Abstract
Purpose
Hodgkin lymphoma (HL) survivors face long-term, elevated risk of treatment-related sequelae, including psychosocial distress associated with poor health outcomes. The magnitude and sources of distress are not well described in the routine care of HL outside of clinical trials.
Methods
We conducted a retrospective cohort study of patients visiting a tertiary-care center for treatment or long-term follow-up of HL. Patient-reported distress was documented using the National Comprehensive Cancer Network Distress Thermometer (DT) and Problem List. Three survivor groups were compared using descriptive methods: on treatment, surviving < 5 years, and surviving ≥ 5 years since diagnosis.
Results
A total of 1524 DT were abstracted for 304 patients (106 on treatment, 77 surviving < 5 years, and 121 surviving ≥ 5 years). Distress was low overall (median DT = 1, inter-quartile range 0–4) and was similar across survivor groups. However, actionable distress (score ≥ 4) was reported at 29.5% of clinical encounters. Patients on treatment more frequently reported actionable distress (32.5% of visits) compared with patients surviving < 5 years (20.4%) and ≥ 5 years (28.7%) (P = 0.065). Distress was associated primarily with physical and emotional problems, especially fatigue, worry, and sleep. We did not observe any associations between distress and clinical prognostic factors.
Conclusions
Distress burden is low in HL, but survivorship is marked by periods of actionable distress, largely related to physical symptoms and emotional issues. This burden may be higher when on treatment and is unrelated to disease-related prognostic factors. Survivorship research typically focuses on the post-therapy period, but our results support testing the efficacy of interventions to address distress in HL during active treatment as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Purpose
More than 200,000 Americans are living with Hodgkin lymphoma (HL), a hematologic malignancy with a 5-year survival rate of 86.4% [1]. Although prognosis for most people with HL is generally quite good, first-line treatments are associated with an increased risk of therapy-related complications, including cardiovascular disease and second cancers for 15–25 years post-treatment [2]. HL survivors also face psychosocial complications of cancer survivorship that may interfere with tasks of daily living, reduce quality of life, and impact physical health [3]. The National Comprehensive Cancer Network (NCCN) refers to these complications as distress: “…a multifactorial unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms and its treatment” [4].
In an early study of distress in cancer, 33% of patients self-reported distress within 4 years of diagnosis [5]. The prevalence of distress among the 135 HL patients in this study was 37.8% [5]. Similarly, in a longitudinal analysis of 161 HL patients participating in a clinical trial, symptom distress increased from the pre-treatment period to 6 months post-treatment, returned to baseline levels at 1 year, and persisted at 2 years post-treatment [6]. Results of these studies may not represent the current profile of distress in HL, however, as treatment approaches evolved [7,8,9,10,11,12] and recommendations for managing late effects in HL survivors [2] emerged during the 15 years since these studies were published. In addition, clinical trial participants differ from patients receiving treatment in a non-experimental setting [13]. More recent studies estimating the prevalence of distress in hematologic malignancies have not distinguished between leukemias and lymphomas [14], have not described distress separately in HL and non-Hodgkin lymphoma [15, 16] or have evaluated distress in HL patients receiving a bone marrow transplant [17], which represents a minority of HL cases. Furthermore, we are unaware of any studies that evaluated differences in symptom distress among patients on active therapy vs. longer-term survivors outside of clinical trials [18, 19]. Understanding self-reported distress is important for improving the experience of HL survivors, e.g., by informing development of personalized survivorship care plans and coordinating care between medical and mental health specialties [20].
We hypothesized that distress is common in HL, but that the magnitude and sources of distress vary in patients on active therapy compared with those who survive for longer periods thereafter. We tested this hypothesis via a retrospective review of a large cohort of HL survivors visiting outpatient clinics at a Comprehensive Cancer Center. Our objective was twofold: First, to inform the clinician who cares for HL survivors by describing the magnitude and sources of patient-reported distress, and second, to assist HL survivors in understanding what to expect as they progress through different survivorship periods. Therefore, we described distress using a validated, point-of-care, patient-reported distress screening tool used routinely at our institution: the NCCN Distress Thermometer (DT) [21]. Patients in our study were visiting the Cancer Center for chemo/radiotherapy or for long-term follow-up after treatment for HL, enabling us to evaluate distress across the continuum of HL survivorship.
