Abstract
Purpose
To describe the perceptions of haematological cancer patients about the components of care deemed essential to supporting them to obtain and understand information about their cancer, its treatment and its impact on their life.
Methods
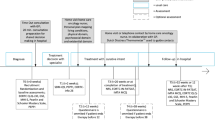
A cross-sectional survey was conducted with individuals diagnosed with haematological cancer. Eligible patients presenting for a scheduled outpatient appointment were invited to complete a pen-and-paper survey in the clinic waiting room while waiting for their appointment. Those who completed the survey were mailed a second survey approximately 4 weeks later. Participants provided data about their demographic and disease characteristics and perceptions of optimal care for haematological cancer patients.
Results
A total of 170 patients completed both surveys and were included in the analysis. The items endorsed as essential components of care by the highest number of participants were being able to share accurate information about their disease, treatment and ongoing care with their GP/family doctor (49%); being able to obtain up-to-date information specific to their circumstances (43%); being able to obtain information in the amount of detail that they want (34%); being able to call a health care professional at the treatment centre where they are receiving care (34%) and being able to call an experienced health care professional who has knowledge of their disease and its treatment (34%).
Conclusions
Further research is needed to determine ways of meeting the preferences of haematological cancer patients and determining the associated impact on patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Haematological cancers impose a significant burden
Haematological cancers originate in blood-forming tissue, such as the bone marrow or in the cells of the immune system [30]. Haematological cancers account for approximately 9% of all cancers and in economically developed areas of the world, are the fourth most frequently diagnosed cancer in both men and women [36]. Haematological cancers have a significant impact on both overall quality of life and health-related quality of life [1]. Individuals with haematological cancers report debilitating side effects as a result of both the cancer and its treatment. These side effects include lack of energy, pain, shortness of breath, nausea and dizziness [25]. Rates of clinical distress among individuals with haematological cancers are high, with studies estimating that individuals with a haematological cancer experience depression (16.9%) and anxiety (22.8%) [23]. Given this significant psychological and physical impact, it is critical that efforts are made to reduce the negative impact of haematological cancers.
The quality of communication and information provision influences patient outcomes
The provision of accurate information to patients about their cancer in a format they can understand is universally acknowledged as a core component of best-practice cancer care [3, 20]. Effective communication and information provision throughout the cancer journey is associated with a myriad of benefits, including lower rates of depression and anxiety [10, 18], increased patient involvement in decision making [10], greater satisfaction with treatment choices [10], greater overall satisfaction with care [18] and better quality of life [2, 18]. In contrast, poor communication and the provision of inadequate information has been shown to lead to uncertainty [9, 12], anxiety and depression [5, 9], non-compliance [40] and difficulties in coping and adjusting to a diagnosis of cancer [11] [24]. The impacts of poor communication can be profound, with a recent study showing that more than half of patients with advanced cancer incorrectly believed that their treatment was curative and that their condition would improve within a year [38].
What are the information needs of haematological cancer patients?
Despite increasing knowledge of the influence of communication and information provision on patient outcomes, there is consistent evidence that the provision of information to cancer patients is often sub-optimal. For example, a recent systematic review of 112 studies examining the information needs of cancer patients found that 96% of included studies identified some information needs related to treatment information, 65% identified information needs related to cancer-specific information and 63% identified information needs related to rehabilitation information [10]. A cross-sectional survey examining the information needs of haematological cancer patients found that needs for information were moderate to high, with 40–70% of participants identifying some unmet information needs. Individuals who were younger and had co-morbidities and lower quality of life were more likely to have higher needs for information [35]. Another systematic review which examined the specific information needs of haematological cancer patients concluded that patients wanted information about the disease (diagnosis and diagnostics), its treatment, prognosis and other topics including self-care and psychosocial functioning [34]. While a significant amount of research effort has been devoted to understanding and describing the information needs of cancer patients, comparatively less has been devoted to understanding what ‘optimal’ cancer care looks like and the practical strategies that could assist cancer patients to understand their disease. To our knowledge, no research has examined haematological cancer patient perceptions of the components they consider to be essential parts of optimal cancer care. This critical information would provide healthcare providers and policy makers with valuable information about how services and care can better be structured to meet the information needs of a highly vulnerable group of patients.
Aims
To describe the perceptions of haematological cancer patients about the components of care deemed essential to supporting them to obtain and understand information about their cancer, its treatment and its impact on their life.
