Abstract
Purpose
Prostate cancer (PCa) is the most commonly diagnosed cancer in Australia, accounting for one quarter of all new cancer diagnoses for males. Androgen deprivation therapy (ADT) is the standard first-line therapy for metastatic PCa but is also used across much of the spectrum of disease. Unfortunately, debilitating adverse effects are a significant and largely unavoidable feature of ADT. A recent systematic review of adverse effects of ADT identified 19 sub-groups classified according to the Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. The potential for multiple simultaneous adverse effects, their associated management and the impact of adverse effects on cancer outcomes and quality of life are important considerations in the treatment and supportive care of men with PCa. Exercise is increasingly being recognized as an efficacious strategy in managing these adverse effects.
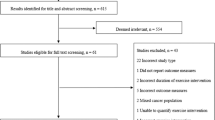
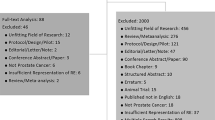
Methods
A rapid review was undertaken to examine the role of exercise in the management of the most commonly reported ADT adverse effects classified according to the CTCAE sub-groups. A systematic search was conducted in Medline, PsycINFO, Google Scholar and Google for the years 2010 to September 2019 to identify the benefits of exercise in managing the adverse effects of ADT for PCa.
Results
There is strong evidence for exercise as medicine in addressing several of the adverse effects of PCa such as loss of muscle mass and strength, fatigue and declining physical function. Moderate level evidence for PCa exists for exercise-induced improvements in depression and anxiety, bone loss, and sexual dysfunction. While evidence of the effectiveness of exercise is lacking for many adverse effects of ADT for PCa, evidence in the cancer population as a whole or other clinical populations is strong, and many clinical guidelines recommend exercise as a fundamental part of their clinical management. With the exception of gynaecomastia and breast pain, there is increasing evidence (PCa, cancer or other clinical populations) to suggest that exercise has the potential to reduce and even prevent many of the adverse effects of ADT, thus improving survivorship outcomes for men with PCa.
Conclusion
Exercise has the potential to reduce and even prevent many of the adverse effects of ADT, thus improving survivorship outcomes for men with PCa. The use of exercise for PCa management has the potential to translate into health and economic benefits in improved quality of life and fewer complications, resulting in savings to the health care system, enhanced productivity and reduced patient and carer burden. Exercise thus has the potential to improve quality of life for this population as well as generate significant cost savings.
Similar content being viewed by others
References
Australian Institute of Health and Welfare (AIHW) (2014) Cancer in Australia: an overview 2014. AIHW, Canberra
International Agency for Research on Cancer (IARC) (2019). Cancer today: prostate cancer 2018
Gordon L, Tuffaha H, James R, Keller A, Lowe A, Scuffham P et al (2018) Estimating the healthcare costs of treating prostate cancer in Australia: a Markov modelling analysis. Urol Oncol 36
National Comprehensive Cancer Network (NCCN) (2018) Clinical practice guidelines in oncology (NCCN guidelines) Prostate Cancer
Edmunds K, Tuffaha H, Galvão D, Scuffham P, Newton R (2020) Incidence of the adverse effects of androgen deprivation therapy for prostate cancer: a systematic review. Support Care Cancer 28:2079–2093. https://doi.org/10.1007/s00520-019-05255-5
National Institutes of Health and National Cancer Institute (2017) Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0
Vina J, Sanchis-Gomar F, Martinez-Bello V, Gomez-Cabrera M (2012) Exercise acts as a drug; the pharmacological benefits of exercise. Br J Pharmacol 167:1–12
Hayes S, Spence R, Galvão D, Newton R (2009) Australian Association for Exercise and Sport Science position stand: optimising cancer outcomes through exercise. J Sci Med Sport 12(4):428–434
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM et al (2010) American College of Sports Medicine roundtable on exercise: guidelines for cancer survivors. Med Sci Sports Exerc 42(7):1407–1426