Methods
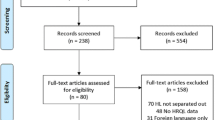
Study design
We conducted a single-institution, retrospective cohort study using data abstracted from electronic medical records (EMR) of patients visiting the Duke Cancer Institute (DCI) for treatment or long-term follow-up of HL. Eligible patients had pathologically confirmed HL, were over 18 at the time of their first visit at the DCI, and were seen in outpatient clinics between July 1, 2013, and November 16, 2016. The study was approved by the Duke Institutional Review Board prior to data collection.
The cohort of HL patients was divided into three groups representing samples of distinct survivorship periods: on treatment; not on treatment and surviving < 5 years; or not on treatment and surviving ≥ 5 years since diagnosis. Therefore, our study looks back at three non-overlapping groups of participants who reached different survivorship milestones and describes distress experienced during each survivorship period.
Data collection procedures
Demographics, disease characteristics, treatment regimens, and patient-reported distress were manually abstracted from the EMR and entered into REDCap [22]. Patient-reported distress is assessed as part of routine care at DCI clinics using the NCCN DT, reported by patients on paper forms and entered into a structured reporting tool in the clinical “visit navigator” of the Epic EMR. The DT includes an 11-point scale reflecting the patient’s overall distress level for the previous week (0 to 10), and an accompanying 39-item “problem list” (PL) that allows patients to indicate the sources of their distress using yes/no answers [21]. Previous research validated the DT against the Hospital Anxiety and Depression Scale and demonstrated that DT ≥ 4 is an optimal cutoff for identifying distress in cancer patients [23] and is considered evidence of clinically significant distress [4]. Nursing staff utilize these results during the intake process to trigger referrals to available support resources in the DCI (e.g., social work, family therapy, or financial counseling). We abstracted the DT score and accompanying PL items, when available, from each documented clinical encounter for all eligible patients. Because reasons for missing DT/PL are not recorded in the EMR, we evaluated the pattern of missing DT/PL across the comparison groups of interest to assess differential compliance.
Dependent and independent variables
The primary-dependent variables were the DT score (an ordinal scale from 0 [no distress] to 10), the occurrence of “actionable distress” (yes/no; using the threshold of DT ≥ 4 discussed previously) [23], report of individual items on the PL (39 yes/no variables), and report of any problem within each of the five domains of the PL: practical, family, emotional, and physical problems, or spiritual/religious concerns. The NCCN DT has been validated in various oncology populations against other patient-reported outcomes assessing anxiety/depression, like the Hospital Anxiety and Depression Scale and the Brief Symptom Inventory [23].
The primary independent variable of interest was survivorship status as described above, which we defined based on time elapsed from diagnosis to the first visit during our study. Only 23 patients in the surviving ≥ 5 years group transitioned status during our study; i.e., they began the study with less than 5 years of survival time (median = 2, range = 1–4 years), supporting our decision to define these groups on the basis of each patient’s status at the index study visit. We also evaluated age at diagnosis, sex, disease stage and risk stratification using the Lugano classification [24], pathologic subtype (classical vs. nodular lymphocyte predominant HL), and Charlson comorbidity index. Patients who were on treatment were also analyzed according to treatment modality (chemotherapy only, chemo/radiotherapy, or radiotherapy only).
Statistical analysis
Our approach evaluated the typical clinical dynamic of distress in HL using descriptive methods. The unit of observation in these analyses was the clinical encounter, at which a single survey is taken per patient, and multiple such encounters are present for each patient. Modeling of putative risk factors for actionable distress was done using generalized estimating equations to adjust standard errors due to the contribution of multiple visits per patient. All analyses were done using SAS v9.4 (SAS Institute, Cary, NC).