Methods
Design and setting
A cross-sectional survey of outpatients was conducted in three metropolitan hospitals located across three Australian states. Participants were recruited from haematological cancer outpatient clinics treating a minimum of 300 patients per year for haematological cancer. Ethics approval was provided by the University of Newcastle Human Research Ethics Committee and site approvals were obtained from participating hospitals.
Participants
People with a diagnosis of any haematological cancer, who were aged 18 years or older and presenting for a scheduled outpatient appointment at a participating cancer clinic were eligible to participate. Patients who were not adequately proficient in English to complete the survey, had not previously attended an appointment at the clinic or judged by clinic staff as unable to provide informed consent were excluded.
Recruitment
Patients were approached and invited to participate in the study by a trained research assistant in the clinic waiting room. Clinical hospital staff assisted the research assistant to identify potentially eligible patients from the daily clinic appointment list. The research assistant provided eligible patients with a verbal overview of the study and a written information statement. Patients who indicated an interest in participating were asked to sign a consent form. Age and gender of non-consenters were recorded by the research assistant on a study log sheet to allow for possible consent bias to be examined.
Data collection
Participation in the study involved completion of two pen-and-paper surveys. Participants were invited to complete the first survey at the time of consent while waiting for their appointment, or could take it home and post it back to the research team within 1 week. The first survey obtained self-report information about participants’ socio-demographic characteristics, their haematological cancer diagnosis and its treatment. The follow-up survey was mailed to participants approximately 4 weeks later. This second survey included questions about chemotherapy side-effects, experiences obtaining cancer and treatment-related information (findings reported elsewhere) and views regarding optimal care for haematological cancer patients. Participants were asked to complete the survey and return it to the research team using a provided reply-paid envelope. Reminders, including a letter and another copy of the survey, were sent to participants who did not return their completed survey approximately 3 and 6 weeks after the initial mailing.
Measures
Demographic and disease characteristics
Participants were asked to provide information about their gender, date of birth, country of birth, Aboriginal or Torres Strait Islander status, marital and employment status, whether they hold a concession card, haematological cancer diagnosis, stage of disease and time since diagnosis.
Perceptions of optimal care for haematological cancer patients
Participants were presented with a list of 14 statements describing aspects of care related to the provision of information and support (e.g. “Having a record of what is discussed in each consultation”- see Table 2 for all items). Participants were asked to indicate their views about the importance of each statement in achieving optimal care for cancer patients. Responses were recorded on a 4-point Likert scale (1 = not important to 4 = essential). Several items were adapted from clinical practice guidelines for the psychosocial care of cancer patients [29]. Additional items were purposely developed in consultation with haematological cancer specialist clinicians to explore the types of information and support strategies that patients perceive would be most important in improving cancer care.
Statistical analysis
Characteristics of participants and non-consenters were compared using F-adjusted Rao-Scott chi-square tests, adjusted for treatment centre. Frequencies and percentages were calculated for each item surveying the participants’ perception of optimal care. Responses were regrouped as Not important, Somewhat or quite important, or Essential. Statistical analyses were programmed using SAS v9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Sample
Of the 349 patients identified as eligible to participate, 84% (n = 292) provided consent.
Of those who consented, 81% (n = 236) completed the first survey and 58% (n = 170) also completed and returned the second survey. There was no indication of consent bias between participants and non-consenters for age (p = 0.14) or gender (p = 0.31). Data is presented for participants who completed both surveys only (n = 170).
Demographic characteristics
Participant demographic characteristics are presented in Table 1. The majority of the sample was older than 50 years (81%), and more than half of participants were male (58%), married or had a partner (67%) and were not currently employed (56%). Thirty-three percent of the sample had early stage cancer, 22% had advanced cancer, 18% were in remission and 27% did not know their cancer stage. The most common haematological cancer diagnoses were Non-Hodgkin lymphoma (30%), myeloma (16%) and chronic lymphocytic leukaemia (13%).
Perceptions of optimal care
Participant perceptions of optimal care are provided in Table 2. Almost half of the sample (49%) thought it was essential to be able to share accurate information about their disease, treatment and ongoing care with their general practitioner (GP)/family doctor and obtain up-to-date information specific to their circumstances (43%). One third of the participants (34%) thought that it was essential that they were able to obtain information in the amount of detail that they want, call a health care professional at the treatment centre where they are receiving care and call an experienced health care professional who has knowledge of their disease and its treatment. There was high agreement about the importance of all items, with more than two thirds of the sample agreeing that each item was either ‘somewhat or quite important’ or ‘essential’. Only 10% of participants thought that being able to connect with others going through similar experiences was essential, with 27% of participants rating this as not important.
