Abstract
Objective
The purpose of this study was to estimate prevalence/severity of self-reported trismus, determine association with quality of life (QOL), and examine clinical risk factors in a large population of patients treated for oropharyngeal cancer.
Materials and methods
A cross-sectional survivorship survey was conducted among patients who completed definitive treatment for oropharyngeal carcinoma, disease-free ≥ 1-year post-treatment (median survival, 7 years among 892 survivors). Associations between trismus and QOL were also analyzed using MDASI-HN, EQ-5D, and MDADI. Dietary and feeding tube status were also correlated to trismus status.
Results
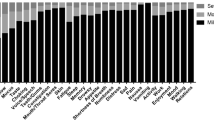
Trismus was self-reported in 31%. Severity of trismus positively correlated (r = 0.29) with higher mean interference scores reflecting a moderate association with quality of life (p < 0.0001). There was a negative correlation for MDADI composite scores (r = − 0.33) indicating increased perceived dysphagia related to trismus severity (p < 0.0001). EQ-5D VAS scores were also negatively correlated with trismus severity (r = − 0.26, p < 0.0001). Larger T-stage (p ≤ 0.001), larger nodal stage (p = 0.03), tumor sub-site (p = 0.05), and concurrent chemoradiation (p = 0.01) associated with increased prevalence of trismus. Diet negatively correlated (r = − 0.27) with trismus severity (p = < 0.0001), and survivors with severe trismus were also more likely to be feeding tube-dependent.
Conclusion
Severity of trismus appears to negatively impact quality of life and associate with various adverse functional outcomes in long-term oropharyngeal cancer survivorship. Trismus remains associated with advanced disease stages, tumor sub-site (tonsil), and addition of chemotherapy. Further investigation is merited for the dose-effect relationship to the muscles of mastication.




Similar content being viewed by others
References
Rutten H et al (2011) Long-term outcome and morbidity after treatment with accelerated radiotherapy and weekly cisplatin for locally advanced head-and-neck cancer: results of a multidisciplinary late morbidity clinic. Int J Radiat Oncol Biol Phys 81(4):923–929
Davies A, Epstein J (2010) Oral complications of cancer and its management. OUP Oxford
Louise Kent M, Brennan MT, Noll JL, Fox PC, Burri SH, Hunter JC, Lockhart PB (2008) Radiation-induced trismus in head and neck cancer patients. Support Care Cancer 16(3):305–309
Dijkstra PU, Kalk WW, Roodenburg JL (2004) Trismus in head and neck oncology: a systematic review. Oral Oncol 40(9):879–889
Rapidis AD, Dijkstra PU, Roodenburg JLN, Rodrigo JP, Rinaldo A, Strojan P, Takes RP, Ferlito A (2015) Trismus in patients with head and neck cancer: etiopathogenesis, diagnosis and management. Clin Otolaryngol 40(6):516–526
Dijkstra PU, Huisman PM, Roodenburg JL (2006) Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg 35(4):337–42
Agerberg G, Osterberg T (1974) Maximal mandibular movements and symptoms of mandibular dysfunction in 70-year old men and women. Sven Tandlak Tidskr 67(3):147–163
Landtwing K (1978) Evaluation of the normal range of vertical mandibular opening in children and adolescents with special reference to age and stature. J Maxillofac Surg 6(3):157–162
Zawawi KH et al (2003) An index for the measurement of normal maximum mouth opening. J Can Dent Assoc 69(11):737–741
Scott B, Butterworth C, Lowe D, Rogers SN (2008) Factors associated with restricted mouth opening and its relationship to health-related quality of life in patients attending a Maxillofacial Oncology clinic. Oral Oncol 44(5):430–438
Kamstra JI, van Leeuwen M, Roodenburg JLN, Dijkstra PU (2017) Exercise therapy for trismus secondary to head and neck cancer: a systematic review. Head Neck 39(11):2352–2362
Lyons AJ, Crichton S, Pezier T (2013) Trismus following radiotherapy to the head and neck is likely to have distinct genotype dependent cause. Oral Oncol 49(9):932–936
Kamstra JI, Dijkstra PU, van Leeuwen M, Roodenburg JLN, Langendijk JA (2015) Mouth opening in patients irradiated for head and neck cancer: a prospective repeated measures study. Oral Oncol 51(5):548–555
Lee R, Slevin N, Musgrove B, Swindell R, Molassiotis A (2012) Prediction of post-treatment trismus in head and neck cancer patients. Br J Oral Maxillofac Surg 50(4):328–332
van der Geer SJ, et al. (2020) Prognostic factors associated with a restricted mouth opening (trismus) in patients with head and neck cancer: systematic review. Head Neck
Beumer J, Marunick MT, Esposito SJ (2011) Maxillofacial rehabilitation: prosthodontic and surgical management of cancer-related, acquired, and congenital defects of the head and neck, 3rd edn. Quintessence Pub. xv, Hanover Park 452 p
Ou X, Zhou X, Shi Q, Xing X, Yang Y, Xu T, Shen C, Wang X, He X, Kong L, Ying H, Hu C (2015) Treatment outcomes and late toxicities of 869 patients with nasopharyngeal carcinoma treated with definitive intensity modulated radiation therapy: new insight into the value of total dose of cisplatin and radiation boost. Oncotarget 6(35):38381–38397