Results
Data were abstracted for 304 patients (Table 1) with median age at diagnosis of 34 years. Slightly more than half (56%) had stage I/II disease, and 25% had early/favorable prognosis. A total of 106 (34.9%) received therapy during the study period with 72% receiving chemotherapy only, 24% receiving chemo/radiotherapy, and 5% treated with radiotherapy alone. Ninety-five of these patients were receiving treatment for newly diagnosed disease, whereas 11 were receiving treatment for relapsed disease. Seventy-seven patients (25.3%) were attending follow-up clinics after surviving less than 5 years (mean = 2.13 years, standard deviation [SD] = 1.54), and 121 (39.8%) were in follow-up for 5 or more years since diagnosis (mean = 16.35 years, SD = 8.87).
Patient-reported distress
Compliance with routine distress screening was high, with a DT and PL collected at over 70% of clinical encounters, and compliance was similar across the three survivor cohorts (Table 2). This is similar to the typical completion rate seen with longitudinal, patient-reported outcomes collected in clinical trials, with high-quality cooperative group trials sometimes achieving 85–95% adherence, and other studies often achieving just 50–75% adherence, especially as time passes [25, 26]. A median of 3 DT/patient were abstracted (interquartile range [IQR] 1–7, range 1–47). Only one participant did not contribute any DT, and the number of DT per patient was unrelated to average distress (Pearson’s r = 0.006, P = 0.99). Distress scores were low overall (median DT = 1, IQR 0–4). However, the frequency of actionable distress (a score of ≥ 4) was high in the entire cohort, being reported at 29.5% of visits. Our analysis of predictors of actionable distress suggests that survivorship status is potentially important (P = 0.067; Table 3). In particular, we noted that patients on treatment reported actionable distress at 300/924 visits (32.5%), whereas this frequency was 55/269 (20.4%) in those surviving < 5 years and 95/331 (28.7%) in patients surviving ≥ 5 years. In multivariable modeling, we found that age, sex, pathologic subtype, risk strata, stage at diagnosis, and comorbidity score were unrelated to actionable distress.
Sources of distress identified on the problem list
Figure 1 shows the frequency of problem reports, as a percentage of clinical encounters, across the survivorship groups. A similar pattern is evident within each group. Physical problems are the most frequent, followed by emotional, practical, and family/spiritual problems. Physical problems were reported at 58.1% of visits in patients on treatment but only at 40.3% and 42.8% of visits in patients surviving < 5 and ≥ 5 years, respectively. The frequency of other types of problems was not appreciably different between the groups.
Frequency of problem reports by domain and survivorship status. Bars show the percent of visits occurring within each survivorship group where problems were reported. For example, family/spiritual problems were reported at 8.2% of visits among patients on treatment, 10.0% of visits among patients surviving < 5 years, and 9.6% of visits among patients surviving ≥ 5 years. The total number of visits per group is shown in Table 2. Some patients contribute more than one visit
The five most frequently reported distressing problems were fatigue (614 reports, 9.8% of problems), pain (417, 6.7%), worry (384, 6.1%), tingling in hands/feet (372, 6.0%), and sleep (341, 5.5%). Figure 2 shows how frequently these problems were endorsed at clinical encounters where a problem list was collected. Nearly half of the problem lists (43.8%) submitted in the on treatment group included reports of fatigue, whereas only ~ 25–30% of problem lists submitted by the longer-term survivor groups included fatigue. Tingling in the hands and feet was the only other symptom that appeared more frequently in problem lists submitted by patients on treatment (~ 28%) compared with short- and long-term survivors (~ 12–16%).
Top five most frequently reported problems by survivorship status. Bars show the proportion of problem lists in which the symptom was reported. The total number of problem lists submitted in each group is shown in Table 2. Some participants submitted multiple problem lists
Since fatigue was the most commonly reported symptom, we also investigated whether other symptoms were likely to be reported concurrently. Among the 614 cases of self-reported fatigue in this study, a total of 220 (35.8%) were accompanied by simultaneous reports of nervousness, 156 reports of depression (25.4%), 128 reports of sadness (20.8%), 120 reports of fear (19.5%), and 109 cases of loss of interest in usual activities (17.8%). Other symptoms were reported with markedly lower frequency in combination with fatigue (not shown).