Kenfield S, Stampfer M, Giovannucci E, Chan J (2011) Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol 29:726–732
Newton R, Galvão D (2013) Exercise medicine for prostate cancer. Eur Rev Ageing Phys Act 5:41–45. https://doi.org/10.1007/s11556-012-0114-4
Hayes S, Newton R, Spence R, Galvão D (2019) The exercise and sports science Australia position statement: exercise medicine in cancer management. J Sci Med Sport 22(11):1175–1199
Campbell K, Winters-Stone K, Wiskemann J, May A, Schwartz A, Courneya K et al (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51(11):2375–2390
Resnick MJ, Lacchetti C, Bergman J, Hauke RJ, Hoffman KE, Kungel TM, Morgans AK, Penson DF (2015) Prostate cancer survivorship care guideline: American society of clinical oncology clinical practice guideline endorsement. J Clin Oncol 33(9):1078–1085. https://doi.org/10.1200/JCO.2014.60.2557
National Comprehensive Cancer Network (NCCN) (2019) National Clinical Guidelines in Oncology (NCCN Guidelines) Survivorship Version 1.2019
National Institute for Health and Care Excellence (NICE) (2019). Prostate cancer: diagnosis and management. https://www.nice.org.uk/guidance/ng131
Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence Working Group (2016). The Oxford 2011 Levels of Evidence. http://www.cebm.net/index.aspx?o=5653
Grossmann M, Zajac JD (2011) Androgen deprivation therapy in men with prostate cancer: How should the side effects be monitored and treated? Clin Endocrinol (Oxf) 74(3):289–293. https://doi.org/10.1111/j.1365-2265.2010.03939.x
Joseph JS, Lam V, Patel MI (2019) Preventing osteoporosis in men taking androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. Eur Urol Oncol 2(5):551–561. https://doi.org/10.1016/j.euo.2018.11.001
Taaffe DR, Galvão DA, Spry N, Joseph D, Chambers SK, Gardiner RA, Hayne D, Cormie P, Shum DHK, Newton RU (2018) Immediate versus delayed exercise in men initiating androgen deprivation: effects on bone density and soft tissue composition. BJU Int 123(2):261–269. https://doi.org/10.1111/bju.14505
Uth J, Hornstrup T, Schmidt JF, Christensen JF, Frandsen C, Christensen KB, Helge EW, Brasso K, Rørth M, Midtgaard J, Krustrup P (2014) Football training improves lean body mass in men with prostate cancer undergoing androgen deprivation therapy. Scand J Med Sci Sports 24(SUPPL.1):105–112
Newton RU, Galvão DA, Spry N, Joseph D, Chambers SK, Gardiner RA et al (2018) Exercise mode specificity for preserving spine and hip bone mineral density in prostate cancer patients. Med Sci Sports Exerc 51(4):607–614. https://doi.org/10.1249/MSS.0000000000001831
Newton RU, Jeffery E, Galvão DA, Peddle-McIntyre CJ, Spry N, Joseph D et al (2018) Body composition, fatigue and exercise in patients with prostate cancer undergoing androgen-deprivation therapy. BJU Int 122(6):986–993. https://doi.org/10.1111/bju.14384
Baumann FT, Zopf EM, Bloch W (2012) Clinical exercise interventions in prostate cancer patients: a systematic review of randomized controlled trials. Support Care Cancer 20(2):221–233
Gardner JR, Livingston PM, Fraser SF (2014) Effects of exercise on treatment-related adverse effects for patients with prostate cancer receiving androgen-deprivation therapy: a systematic review. J Clin Oncol 32(4):335–346
Hasenoehrl T, Keilani M, Sedghi Komanadj T, Mickel M, Margreiter M, Marhold M, Crevenna R (2015) The effects of resistance exercise on physical performance and health-related quality of life in prostate cancer patients: a systematic review. Support Care Cancer 23(8):2479–2497. https://doi.org/10.1007/s00520-015-2782-x
Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, Albertsen PC, Tombal B, Payne HA, Rosario DJ (2016) Exercise for men with prostate cancer: a systematic review and meta-analysis. Eur Urol 69(4):693–703
Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, Sedghi Komandj T, Crevenna R (2017) Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer 25:2953–2968
Yunfeng G, Weiyang H, Xueyang H, Yilong H, Xin G (2017) Exercise overcome adverse effects among prostate cancer patients receiving androgen deprivation therapy. Medicine (United States) 96(27). https://doi.org/10.1097/MD.0000000000007368
Crawford-Williams F, March S, Goodwin BC, Ralph N, Galvão DA, Newton RU et al (2018) Interventions for prostate cancer survivorship: a systematic review of reviews. Psychooncology. 27:1339–2348
