Abstract
Objective
To compare sexual function and quality of life (QoL) in breast cancer survivors with and without a history of bilateral salpingo-oophorectomy (BSO).
Methods
A cross-sectional study of breast cancer survivors treated at a tertiary referral hospital in Western Australia. The Female Sexual Function Index was used to determine rates of female sexual dysfunction (FSD) and hypoactive sexual desire disorder (HSDD). Participants also completed the Relationship Assessment Scale, Menopause-specific quality of life questionnaire and Short Form Health Survey-36.
Results
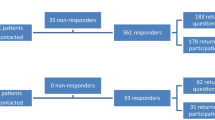
A total of 427 women were invited to participate: 119 had undergone BSO and 308 were controls with at least one ovary remaining. A total of 172 women participated (overall response rate 40.3%), consisting of 76 women in the BSO group (response rate 63.9%) and 96 women with at least one ovary remaining (response rate 31.2%). There was no difference in FSD between the two groups: 63/76 (82.9%) women who had undergone BSO had FSD compared to 75/96 (78.1%) controls (p = 0.458). No difference in HSDD was observed (p = 0.084) between the BSO group 70/76 (96.0%) and the controls 96/96 (100%). Women who had undergone BSO had lower general health scores compared to the control group (p = 0.034). Both groups had similar energy levels, emotional well-being, pain scores, physical functioning levels and social functioning levels.
Conclusions
In this study, women with prior treatment for breast cancer had high levels of FSD and HSDD, irrespective of whether they had undergone BSO. Both groups reported similar sexual function scores and QoL.
Similar content being viewed by others
References
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin
Breast Cancer Network Australia. https://www.bcna.org.au/media/7111/bcna-2019-current-breast-cancer-statistics-in-australia-11jan2019.pdf. Accessed 4th Aug 2019
Gandhi C, Butler E, Pesek S, Kwait R, Edmonson D, Raker C, Clark MA, Stuckey A, Gass J (2019) Sexual dysfunction in breast Cancer survivors: is it surgical modality or adjuvant therapy? Am J Clin Oncol 42(6):500–506
Jing L, Zhang C, Li W, Jin F, Wang A (2019) Incidence and severity of sexual dysfunction among women with breast cancer: a meta-analysis based on female sexual function index. Support Care Cancer 27(4):1171–1180
Fallowfield L, Jenkins V (2015) Psychosocial/survivorship issues in breast cancer: are we doing better? J Natl Cancer Inst 107(1):335
Tucker PE, Saunders C, Bulsara MK, Tan JJS, Salfinger SG, Green H, Cohen PA (2016) Sexuality and quality of life in women with a prior diagnosis of breast cancer after risk-reducing salpingo-oophorectomy. Breast 30:26–31
Beatson GT (1896) On the treatment of inoperable cases of carcinoma of the mamma: suggestions for a new method of treatment, with illustrative cases. Trans Med Chir Soc Edinb 15:153–179
Saha P, Regan MM, Pagani O, Francis PA, Walley BA, Ribi K, Bernhard J, Luo W, Gómez HL, Burstein HJ, Parmar V, Torres R, Stewart J, Bellet M, Perelló A, Dane F, Moreira A, Vorobiof D, Nottage M, Price KN, Coates AS, Goldhirsch A, Gelber RD, Colleoni M, Fleming GF, for the SOFT, TEXT Investigators, the International Breast Cancer Study Group (2017) Treatment efficacy, adherence, and quality of life among women younger than 35 years in the international breast Cancer study group TEXT and SOFT adjuvant endocrine therapy trials. J Clin Oncol 35(27):3113–3122
Pagani O, Regan MM, Walley BA, Fleming GF, Colleoni M, Láng I, Gomez HL, Tondini C, Burstein HJ, Perez EA, Ciruelos E, Stearns V, Bonnefoi HR, Martino S, Geyer CE Jr, Pinotti G, Puglisi F, Crivellari D, Ruhstaller T, Winer EP, Rabaglio-Poretti M, Maibach R, Ruepp B, Giobbie-Hurder A, Price KN, Bernhard J, Luo W, Ribi K, Viale G, Coates AS, Gelber RD, Goldhirsch A, Francis PA, TEXT and SOFT Investigators, International Breast Cancer Study Group (2014) Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med 371(2):107–118
Manahan ER, Kuerer HM, Sebastian M, Hughes KS, Boughey JC, Euhus DM, Boolbol SK, Taylor WA (2019) Consensus guidelines on genetic` testing for hereditary breast cancer from the American Society of Breast Surgeons. Ann Surg Oncol 26:3025–3031