Conclusions
This retrospective review of patient-reported distress in HL survivors under routine clinical observation outside of a clinical trial revealed three important findings. First, although distress is low in HL overall, actionable distress is commonly observed at ~ 30% of clinical encounters. This frequency may be highest in patients receiving treatment. Second, the frequency of actionable distress was not associated with disease-related prognostic factors. Third, physical problems were the primary source of distress among all survivors, and the majority of problems were reported by patients on active therapy.
Our observation of significant risk of actionable distress in HL patients on treatment expands upon the findings of a previous study that employed a modified, Dutch-language version of the DT [27] in a cohort of 29 lymphoma patients (12 HL and 17 non-Hodgkin lymphoma [NHL]) [28]. This study reported that 4/12 (33%) recently diagnosed HL/NHL patients had prevalent actionable distress (DT ≥ 4) prior to the start of therapy; this declined to 14% after 3 weeks of chemotherapy, and to only 9% at 5 weeks after completion of therapy [28]. In our larger cohort of exclusively HL patients, we noted a similar trend in which DT ≥ 4 was reported at one third of clinical encounters among patients on active therapy, and this declined to one fifth of encounters among those surviving < 5 years and not currently on treatment. This suggests that actionable distress is common in actively treated HL patients and emphasizes the importance of continually monitoring changes in patients’ distress level during treatment. Other studies that evaluated peri-treatment distress in HL did not specifically address the active therapy period, so this novel finding calls for further research, and ultimately intervention development to improve patients’ experiences of illness when undergoing treatment for HL [5, 6]. This sizeable burden of symptoms should be remediable with targeted intervention. For example, studies testing integrated specialist palliative care interventions among patients with advanced cancer receiving active therapy demonstrate significant benefits in symptom management, quality of life improvement, and mood [29,30,31,32]. A randomized clinical trial of such an intervention during stem cell transplantation yielded similar outcome improvements, thus shifting the typical population receiving palliative care to one receiving curative-intent therapy [33]. Our findings raise the possibility that such an intervention could help HL patients as well, during the period of active therapy. Although most HL patients have a good long-term outcome, there is still significant potential for benefit from such an intervention.
Physical problems were the most common in our study, with fatigue being the most frequently reported. Longitudinal studies of HL survivors participating in clinical trials have shown that fatigue increases from the start of treatment to mid-way between the treatment cycle, declines during the first 1.5–2 years post-treatment, and stabilizes (but remains present) as many as 10 years post-treatment [18, 19]. Our results from three independent survivor cohorts treated outside of a clinical trial are consistent with this observation, with patients treated in a usual-care environment being much more likely to report fatigue than longer-term survivors. Fatigue has been associated with age at diagnosis, and presence of comorbidities in earlier studies [19, 34]; we did not observe any such association in our investigation. However, we did note an association between fatigue and depression, which has been reported previously [34]. Specifically, depression was reported on the PL in 25% of cases where fatigue was reported. Other psychological symptoms like nervousness, sadness, fear, and loss of interest in usual activities were also commonly reported concurrently with fatigue. These results are consistent with other studies that show that emotional functioning in HL survivors improves over time as fatigue decreases [19]. Our observations support the notion that fatigue is part of a symptom cluster associated with mental health and suggest that distress related to fatigue can be monitored in HL using the NCCN DT. Again, utilizing the DT and its PL as a screening tool for unmet psychosocial needs appears to be an effective way to identify these issues. As above, interventions testing integrated, specialist palliative care as part of HL treatment, and survivorship could mitigate these bothersome patient experience issues significantly; to date, several randomized trials of specialist palliative care demonstrate improvements in mood, and even reductions in post-traumatic stress after treatment [35].
A few limitations are inherent in this study, given its retrospective design. The number of visits and time between visits were determined according to the medical needs of each patient, and not per-protocol. Thus, we were not able to follow each patient longitudinally from diagnosis through extended survivorship, and instead constructed our analyses based on independent groups of patients who were on therapy at the time of our study and those who had survived longer periods. Thus, we cannot exclude secular trends in HL management from the list of potential explanatory factors for the differences in distress profiles we observed among the groups in our study. These secular trends primarily involved changes in patterns of radiation and/or chemotherapy regimens, such as the rise in use of adaptive therapy, wherein number of treatment cycles is dependent on how soon a patient’s PET scan results show a complete remission [36]. We did observe differences in actionable distress comparing patients recently treated with radiation vs. chemo/radiotherapy, although the results were derived from a small number of participants receiving radiation and it is not possible to tell whether this is consistent with any secular trend.