O’Neill RF, Haseen F, Murray LJ, O’Sullivan JM, Cantwell MM (2015) A randomised controlled trial to evaluate the efficacy of a 6-month dietary and physical activity intervention for patients receiving androgen deprivation therapy for prostate cancer. J Cancer Surviv 9(3):431–440. https://doi.org/10.1007/s11764-014-0417-8
Gilbert SE, Tew GA, Fairhurst C, Bourke L, Saxton JM, Winter EM, Rosario DJ (2016) Effects of a lifestyle intervention on endothelial function in men on long-term androgen deprivation therapy for prostate cancer. Br J Cancer 114(4):401–408. https://doi.org/10.1038/bjc.2015.479
Galvão DA, Taaffe DR, Spry N, Cormie P, Joseph D, Chambers SK et al (2018) Exercise preserves physical function in prostate cancer patients with bone metastases. Med Sci Sports Exerc 50(3):393–399. https://doi.org/10.1249/MSS.0000000000001454
Grossmann M, Zajac J (2011) Management of the side effects of androgen deprivation therapy. Endocrinol Metab Clin N Am 40(4):655–671. https://doi.org/10.1016/j.ecl.2011.05.004
Grossmann M, Hamilton EJ, Gilfillan C, Bolton D, Joon DL, Zajac JD (2011) Bone and metabolic health in patients with non-metastatic prostate cancer who are receiving androgen deprivation therapy. Med J Aust 194(6):301–306
Arnett D, Blumenthal R, Albert M, Buroker A, Goldberger Z, Hahn E, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy J, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 140:e596–e646. https://doi.org/10.1161/CIR.0000000000000678
Colberg S, Sigal R, Yardley J, Riddell M, Dunstan D, Dempsey P et al (2016) Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 39(11):2065–2079
The Royal Australian College of General Practitioners & Diabetes Australia. General practice management of type 2 diabetes 2016–2018. 2016
Collins L, Mohammed N, Ahmad T, Basaria S (2012) Androgen deprivation therapy for prostate cancer: implications for cardiometabolic clinical care. J Endocrinol Investig 35(3):332–339
Beaudry R, Liang Y, Boyton S, Tucker W, Brothers R, Daniel K et al (2018) Meta-analysis of exercise training on vascular endothelial function in cancer survivors. Integr Cancer Ther 17(2):192–199
Ahmadi H, Daneshmund S (2013) Androgen deprivation therapy: evidence-based management of side effects. BJU Int 111:543–548
Fagerlund A, Cormio L, Palangi L, Lewin R, Di Pompeo FS, Elander A et al (2015) Gynecomastia in patients with prostate cancer: a systematic review. PLoS ONE 10(8). https://doi.org/10.1371/journal.pone.0136094
Hamilton K, Chambers SK, Legg M, Oliffe JL, Cormie P (2015) Sexuality and exercise in men undergoing androgen deprivation therapy for prostate cancer. Support Care Cancer 23(1):133–142. https://doi.org/10.1007/s00520-014-2327-8
Cormie P, Newton R, Taaffe D, Saunders JD, Akhil Hamid M et al (2013) Exercise maintains sexual activity in men undergoing androgen suppression for prostate cancer: a randomized controlled trial. Prostate Cancer Prostatic Dis 16:170–175. https://doi.org/10.1038/pcan.2012.52
Chambers S, Dunn J, Lazenby M, Clutton S, Newton R, Cormie P et al (2013) ProsCare: a psychological care model for men with prostate cancer. Prostate Cancer Foundation of Australia (PCFA) and Griffith University, Australia
Chipperfield K, Brooker J, Fletcher J, Burney S (2014) The impact of physical activity on psychosocial outcomes in men receiving androgen deprivation therapy for prostate cancer: a systematic review. Health Psychol 33(11):1288–1297. https://doi.org/10.1037/hea0000006
Bourke L, Boorjian SA, Briganti A, Klotz L, Mucci L, Resnick MJ, Rosario DJ, Skolarus TA, Penson DF (2015) Survivorship and improving quality of life in men with prostate cancer. Eur Urol 68(3):374–383. https://doi.org/10.1016/j.eururo.2015.04.023
Keogh JWL, MacLeod RD (2012) Body composition, physical fitness, functional performance, quality of life, and fatigue benefits of exercise for prostate cancer patients: a systematic review. J Pain Sympt Manage 43(1):96–110. https://doi.org/10.1016/j.jpainsymman.2011.03.006
Baguley BJ, Bolam KA, Wright ORL, Skinner TL (2017) The effect of nutrition therapy and exercise on cancer-related fatigue and quality of life in men with prostate cancer. Nutrients. 9. https://doi.org/10.3390/nu9091003