Discussion
This cross-sectional study examined the perceptions of haematological cancer patients about strategies that would assist them to obtain and understand information about their cancer, its treatment and its impact on their life. Overall, all of the statements presented were rated as important components of optimal cancer care by a majority of participants.
The item with the highest overall endorsement was sharing of accurate information with the participant’s general practitioner or family doctor. This finding aligns with previous research [21, 22] and highlights the crucial role that patients perceive their general practitioner plays in their cancer care. There are a number of benefits to GP involvement in haematological cancer care, including often having a long-standing relationship with the patient, a more holistic knowledge of the cancer diagnosis in the context of the patient’s life and overall health and more time and training to recognise and respond to psychosocial needs [6, 31]. Despite this, inadequate sharing of information has been reported by both general practitioners and patients as an issue, with some GPs voicing concerns about their patients ‘disappearing into the hospital’ when specialist haematological care is provided [28]. This is particularly the case when patients from rural or remote areas have to seek treatment in larger metropolitan treatment centres. Collaborative systems of care that involve the cancer specialists and the GP working together with the patient and their family are widely agreed as the optimal model of care [7, 27]. There is also strong evidence that GPs support this model and are committed to being involved in information giving, providing independent clinical advice and encouraging patient advocacy [28]. Patient-held records have been proposed as one strategy to facilitate information exchange and communication between providers; however, a systematic review of 13 studies determined that they did not improve communication, patient health or satisfaction with care, primarily because of a low rate of uptake by healthcare professionals [15]. It is critical that work continues to develop systems and processes that facilitate the efficient sharing of accurate information between haematological cancer specialists and GPs. A recent review identified no randomised controlled trials or literature reviews have been undertaken specifically examining models of survivorship care for haematological cancer patients [39].
Being able to obtain up-to-date information specific to their circumstances was also deemed essential by a high proportion (43%) of participants. While the majority of cancer patients obtain most information about their cancer directly from their healthcare providers [8, 33], a high proportion also obtain information from the Internet [26, 33]. For example, one study of haematological cancer patients found that 52% had accessed the Internet in the past 12 months to obtain information about their cancer [33] with a further 22% of participants requesting others access online health information on their behalf [33]. While the proliferation of information on the Internet and its accessibility, means that sourcing information about cancer has never been easier [32]; haematological cancer patients frequently report problems identifying credible information that is specific to their circumstances. The development of tailored, web-based information programs to support haematological cancer patients may offer a solution to the difficulties of navigating the plethora of information on the Internet [37]. Such programs may be particularly valuable for outpatients who have less frequent contact with their health care providers.
Ease of contact with health professionals was also highly endorsed by participants. Overall, 34% of participants rated being able to call a health professional at the treatment centre where the patient was receiving care and being able to call an experienced health professional with knowledge of the individuals’ disease and its treatment, as essential elements of care. While many not-for-profit cancer charities in Australia and internationally provide telephone help lines to put cancer patients in contact with nurses and other allied health professionals, these are underutilised [4, 14]. These findings suggest that patients may prefer to talk to someone from the healthcare service where they are receiving treatment, or with knowledge of their particular circumstances. While it may not be feasible for specialist clinicians to be available to address the concerns of patients as they arise, the important role care navigators can play in meeting the information and support needs of patients, as has been demonstrated with other cancer types [13], deserves further exploration as a strategy to assist in information acquisition for haematological cancer patients, particularly in the early stages of the disease.
The least endorsed strategy was being able to connect by telephone, Internet or face-to-face with other people going through similar experiences, with only 10% of participants endorsing this as an essential component of care. This is an interesting finding given that previous research has found that haematological cancer patients indicate talking to others who are going through a similar experience as a frequent unmet need [16, 17]. While patients may desire the ability to connect with others going through a similar experience, it is possible they do not perceive it to be a critical aspect of care. Peer-support programs are based on the premise that connecting with, and receiving support from, another person who has been diagnosed with cancer and been through a similar experience can result in significant benefits [19]. Often, peer-support partners are matched according to the type of cancer to increase the relevance of the support that is provided. Peer-support programs delivered in various formats including telephone, face-to-face and via the Internet have been trialled, with mixed findings of effectiveness [19].