We also note that we did not validate DT findings against other measures such as the Hospital Anxiety and Depression Scale, as has been done previously [23]. Thus, we cannot exclude the possibility that that the NCCN DT lacks specificity in the long-term survival setting. We were also unable to recover DT from approximately 30% of clinical encounters, and reasons for missing DT are not recorded in the EMR. However, the missing rate was similar across the survivor cohorts, and only one participant had entirely absent DT data. Nonetheless, we acknowledge the possibility that failure to complete a DT may be associated with extreme distress. Thus, the overall distress burden reflected in our study may underestimate the true value. In addition, while we found scant evidence in the EMR of referral to psychosocial counseling services based on DT screening, we cannot be sure the real extent of service utilization in our cohort and whether it was effective. Further research is needed to determine whether intervention can successfully ameliorate distress during the treatment period.
Finally, our estimation of distress in patients on treatment reflects only the average experience of patients who are recently treated, rather than distress exactly coinciding with treatment visits. Nonetheless, our results are not dissimilar to the aforementioned Dutch study of lymphoma patients whose distress level was measured concurrently with milestones during treatment [28]. Thus, our study suggests that the NCCN DT has face validity for screening actively treated HL patients for distress, and calls for more attention to distress in HL patients undergoing active treatment and beyond.
Our study provides unique insight into the psychological experience of patients undergoing treatment for HL outside of a clinical trial and suggests that the NCCN DT is a feasible screening tool for identifying excessive psychological and symptom distress in these patients. Of particular importance is our observation that distress is measurable in HL across the continuum of survivorship and generally remains at low levels. However, actionable distress is reported at a substantial proportion of clinical encounters among all survivors, and possibly more frequently among patients on treatment. This finding adds to the literature, as most studies of patient-reported quality of life in HL, including symptom distress, have focused primarily on the post-treatment survivorship period, and less so on patients’ experiences during active therapy [37]. It also runs counter to the common assumption that patients will largely do well and feel well, after a year or two post-completion of chemotherapy, when cured of their disease. Our data points to persistent unmet needs in even the longer-term survivorship cohort, regarding distressing symptoms and emotional issues. Further attention to these issues is needed. In addition, our observations provide a rarely-seen insight into the real-world care environment, making the results immediately relevant to clinicians who are managing HL survivors. Our observations that actionable distress is largely unrelated to disease-related factors also highlight the potential importance of the healthcare system itself as an antagonist. The severity and etiology of distress occurring between visits are unknown and warrant further study. More, real-time data collection concerning distress and triggers of distress outside the setting of clinical care would be necessary to test this hypothesis. Finally, our findings support testing the efficacy of interventions to reduce distress in HL, and to monitor and compare distress levels during periods of survivorship when patients are not attending the clinic.