Cancer Genome Atlas, N (2012) Comprehensive molecular portraits of human breast tumours. Nature 490(7418):61–70
Hartmann LC, Lindor NM (2016) The role of risk-reducing surgery in hereditary breast and ovarian cancer. N Engl J Med 374(5):454–468
Yang G, Nowsheen S, Aziz K, Georgakilas AG (2013) Toxicity and adverse effects of Tamoxifen and other anti-estrogen drugs. Pharmacol Ther (Oxford) 139(3):392–404
Baumgart J, Nilsson K, Evers AS, Kallak TK, Poromaa IS (2013) Sexual dysfunction in women on adjuvant endocrine therapy after breast cancer. Menopause 20(2):162–168
Francis PA, Pagani O, Fleming GF, Walley BA, Colleoni M, Láng I, Gómez HL, Tondini C, Ciruelos E, Burstein HJ, Bonnefoi HR, Bellet M, Martino S, Geyer CE Jr, Goetz MP, Stearns V, Pinotti G, Puglisi F, Spazzapan S, Climent MA, Pavesi L, Ruhstaller T, Davidson NE, Coleman R, Debled M, Buchholz S, Ingle JN, Winer EP, Maibach R, Rabaglio-Poretti M, Ruepp B, di Leo A, Coates AS, Gelber RD, Goldhirsch A, Regan MM, SOFT and TEXT Investigators and the International Breast Cancer Study Group (2018) Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med 379(2):122–137
Burstein HJ, Curigliano G, Loibl S, Dubsky P, Gnant M, Poortmans P, Colleoni M, Denkert C, Piccart-Gebhart M, Regan M, Senn HJ, Winer EP, Thurlimann B, Members of the St. Gallen International Consensus Panel on the Primary Therapy of Early Breast Cancer 2019 (2019) Estimating the benefits of therapy for early stage breast cancerThe St Gallen International Consensus Guidelines for the Primary Therapy of Early Breast Cancer 2019. Ann Oncol 30:1541–1557
Cohen PA, Brennan A, Marino JL, Saunders CM, Hickey M (2017) Managing menopausal symptoms after breast cancer - a multidisciplinary approach. Maturitas 105:4–7
Rosen R et al (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26(2):191–208
Meyer-Bahlburg HFL, Dolezal C (2007) The female sexual function index: a methodological critique and suggestions for improvement. J Sex Marital Ther 33(3):217–224
Wiegel M, Meston C, Rosen R (2005) The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31(1):1–20
Gerstenberger EP, Rosen RC, Brewer JV, Meston CM, Brotto LA, Wiegel M, Sand M (2010) Sexual desire and the female sexual function index (FSFI): a sexual desire cutpoint for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. J Sex Med 7(9):3096–3103
Hendrick S (1988) A generic measure of relationship satisfaction. J Marriage Fam 50(1):93–98
Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, Guyatt GH, Nortona PG, Dunn E (2008) A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas 61(1–2):107–121
Ware J, Sherbourne C (1992) The MOS 36-item short-form health survey (SF-36). Med Care 30(6):473–483
Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake L (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Bmj 305(6846):160–164
Aerts L, Christiaens MR, Enzlin P, Neven P, Amant F (2014) Sexual functioning in women after mastectomy versus breast conserving therapy for early-stage breast cancer: a prospective controlled study. Breast 23(5):629–636
Schover LR, Baum GP, Fuson LA, Brewster A, Melhem-Bertrandt A (2014) Sexual problems during the first 2 years of adjuvant treatment with aromatase inhibitors. J Sex Med 11(12):3102–3111
Lewis RW, Fugl-Meyer KS, Bosch R, Fugl-Meyer AR, Laumann EO, Lizza E, Martin-Morales A (2004) Epidemiology/ risk factors of sexual dysfunction. J Sex Med 1(1):35–39
Laumann EO, Paik A, Rosen R (1999) Sexual dysfunction in the United States: prevalence and predictors. JAMA 281(6):537–544
Acknowledgements
The authors gratefully acknowledge the women who participated in this study.
Funding
This study was funded by St John of God Subiaco Hospital, Perth, Western Australia. Dr. Paige Tucker is a PhD Student at the University of Notre Dame Australia, Fremantle and is supported by a scholarship funded through the St John of God Foundation by a donation from the Kailis Family Foundation, Leederville.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tucker, P.E., Cohen, P.A., Bulsara, M.K. et al. The impact of bilateral salpingo-oophorectomy on sexuality and quality of life in women with breast cancer. Support Care Cancer 29, 369–375 (2021). https://doi.org/10.1007/s00520-020-05503-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05503-z