Watters AL, Cope S, Keller MN, Padilla M, Enciso R (2019) Prevalence of trismus in patients with head and neck cancer: a systematic review with meta-analysis. Head Neck 41(9):3408–3421
Wang CJ, Huang EY, Hsu HC, Chen HC, Fang FM, Hsiung CY (2005) The degree and time-course assessment of radiation-induced trismus occurring after radiotherapy for nasopharyngeal cancer. Laryngoscope 115(8):1458–1460
Rosenthal DI, Mendoza TR, Chambers MS, Asper JA, Gning I, Kies MS, Weber RS, Lewin JS, Garden AS, Ang KK, S. Wang X, Cleeland CS (2007) Measuring head and neck cancer symptom burden: the development and validation of the M. D. Anderson symptom inventory, head and neck module. Head Neck 29(10):923–931
Balestroni G, Bertolotti G (2012) EuroQol-5D (EQ-5D): an instrument for measuring quality of life. Monaldi Arch Chest Dis 78(3):155–159
Hutcheson KA, Barrow MP, Lisec A, Barringer DA, Gries K, Lewin JS (2016) What is a clinically relevant difference in MDADI scores between groups of head and neck cancer patients? Laryngoscope 126(5):1108–1113
Pezzuto F, Buonaguro L, Caponigro F, Ionna F, Starita N, Annunziata C, Buonaguro FM, Tornesello ML (2015) Update on head and neck cancer: current knowledge on epidemiology, risk factors, molecular features and novel therapies. Oncology 89(3):125–136
Pytynia KB, Dahlstrom KR, Sturgis EM (2014) Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol 50(5):380–386
Simard EP, Torre LA, Jemal A (2014) International trends in head and neck cancer incidence rates: differences by country, sex and anatomic site. Oral Oncol 50(5):387–403
Goldstein M, Maxymiw WG, Cummings BJ, Wood RE (1999) The effects of antitumor irradiation on mandibular opening and mobility: a prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88(3):365–373
Pauli N, Johnson J, Finizia C, Andréll P (2012) The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncologica 52(6):1137–1145
Funding
This work was directly supported by the Charles and Daneen Stiefel Oropharynx Fund at the University of Texas MD Anderson Cancer Center.
Author information
Authors and Affiliations
Contributions
All listed co-authors performed the following:
1. Substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data for the work;
2. Drafting the work or revising it critically for important intellectual content;
3. Final approval of the version to be published;
4. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Specific additional individual cooperative effort contributions to study/manuscript design/execution/interpretation, in addition to all criteria above, are listed as follows:
RC, MK, JZ, HM, -Drafted manuscript, undertook supervised analysis and interpretation of data.
KH- Corresponding author; principal investigator; conceived, coordinated, and directed all study activities, responsible for data collection, project integrity, data collection infrastructure, programmatic oversight, direct oversight of classified personnel, manuscript content, and editorial oversight and correspondence.
MC, GBG, CDF, SYL, FM – Co-investigators; direct patient care provision, direct toxicity assessment, and clinical data collection; interpretation and analytic support.
JZ-Data coordination, collection, curation, and supervised analysis.
Corresponding author
Ethics declarations
Conflict of interest
RC: This author declares that he has no conflict of interest.
MK: This author declares that she has no conflict of interest.
JZ: This author declares that she has no conflict of interest.
MC: This author declares that he has no conflict of interest.
GBG: This author declares that he has no conflict of interest.
CF: This author declares that he has conflicts of interest as listed on the COI form.
SL: This author declares that he has no conflict of interest.
FM: This author declares that he has no conflict of interest.
HM: This author declares that she has no conflict of interest.
KH: This author declares that she has conflicts of interest as listed on the COI form.
Ethical approval
Ethical approval was waived by the local Ethics Committee of the University of Texas, M.D. Anderson Cancer Center, in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care. Approval for this study was granted by the institutional review board of The University of Texas, M.D. Anderson Cancer Center, PA11-0936.
Consent to participate
Informed consent was obtained by all individual participants included in the study.
Consent to publish
All authors provided consent to publish this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cardoso, R.C., Kamal, M., Zaveri, J. et al. Self-Reported Trismus: prevalence, severity and impact on quality of life in oropharyngeal cancer survivorship: a cross-sectional survey report from a comprehensive cancer center. Support Care Cancer 29, 1825–1835 (2021). https://doi.org/10.1007/s00520-020-05630-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05630-7