Limitations
The low rate of completion of both surveys relative to the number of persons invited to participate (48.7% completion rate) may have impacted the representativeness of the sample. Although we collected data from participants about time since diagnosis, whether participants were currently undergoing active treatment was not assessed. It is possible that the perceptions of the importance of strategies for those currently undergoing treatment may be different than those who are in remission and/or in the survivorship phase of their cancer journey.
Conclusions
More than one third of haematological cancer patients perceive that being able to share accurate information with their GP, being able to obtain up to date information specific to their circumstances in the amount of detail they want and being able to contact a healthcare professional at their treatment centre with knowledge of their disease and treatment are essential components of cancer care. Further research is needed to identify effective strategies for meeting these preferences and determine the associated impact on quality of care and cancer outcomes.
References
Allart-Vorelli P, Porro B, Baguet F, Michel A, Cousson-Gélie F (2015) Haematological cancer and quality of life: a systematic literature review. Blood Cancer J 5:e305
Arora NK (2003) Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med 57:791–806
Barnato AE, Llewellyn-Thomas HA, Peters EM, Siminoff L, Collins ED, Barry MJ (2007) Communication and decision making in cancer care: setting research priorities for decision support/patients’ decision aids. Med Decis Mak 27:626–634
Basch EM, Thaler HT, Shi W, Yakren S, Schrag D (2004) Use of information resources by patients with cancer and their companions. Cancer 100:2476–2483
Beekers N, Husson O, Mols F, van Eenbergen M, van de Poll-Franse LV (2015) Symptoms of anxiety and depression are associated with satisfaction with information provision and internet use among 3080 cancer survivors: results of the PROFILES Registry. Cancer Nurs 38:335–342
Brennan M, Jefford M (2009) General practitioner-based models of post-treatment follow up. Cancer Forum 33
Bulsara C, Ward AM, Joske D (2005) Patient perceptions of the GP role in cancer management. Aust Fam Physician 34:299
Carlsson ME (2009) Cancer patients seeking information from sources outside the health care system: change over a decade. Eur J Oncol Nurs 13:304–305
Ellis PM, Tattersall MHN (1999) How should doctors communicate the diagnosis of cancer to patients? Ann Med 31:336–341
Finney Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J (2005) Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns 57:250–261
Finset A, Smedstad LM, Øgar B (1997) Physician—patient interaction and coping with cancer: the doctor as informer or supporter? J Cancer Educ 12:174–178
Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR (1999) Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol 17:371–379
Gorin SS, Haggstrom D, Han PK, Fairfield KM, Krebs P, Clauser SB (2017) Cancer care coordination: a systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med:1–15
Grogan S, Yeoman G, Jefford M, Kirke B, Boyes A (2005) Australia’s cancer helpline: an audit of utility and caller profile. Aust Fam Physician 34:393
Gysels M, Richardson A, Higginson IJ (2007) Does the patient-held record improve continuity and related outcomes in cancer care: a systematic review. Health Expect 10:75–91
Hall A, Campbell HS, Sanson-Fisher R, Lynagh M, D'este C, Burkhalter R, Carey M (2013) Unmet needs of Australian and Canadian haematological cancer survivors: a cross-sectional international comparative study. Psycho-Oncology 22:2032–2038
Hall AE, Sanson-Fisher RW, Lynagh MC, Tzelepis F, D’Este C (2015) What do haematological cancer survivors want help with? A cross-sectional investigation of unmet supportive care needs. BMC Res Notes 8:221
Hawkins NA, Pollack LA, Leadbetter S, Steele WR, Carroll J, Dolan JG, Ryan EP, Ryan JL, Morrow GR (2008) Informational needs of patients and perceived adequacy of information available before and after treatment of cancer. J Psychosoc Oncol 26:1–16
Hoey LM, Ieropoli SC, White VM, Jefford M (2008) Systematic review of peer-support programs for people with cancer. Patient Educ Couns 70:315–337
Institute of Medicine, Committee on Quality of Health Care in America (2001) Crossing the quality chasm: a new health system for the 21st century. National Academies Press, Washington
Johansson B, Berglund G, Hoffman K, Glimelius B, Sjödén P-O (2000) The role of the general practitioner in cancer care and the effect of an extended information routine. Scand J Prim Health Care 18:143–148