References
SEER Cancer Statistics Review (1975-2014) National Cancer Institute, Bethesda, MD
Ng AK (2014) Current survivorship recommendations for patients with Hodgkin lymphoma: focus on late effects. Blood 124(23):3373–3379. https://doi.org/10.1182/blood-2014-05-579193
Brown KW, Levy AR, Rosberger Z, Edgar L (2003) Psychological distress and cancer survival: a follow-up 10 years after diagnosis. Psychosom Med 65(4):636–643
Holland JC (2017) NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Distress Management Version 2.2017. National Comprehensive Cancer Network, Inc. https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. Accessed 8 Sept 2017
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psycho-Oncology 10(1):19–28
Ganz PA, Moinpour CM, Pauler DK, Kornblith AB, Gaynor ER, Balcerzak SP, Gatti GS, Erba HP, McCoy S, Press OW, Fisher RI (2003) Health status and quality of life in patients with early-stage Hodgkin’s disease treated on southwest oncology group study 9133. J Clin Oncol 21(18):3512–3519. https://doi.org/10.1200/JCO.2003.01.044
Engert A, Plutschow A, Eich HT, Lohri A, Dorken B, Borchmann P, Berger B, Greil R, Willborn KC, Wilhelm M, Debus J, Eble MJ, Sokler M, Ho A, Rank A, Ganser A, Trumper L, Bokemeyer C, Kirchner H, Schubert J, Kral Z, Fuchs M, Muller-Hermelink HK, Muller RP, Diehl V (2010) Reduced treatment intensity in patients with early-stage Hodgkin’s lymphoma. N Engl J Med 363(7):640–652. https://doi.org/10.1056/NEJMoa1000067
Meyer RM, Gospodarowicz MK, Connors JM, Pearcey RG, Wells WA, Winter JN, Horning SJ, Dar AR, Shustik C, Stewart DA, Crump M, Djurfeldt MS, Chen BE, Shepherd LE, Group NCT, Eastern Cooperative Oncology G (2012) ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med 366(5):399–408. https://doi.org/10.1056/NEJMoa1111961
Diehl V, Franklin J, Hasenclever D, Tesch H, Pfreundschuh M, Lathan B, Paulus U, Sieber M, Ruffer JU, Sextro M, Engert A, Wolf J, Hermann R, Holmer L, Stappert-Jahn U, Winnerlein-Trump E, Wulf G, Krause S, Glunz A, von Kalle K, Bischoff H, Haedicke C, Duhmke E, Georgii A, Loeffler M (1998) BEACOPP: a new regimen for advanced Hodgkin’s disease. German Hodgkin’s Lymphoma Study. Group Ann Oncol 9(Suppl 5):S67–S71
Gordon LI, Hong F, Fisher RI, Bartlett NL, Connors JM, Gascoyne RD, Wagner H, Stiff PJ, Cheson BD, Gospodarowicz M, Advani R, Kahl BS, Friedberg JW, Blum KA, Habermann TM, Tuscano JM, Hoppe RT, Horning SJ (2013) Randomized phase III trial of ABVD versus Stanford V with or without radiation therapy in locally extensive and advanced-stage Hodgkin lymphoma: an intergroup study coordinated by the eastern cooperative oncology group (E2496). J Clin Oncol 31(6):684–691. https://doi.org/10.1200/JCO.2012.43.4803
Younes A, Gopal AK, Smith SE, Ansell SM, Rosenblatt JD, Savage KJ, Ramchandren R, Bartlett NL, Cheson BD, de Vos S, Forero-Torres A, Moskowitz CH, Connors JM, Engert A, Larsen EK, Kennedy DA, Sievers EL, Chen R (2012) Results of a pivotal phase II study of brentuximab vedotin for patients with relapsed or refractory Hodgkin’s lymphoma. J Clin Oncol 30(18):2183–2189. https://doi.org/10.1200/JCO.2011.38.0410
Younes A, Connors JM, Park SI, Fanale M, O'Meara MM, Hunder NN, Huebner D, Ansell SM (2013) Brentuximab vedotin combined with ABVD or AVD for patients with newly diagnosed Hodgkin’s lymphoma: a phase 1, open-label, dose-escalation study. Lancet Oncol 14(13):1348–1356. https://doi.org/10.1016/S1470-2045(13)70501-1
Singh H, Kanapuru B, Smith C, Fashoyin-Aje LA, Myers A, Kim G, Pazdur R (2017) FDA analysis of enrollment of older adults in clinical trials for cancer drug registration: a 10-year experience by the U.S. Food and Drug Administration. J Clin Oncol 35(suppl; abstr 10009):10009
