cancer Care 6:209–214. https://doi.org/10.1046/j.1365-2354.1997.00036.x
Mercadante S, Aielli F, Adile C, Ferrera P, Valle A, Fusco F, Caruselli A, Cartoni C, Massimo P, Masedu F, Valenti M, Porzio G (2015) Prevalence of oral mucositis, dry mouth, and dysphagia in advanced cancer patients. Support Care Cancer 23:3249–3255. https://doi.org/10.1007/s00520-015-2720-y
Wilberg P, Hjermstad MJ, Ottesen S, Herlofson BB (2012) Oral health is an important issue in end-of-life cancer care. Support Care Cancer 20:3115–3122. https://doi.org/10.1007/s00520-012-1441-8
Davies AN, Broadley K, Beighton D (2001) Xerostomia in patients with advanced cancer. J Pain Symptom Manag 22:820–825. https://doi.org/10.1016/s0885-3924(01)00318-9
Fischer DJ, Epstein JB, Yao Y, Wilkie DJ (2014) Oral health conditions affect functional and social activities of terminally ill cancer patients. Support Care Cancer 22:803–810. https://doi.org/10.1007/s00520-013-2037-7
Guggenheimer J, Moore PA (2003) Xerostomia: etiology, recognition and treatment. J Am Dent Assoc 134:61–69; quiz 118–119. https://doi.org/10.14219/jada.archive.2003.0018
Davies A, Mundin G, Vriens J, Webber K, Buchanan A, Waghorn M (2015) The influence of low salivary flow rates on the absorption of a sublingual fentanyl citrate formulation for breakthrough cancer pain. J Pain Symptom Manag. https://doi.org/10.1016/j.jpainsymman.2015.11.018
Fleming M, Craigs CL, Bennett MI (2020) Palliative care assessment of dry mouth: what matters most to patients with advanced disease? Support Care Cancer 28:1121–1129. https://doi.org/10.1007/s00520-019-04908-9
Kvalheim SF, Marthinussen MC, Haugen DF, Berg E, Strand GV, Lie SA (2019) Randomized controlled trial of the effectiveness of three different oral moisturizers in palliative care patients. Eur J Oral Sci 127:523–530. https://doi.org/10.1111/eos.12655
Magnani C, Mastroianni C, Giannarelli D, Stefanelli MC, Di Cienzo V, Valerioti T et al (2019) Oral hygiene care in patients with advanced disease: an essential measure to improve oral cavity conditions and symptom management. Am J Hosp Palliat Med 36:815–819. https://doi.org/10.1177/1049909119829411
Nikles J, Mitchell GK, Hardy J, Agar M, Senior H, Carmont S-A, Schluter PJ, Good P, Vora R, Currow D (2013) Do pilocarpine drops help dry mouth in palliative care patients: a protocol for an aggregated series of n-of-1 trials. BMC Palliative Care 12:39. https://doi.org/10.1186/1472-684x-12-39
Oechsle K, Wais MC, Vehling S, Bokemeyer C, Mehnert A (2014) Relationship between symptom burden, distress, and sense of dignity in terminally ill cancer patients. J Pain Symptom Manag 48:313–321. https://doi.org/10.1016/j.jpainsymman.2013.10.022
Okuyama T, Wang XS, Akechi T, Mendoza TR, Hosaka T, Cleeland CS, Uchitomi Y (2003) Japanese version of the M.D. Anderson Symptom Inventory: a validation study. J Pain Symptom Manag 26:1093–1104. https://doi.org/10.1016/j.jpainsymman.2003.05.003
Cheng Y-M, Lan S-H, Hsieh Y-P, Lan S-J, Hsu S-W (2019) Evaluate five different diagnostic tests for dry mouth assessment in geriatric residents in long-term institutions in Taiwan. BMC Oral Health 19. https://doi.org/10.1186/s12903-019-0797-2
Fujimaki Y, Tsunoda K, Ishimoto S-I, Okada K, Kinoshita M, Igaki H, Terahara A, Asakage T, Yamasoba T (2014) Non-invasive objective evaluation of radiotherapy-induced dry mouth. J Oral Pathol Med 43:97–102. https://doi.org/10.1111/jop.12099
Fukushima Y, Yoda T, Kokabu S, Araki R, Murata T, Kitagawa Y, Omura K, Toya S, Ito K, Funayama S, Iwabuchi H, Asano K, Imai Y, Negishi A, Yokoo S, Matsumoto G, Kubota E, Watanabe H, Kusama M, Onizawa K, Goto T, Nakamura S, Nakazawa R, Harada K, Fujibayashi T (2013) Evaluation of an oral moisture-checking device for screening dry mouth. Open J Stomatol 03:440–446. https://doi.org/10.4236/ojst.2013.38073