Kendall M, Boyd K, Campbell C, Cormie P, Fife S, Thomas K, Weller D, Murray SA (2006) How do people with cancer wish to be cared for in primary care? Serial discussion groups of patients and carers. Fam Pract 23:644–650
Linden W, Vodermaier A, MacKenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 141:343–351
Mager WM, Andrykowski MA (2002) Communication in the cancer ‘bad news’ consultation: patient perceptions and psychological adjustment. Psycho-Oncology 11:35–46
Manitta V, Zordan R, Cole-Sinclair M, Nandurkar H, Philip J (2011) The symptom burden of patients with hematological malignancy: a cross-sectional observational study. J Pain Symptom Manag 42:432–442
Mattsson S, Olsson EMG, Johansson B, Carlsson M (2017) Health-related internet use in people with cancer: results from a cross-sectional study in two outpatient clinics in Sweden. J Med Internet Res 19:e163
McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, Hudson MM (2013) American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol 31:631–640
McGrath P (2007) Care of the haematology patient and their family- the GP viewpoint. Aust Fam Physician 36:779–781
National Breast Cancer Centre, National Cancer Control Initiative (2003) clinical practice guidelines for the psychosocial care of adults with cancer. In: editor (ed)^(eds) book clinical practice guidelines for the psychosocial care of adults with cancer. National Breast Cancer Centre, City
National Cancer Institute NCI Dictionary of Cancer Terms. In: Editor (ed)^(eds) Book NCI Dictionary of Cancer Terms, City
Nekhlyudov L (2009) “Doc, should I see you or my oncologist?” a primary care perspective on opportunities and challenges in providing comprehensive care for cancer survivors. J Clin Oncol 27:2424–2426
Rice RE (2006) Influences, usage, and outcomes of internet health information searching: multivariate results from the pew surveys. Int J Med Inform 75:8–28
Rider T, Malik M, Chevassut T (2014) Haematology patients and the internet—the use of on-line health information and the impact on the patient–doctor relationship. Patient Educ Couns 97:223–238
Rood JAJ, Eeltink CM, van Zuuren FJ, Verdonck-de Leeuw IM, Huijgens PC (2014) Perceived need for information of patients with haematological malignancies: a literature review. J Clin Nurs 24
Rood JAJ, van Zuuren FJ, Stam F, van der Ploeg T, Eeltink C, Verdonck-de Leeuw IM, Huijgens PC (2015) Perceived need for information among patients with a haematological malignancy: associations with information satisfaction and treatment decision-making preferences. Hematol Oncol 33:85–98
Smith A, Howell D, Patmore R, Jack A, Roman E (2011) Incidence of haematological malignancy by sub-type: a report from the haematological malignancy research network. Br J Cancer 105:1684–1692
Smits R, Bryant J, Sanson-Fisher R, Tzelepis F, Henskens F, Paul C, Stevenson W (2014) Tailored and integrated web-based tools for improving psychosocial outcomes of cancer patients: the DoTTI development framework. J Med Internet Res 16:e76
Soylu C, Babacan T, Sever AR, Altundag K (2016) Patients’ understanding of treatment goals and disease course and their relationship with optimism, hope, and quality of life: a preliminary study among advanced breast cancer outpatients before receiving palliative treatment. Support Care Cancer 24:3481–3488
Taylor K, Chan RJ, Monterosso L (2015) Models of survivorship care provision in adult patients with haematological cancer: an integrative literature review. Support Care Cancer 23:1447–1458
Zolnierek KBH, DiMatteo MR (2009) Physician communication and patient adherence to treatment: a meta-analysis. Med Care 47:826–834
Acknowledgements and funding
The development of the survey instrument was supported by the Cancer Institute New South Wales (10/THS/2-14). This research was funded by a Strategic Research Partnership grant provided by Cancer Council New South Wales to the Newcastle Cancer Control Collaborative (CSR11-02) and infrastructure funding from the Hunter Medical Research Institute (HMRI). Dr. Jamie Bryant was supported by an Australian Research Council Post-Doctoral Industry Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bryant, J., Smits, R., Turon, H. et al. Optimal cancer care: what essential elements of care would help haematological cancer patients obtain and understand information about their disease and its treatment and impact?. Support Care Cancer 26, 2843–2849 (2018). https://doi.org/10.1007/s00520-018-4140-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4140-2