Fang CK, Chang MC, Chen PJ, Lin CC, Chen GS, Lin J, Hsieh RK, Chang YF, Chen HW, Wu CL, Lin KC, Chiu YJ, Li YC (2014) A correlational study of suicidal ideation with psychological distress, depression, and demoralization in patients with cancer. Support Care Cancer 22(12):3165–3174. https://doi.org/10.1007/s00520-014-2290-4
Hurria A, Li D, Hansen K, Patil S, Gupta R, Nelson C, Lichtman SM, Tew WP, Hamlin P, Zuckerman E, Gardes J, Limaye S, Lachs M, Kelly E (2009) Distress in older patients with cancer. J Clin Oncol 27(26):4346–4351. https://doi.org/10.1200/jco.2008.19.9463
Wang Y, Zou L, Jiang M, Wei Y, Jiang Y (2013) Measurement of distress in Chinese inpatients with lymphoma. Psycho-Oncology 22(7):1581–1586. https://doi.org/10.1002/pon.3170
Ransom S, Jacobsen PB, Booth-Jones M (2006) Validation of the distress thermometer with bone marrow transplant patients. Psycho-Oncology 15(7):604–612. https://doi.org/10.1002/pon.993
Kreissl S, Mueller H, Goergen H, Mayer A, Brillant C, Behringer K, Halbsguth TV, Hitz F, Soekler M, Shonukan O, Rueffer JU, Flechtner HH, Fuchs M, Diehl V, Engert A, Borchmann P (2016) Cancer-related fatigue in patients with and survivors of Hodgkin’s lymphoma: a longitudinal study of the German Hodgkin study group. Lancet Oncol 17:1453–1462. https://doi.org/10.1016/s1470-2045(16)30093-6
Heutte N, Flechtner HH, Mounier N, Mellink WA, Meerwaldt JH, Eghbali H, van’t Veer MB, Noordijk EM, Kluin-Nelemans JC, Lampka E, Thomas J, Lugtenburg PJ, Viterbo L, Carde P, Hagenbeek A, van der Maazen RW, Smit WG, Brice P, van Marwijk Kooy M, Baars JW, Poortmans P, Tirelli U, Leeksma OC, Tomsic R, Feugier P, Salles G, Gabarre J, Kersten MJ, Van Den Neste E, Creemers GJ, Gaillard I, Meijnders P, Tertian G, Reman O, Muller HP, Troncy J, Blanc M, Schroyens W, Voogt PJ, Wijermans P, Rieux C, Ferme C, Henry-Amar M, Group E-GHT (2009) Quality of life after successful treatment of early-stage Hodgkin's lymphoma: 10-year follow-up of the EORTC-GELA H8 randomised controlled trial. Lancet Oncol 10(12):1160–1170. https://doi.org/10.1016/S1470-2045(09)70258-X
Nekhlyudov L, Ganz PA, Arora NK, Rowland JH (2017) Going beyond being lost in transition: a decade of progress in cancer survivorship. J Clin Oncol 35(18):1978–1981. https://doi.org/10.1200/JCO.2016.72.1373
Holland JC, Andersen B, Breitbart WS, Buchmann LO, Compas B, Deshields TL, Dudley MM, Fleishman S, Fulcher CD, Greenberg DB, Greiner CB, Handzo GF, Hoofring L, Hoover C, Jacobsen PB, Kvale E, Levy MH, Loscalzo MJ, McAllister-Black R, Mechanic KY, Palesh O, Pazar JP, Riba MB, Roper K, Valentine AD, Wagner LI, Zevon MA, McMillian NR, Freedman-Cass DA (2013) Distress management. J Natl Compr Cancer Netw 11(2):190–209
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Ma X, Zhang J, Zhong W, Shu C, Wang F, Wen J, Zhou M, Sang Y, Jiang Y, Liu L (2014) The diagnostic role of a short screening tool—the distress thermometer: a meta-analysis. Support Care Cancer 22(7):1741–1755. https://doi.org/10.1007/s00520-014-2143-1
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, Lister TA (2014) Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol 32(27):3059–3068. https://doi.org/10.1200/jco.2013.54.8800
Atherton PJ, Burger KN, Pederson LD, Kaggal S, Sloan JA (2016) Patient-reported outcomes questionnaire compliance in Cancer Cooperative Group Trials (Alliance N0992). Clin Trials 13(6):612–620. https://doi.org/10.1177/1740774516655101
Friedlander M, Mercieca-Bebber RL, King MT (2016) Patient-reported outcomes (PRO) in ovarian cancer clinical trials-lost opportunities and lessons learned. Ann Oncol 27(Suppl 1):i66–i71. https://doi.org/10.1093/annonc/mdw080