Larkin D, Lopez V, Aromataris E (2014) Managing cancer-related fatigue in men with prostate cancer: a systematic review of non-pharmacological interventions. Int J Nurs Pract 20(5):549–560. https://doi.org/10.1111/ijn.12211
Moe E, Chadd J, McDonagh M, Valtonen M, Horner-Johnson W, Eden K et al (2017) Exercise interventions for prostate cancer survivors receiving hormone therapy: systematic review. Transl J Am Coll Sports Med 2(1):1-9. https://doi.org/10.1249/TJX.0000000000000025
Vashistha V, Singh B, Kaura S, Prokop L, Kaushik D (2016) The effects of exercise on fatigue, quality of life, and psychological function for men with prostate cancer: systematic review and meta-analyses. Eur Urol Focus 2:284–295
Taaffe DR, Newton RU, Spry N, Joseph D, Chambers SK, Gardiner RA, Wall BA, Cormie P, Bolam KA, Galvão DA (2017) Effects of different exercise modalities on fatigue in prostate cancer patients undergoing androgen deprivation therapy: a year-long randomised controlled trial. Eur Urol 72(2):293–299. https://doi.org/10.1016/j.eururo.2017.02.019
Segal R (2014) Physical functioning for prostate health. Can Urol Assoc J 8(7–8 Supplement 5):S162–S163. https://doi.org/10.5489/cuaj.2315
Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff Z, Howard K et al (2019) Exercise for preventing falls in older people living in the community (Review). Cochrane Database Syst Rev:CD012424(1). https://doi.org/10.1002/14651858.CD012424.pub2
Lin X, Zhang X, Guo J, Roberts C, McKenzie S, Wu W et al (2015) Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 4(7). https://doi.org/10.1161/JAHA.115.002014
Pan B, Ge L, Xun YQ, Chen YJ, Gao CY, Han X, Zuo LQ, Shan HQ, Yang KH, Ding GW, Tian JH (2018) Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. Int J Behav Nutr Phys Act 15(1):72. https://doi.org/10.1186/s12966-018-0703-3
Schellenberg E, Dryden D, Vandermeer B, Ha C, Korownyk C (2013) Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 159:543–551
Zanuso S, Sacchetti M, Sundberg CJ, Orlando G, Benvenuti P, Balducci S (2017) Exercise in type 2 diabetes: genetic, metabolic and neuromuscular adaptations. a review of the evidence. Br J Sports Med 51(21):1533–1538. https://doi.org/10.1136/bjsports-2016-096724
Scott J, Nilsen T, Gupta D, Jones L (2018) Exercise therapy and cardiovascular toxicity in cancer. Circulation. 137:1176–1191
Green DJ, Hopman MT, Padilla J, Laughlin MH, Thijssen DH (2017) Vascular adaptation to exercise in humans: role of hemodynamic stimuli. Physiol Rev 97(2):495–528
Janssen V, De Gucht V, Dusseldorp E, Maes S (2013) Lifestyle modification programmes for patients with coronary heart diease: a systematic review and meta-analysis of randomized controlled trials. Eur J Prevent Cardiol 20:620–640. https://doi.org/10.1177/2047487312462824
Northey J, Cherbuin N, Pumpa K, Smee D, Rattray B (2018) Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med 52(3):154–160
Blondell S, Hammersley-Mather R, Veerman J (2014) Does physical activity prevent cognitive decline and dementia? A systematic review and meta-analysis of longitudinal studies. BMC Public Health 14:510. https//doi.org/10.1186/1471-2458-14-510
Meschia J, Bushnell CB, Boden-Albala B, Braun L, Dawn M. Bravata D, Chaturvedi S et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3754–3832
Tsivgoulis G, Safouris A, Kim D-E, Alexandrovb A (2018) Recent advances in primary and secondary prevention of artherosclerotic stroke. J Stroke 20(2):145–166
Carlson D, Dieberg G, Hess N, Millar P, Smart N (2014) Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc 89(3):327–324
Carpio-Rivera E, Moncada-Jiménez J, Salazar-Rojas W, Solera-Herrera A (2016) Acute effects of exercise on blood pressure: a meta-analytic investigation. Arq Bras Cardiol 106(5):422–433. https://doi.org/10.5935/abc.20160064
Cornelissen V, Smart N (2013) Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc 2(1):e004473
Nelson MR, Doust JA (2013) Primary prevention of cardiovascular disease: new guidelines, technologies and therapies. Med J Aust 198(11):606–610. https://doi.org/10.5694/mja12.11054
National Vascular Disease Prevention Alliance (NVDPA) (2012) Guidelines for the management of absolute cardiovascular disease risk. NVDPA:1-124