Kim H-J, Lee J-Y, Lee E-S, Jung H-J, Ahn H-J, Kim B-I (2019) Improvements in oral functions of elderly after simple oral exercise. Clin Interv Aging 14:915–924. https://doi.org/10.2147/cia.s205236
Takahashi F, Koji T, Morita O (2006) Oral dryness examinations: use of an oral moisture checking device and a modified cotton method. Prosthodont Res Pract 5:26–30. https://doi.org/10.2186/prp.5.26
Sakurai H, Miyashita M, Imai K, Miyamoto S, Otani H, Oishi A, Kizawa Y, Matsushima E (2019) Validation of the Integrated Palliative care Outcome Scale (IPOS)—Japanese version. Jpn J Clin Oncol 49:257–262. https://doi.org/10.1093/jjco/hyy203
Metz CE (1978) Basic principles of ROC analysis. Semin Nucl Med 8:283–298. https://doi.org/10.1016/s0001-2998(78)80014-2
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47:458–472. https://doi.org/10.1002/bimj.200410135
Fitzsimons JT (1972) Thirst. Physiol Rev 52:468–561
Hatano Y, Matsuoka H, Lam L, Currow DC (2018) Side effects of corticosteroids in patients with advanced cancer: a systematic review. Support Care Cancer 26:3979–3983. https://doi.org/10.1007/s00520-018-4339-2
Thunhorst RL, Beltz TG, Johnson AK (2007) Glucocorticoids increase salt appetite by promoting water and sodium excretion. Am J Phys Regul Integr Comp Phys 293:R1444–R1451. https://doi.org/10.1152/ajpregu.00294.2007
Nochaiwong S, Ruengorn C, Awiphan R, Koyratkoson K, Chaisai C, Noppakun K, Chongruksut W, Thavorn K (2018) The association between proton pump inhibitor use and the risk of adverse kidney outcomes: a systematic review and meta-analysis. Nephrol Dial Transplant 33:331–342. https://doi.org/10.1093/ndt/gfw470
Yu L-Y, Sun L-N, Zhang X-H, Li Y-Q, Yu L, Yuan Z-Q-Y, Meng L, Zhang HW, Wang YQ (2017) A review of the novel application and potential adverse effects of proton pump inhibitors. Adv Ther 34:1070–1086. https://doi.org/10.1007/s12325-017-0532-9
Morita T, Tei Y, Tsunoda J, Inoue S, Chihara S (2001) Determinants of the sensation of thirst in terminally ill cancer patients. Support Care Cancer 9:177–186. https://doi.org/10.1007/s005200000205
Eilers J, Berger AM, Petersen MC (1988) Development, testing, and application of the oral assessment guide. Oncol Nurs Forum 15:325–330
Kohler PF, Winter ME (1985) A quantitative test for xerostomia. The Saxon test, an oral equivalent of the Schirmer test. Arthritis Rheum 28:1128–1132. https://doi.org/10.1002/art.1780281008
Safikhani S, Gries KS, Trudeau JJ, Reasner D, Rüdell K, Coons SJ, Bush EN, Hanlon J, Abraham L, Vernon M (2018) Response scale selection in adult pain measures: results from a literature review. J Patient-Report Outcomes 2:2. https://doi.org/10.1186/s41687-018-0053-6
Hartrick CT, Kovan JP, Shapiro S (2003) The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract 3:310–316. https://doi.org/10.1111/j.1530-7085.2003.03034.x
Acknowledgments
The authors would like to thank the palliative care doctors and all nurses at the Unit of Palliative Care, Kyoto Medical Center. The authors would also like to thank Editage (www.editage.com) for English language editing.
Funding
Funding for this development study was supported by the Sasakawa Health Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Review Board of the National Hospital Organization Kyoto Medical Center (approval ID: 16-076).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shimosato, M., Asai, K., Yokomichi, N. et al. Diagnostic accuracy of patient-reported dry mouth as a predictor for oral dryness in terminally ill cancer patients. Support Care Cancer 29, 2743–2748 (2021). https://doi.org/10.1007/s00520-020-05798-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05798-y