Bauwens S, Baillon C, Distelmans W, Theuns P (2009) The ‘Distress Barometer’: validation of method of combining the distress thermometer with a rated complaint scale. Psycho-Oncology 18(5):534–542. https://doi.org/10.1002/pon.1425
Vermaete N, Wolter P, Verhoef G, Gosselink R (2014) Physical activity and physical fitness in lymphoma patients before, during, and after chemotherapy: a prospective longitudinal study. Ann Hematol 93(3):411–424. https://doi.org/10.1007/s00277-013-1881-3
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742. https://doi.org/10.1056/NEJMoa1000678
Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I, Donner A, Lo C (2014) Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 383(9930):1721–1730. https://doi.org/10.1016/S0140-6736(13)62416-2
Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, Hull JG, Li Z, Tosteson TD, Byock IR, Ahles TA (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the project ENABLE II randomized controlled trial. JAMA 302(7):741–749. https://doi.org/10.1001/jama.2009.1198
Bakitas MA, Tosteson TD, Li Z, Lyons KD, Hull JG, Li Z, Dionne-Odom JN, Frost J, Dragnev KH, Hegel MT, Azuero A, Ahles TA (2015) Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol 33(13):1438–1445. https://doi.org/10.1200/JCO.2014.58.6362
El-Jawahri A, LeBlanc T, VanDusen H, Traeger L, Greer JA, Pirl WF, Jackson VA, Telles J, Rhodes A, Spitzer TR, McAfee S, Chen YA, Lee SS, Temel JS (2016) Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: a randomized clinical trial. JAMA 316(20):2094–2103. https://doi.org/10.1001/jama.2016.16786
Daniels LA, Oerlemans S, Krol AD, Creutzberg CL, van de Poll-Franse LV (2014) Chronic fatigue in Hodgkin lymphoma survivors and associations with anxiety, depression and comorbidity. Br J Cancer 110(4):868–874. https://doi.org/10.1038/bjc.2013.779
El-Jawahri A, Traeger L, Greer JA, VanDusen H, Fishman SR, LeBlanc TW, Pirl WF, Jackson VA, Telles J, Rhodes A, Li Z, Spitzer TR, McAfee S, Chen YA, Temel JS (2017) Effect of inpatient palliative care during hematopoietic stem-cell transplant on psychological distress 6 months after transplant: results of a randomized clinical trial. J Clin Oncol 35(32):3714–3721. https://doi.org/10.1200/JCO.2017.73.2800
Canellos GP, Rosenberg SA, Friedberg JW, Lister TA, Devita VT (2014) Treatment of Hodgkin lymphoma: a 50-year perspective. J Clin Oncol 32(3):163–168. https://doi.org/10.1200/JCO.2013.53.1194
Linendoll N, Saunders T, Burns R, Nyce JD, Wendell KB, Evens AM, Parsons SK (2016) Health-related quality of life in Hodgkin lymphoma: a systematic review. Health Qual Life Outcomes 14(1):114. https://doi.org/10.1186/s12955-016-0515-6
Funding
This research was funded in part by a grant from Seattle Genetics, Inc., Seattle, WA, to Duke University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Jesse Troy reports honoraria from GamidaCell, consulting fees from The EMMES Corporation, AegisCN, and The Community Data Roundtable; Thomas LeBlanc reports consulting fees from Amgen, Agios, AbbVie, CareVive, Celgene, Pfizer, Helsinn, Flatiron Health, Medtronic, Otsuka, Welvie, and Heron, grants from American Cancer Society, AstraZeneca, and Cambia Health Solutions. Jose Feliciano and Akshara Richhariya report equity ownership and employment at Seattle Genetics. Susan Locke and Greg Samsa have no disclosures to report.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Troy, J.D., Locke, S.C., Samsa, G.P. et al. Patient-reported distress in Hodgkin lymphoma across the survivorship continuum. Support Care Cancer 27, 2453–2462 (2019). https://doi.org/10.1007/s00520-018-4523-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4523-4