Brook R, Appel L, Rubenfire M, Ogedegbe G, Bisognano J, Elliott W, Fuchs FD, Hughes JW, Lackland DT, Staffileno BA, Townsend RR, Rajagopalan S, American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity (2013) Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 61:1360–1383
Key N, Khorana A, Kuderer N, Bohlke K, Lee A, Arcelus J et al (2019) Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol 38(5):496–520
Kahn SR, Shrier I, Kearon C (2008) Physical activity in patients with deep venous thromboembolism: a systematic review. Thromb Res 122:763–773
Lambiase MJ, Thurston RC (2013) Physical activity and sleep among midlife women with vasomotor symptoms. Menopause (New York, NY) 20(9):946–952
Moilanen J, Aalto AM, Hemminki E, Aro AR, Raitanen J, Luoto R (2010) Prevalence of menopause symptoms and their association with lifestyle among Finnish middle-aged women. Maturitas. 67:368–374
van der Windt DJ, Sud V, Zhang H, Tsung A, Huang H (2018) The effects of physical exercise on fatty liver disease. Gene Expr 18:89–101
Golabi P, Locklear C, Austin P, Afdhal S, Byrns M, Gerber L et al (2016) Effectiveness of exercise in hepatic fat mobilization in non-alcoholic fatty liver disease: systematic review. World J Gastroenterol 22(27):6318–6327
Whitsett M, van Wagner L (2015) Physical activity as a treatment of non-alcoholic fatty liver disease: a systematic review. World J Hepatol 7(16):2041–2052
Schuch F, Vancampfort D, Richards J, Rosenbaum S, Ward P, Stubbs B (2016) Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res 77:42–51
Craft L, Vaniterson E, Helenowski I, Rademaker A, Courneya K (2012) Exercise effects on depressive symptoms in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev 21(1):3–19
Brown A, Huedo-Medina T, Pescatello L, Ryan S, Pescatello S, Moker E et al (2012) The efficacy of exercise in reducing depressive symptoms among cancer survivors: a meta-analysis. PLoS One 7(1):e30955 https://doi.org/10.1371/journal.pone.0030955
Mishra S, Scherer R, Geigle P, Berlanstein D, Topaloglu O, Gotay C et al (2012) Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Sys Rev. 8. https://doi.org/10.1002/14651858.CD007566.pub2
Mishra S, Scherer R, Snyder C, Geigle P, Berlanstein D, Topaloglu O (2012) Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Sys Rev 8. https://doi.org/10.1002/14651858.CD008465.pub2
Fong D, Ho J, Hui B, Lee A, Macfarlane D, Leung S et al (2012) Physical activity for cancer survivors: meta-analysis of randomised controlled trials. BMJ (Online) 344:e70. https://doi.org/10.1136/bmj.e70
Winters-Stone KM, Dobek JC, Bennett JA, Maddalozzo GF, Ryan CW, Beer TM (2014) Skeletal response to resistance and impact training in prostate cancer survivors. Med Sci Sports Exerc 46(8):1482–1488. https://doi.org/10.1249/MSS.0000000000000265
Pernar CH, Ebot EM, Wilson KM, Mucci LA (2018) The epidemiology of prostate cancer. CSH Perspecti Med 8(12). https://doi.org/10.1101/cshperspect.a030361
Greasely R, Turner R, Collins K, Brown J, Bourke L, Rosario D (2018) Treatment in the STAMPEDE for castrate resistant prostate cancer in the UK: ongoing challenges and underappreciated clinical problems. BMC Cancer 18:667. https://doi.org/10.1186/s12885-018-4527-y
Bourke L, Turner R, Greasley R, Sutton E, Steed L, Smith D et al (2018) A multi-centre investigation of delivering national guidelines on exercise training for men with advanced prostate cancer undergoing androgen deprivation therapy in the UK NHS. PLoS ONE 13(7):e0197606-e. https://doi.org/10.1371/journal.pone.0197606
Schmidt M, Østergren P, Cormie P, Ragle A, Sønksen J, Midtgaard J (2019) “Kicked out into the real world”: prostate cancer patients' experiences with transitioning from hospital-based supervised exercise to unsupervised exercise in the community. Support Care Cancer 27(1):199–208
Funding
Kim Edmunds’ PhD was supported by an Australian Post Graduate Awards (APA) scholarship and an Inspiring Minds scholarship from Edith Cowan University, Western Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Edmunds, K., Tuffaha, H., Scuffham, P. et al. The role of exercise in the management of adverse effects of androgen deprivation therapy for prostate cancer: a rapid review. Support Care Cancer 28, 5661–5671 (2020). https://doi.org/10.1007/s00520-020-05637-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05637-0