Abstract
Purpose
Patients with advanced cancers frequently experience pain. Opioids are commonly prescribed to treat cancer-related pain, but their use might be associated with undesirable consequences including adverse effects and tumor progression, resulting in increased heath care utilization and shorter survival. We examined these possibilities in a large cohort of patients diagnosed with ten common advanced malignancies.
Methods
We identified 1386 newly diagnosed patients with stage IV non-hematologic malignancies from 2005 to 2013 and ascertained opioid utilization within 90 days of starting anti-cancer treatment using electronic medical record and tumor registry data. Opioid utilization was stratified into low opioid (LO; < 5 mg oral morphine equivalents (OME)/day) and high opioid (HO; ≥ 5 mg OME/day). Health care utilization included tallies of emergency room, urgent care, and inpatient visits. The association of opioid use, tumor type prognosis, age, and gender with overall survival was analyzed in univariate and multivariate models.
Results
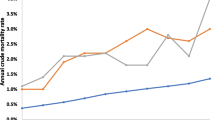
HO use patients (n = 624) had greater health care utilization compared to LO use patients (n = 762; p < 0.05). HO use patients also had shorter survival (median survival, 5.5 vs 12.4 months; p < 0.0001). On multivariate analysis, HO use remained associated with shorter overall survival (HR 1.4; 95% CI, 1.3–1.6; p < 0.0001) after adjusting for age, gender, and prognostic group.
Conclusions
In advanced cancer patients, HO use is associated with greater health care utilization and shorter survival. Prospective studies using opioid-sparing approaches are indicated, to confirm these retrospective findings and to evaluate if these undesirable effects associated with opioid use can be mitigated.

Similar content being viewed by others
References
Portenoy RK, Ahmed E (2014) Principles of opioid use in cancer pain. J Clin Oncol 32(16):1662–1670. https://doi.org/10.1200/JCO.2013.52.5188
World Health Organization (1996) Cancer pain relief: with a guide to opioid availability. World Health Organization
van den Beuken-van Everdingen MH et al (2007) Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 18(9):1437–1449. https://doi.org/10.1093/annonc/mdm056
Dalal S, Bruera E (2013) Access to opioid analgesics and pain relief for patients with cancer. Nat Rev Clin Oncol 10(2):108–116. https://doi.org/10.1038/nrclinonc.2012.237
Baldini A, Von Korff M, Lin EH (2012) A review of potential adverse effects of long-term opioid therapy: a practitioner’s guide. Prim Care Companion CNS Disord 14(3)
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, Glaser SE, Vallejo R (2008) Opioid complications and side effects. Pain Physician 11(2 Suppl):S105–S120
Kotajima F et al (2014) Lung cancer patients frequently visit the emergency room for cancer-related and -unrelated issues. Mol Clin Oncol 2(2):322–326. https://doi.org/10.3892/mco.2014.241
Rudd RA, Seth P, David F, Scholl L (2016) Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep 65(5051):1445–1452. https://doi.org/10.15585/mmwr.mm655051e1
Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL (2011) Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 12(4):657–667. https://doi.org/10.1111/j.1526-4637.2011.01075.x
Boland JW, Ziegler L, Boland EG, McDermid K, Bennett MI (2015) Is regular systemic opioid analgesia associated with shorter survival in adult patients with cancer? A systematic literature review. Pain 156(11):2152–2163. https://doi.org/10.1097/j.pain.0000000000000306
Sjogren P, Kaasa S (2016) The role of opioids in cancer progression: emerging experimental and clinical implications. Ann Oncol 27(11):1978–1980. https://doi.org/10.1093/annonc/mdw407
Zylla D, Gourley BL, Vang D, Jackson S, Boatman S, Lindgren B, Kuskowski MA, Le C, Gupta K, Gupta P (2013) Opioid requirement, opioid receptor expression, and clinical outcomes in patients with advanced prostate cancer. Cancer 119(23):4103–4110. https://doi.org/10.1002/cncr.28345
Zylla D, Kuskowski MA, Gupta K, Gupta P (2014) Association of opioid requirement and cancer pain with survival in advanced non-small cell lung cancer. Br J Anaesth 113(Suppl 1):i109–i116. https://doi.org/10.1093/bja/aeu351
Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S (2003) Clinical application of opioid equianalgesic data. Clin J Pain 19(5):286–297. https://doi.org/10.1097/00002508-200309000-00002
Kern DM, Zhou S, Chavoshi S, Tunceli O, Sostek M, Singer J, LoCasale RJ (2015) Treatment patterns, healthcare utilization, and costs of chronic opioid treatment for non-cancer pain in the United States. Am J Manag Care 21(3):e222–e234
Halabi S, Vogelzang NJ, Kornblith AB, Ou SS, Kantoff PW, Dawson NA, Small EJ (2008) Pain predicts overall survival in men with metastatic castration-refractory prostate cancer. J Clin Oncol 26(15):2544–2549. https://doi.org/10.1200/JCO.2007.15.0367
Farooqui M, Li Y, Rogers T, Poonawala T, Griffin RJ, Song CW, Gupta K (2007) COX-2 inhibitor celecoxib prevents chronic morphine-induced promotion of angiogenesis, tumour growth, metastasis and mortality, without compromising analgesia. Br J Cancer 97(11):1523–1531. https://doi.org/10.1038/sj.bjc.6604057
Gupta K, Kshirsagar S, Chang L, Schwartz R, Law PY, Yee D, Hebbel RP (2002) Morphine stimulates angiogenesis by activating proangiogenic and survival-promoting signaling and promotes breast tumor growth. Cancer Res 62(15):4491–4498
Mathew B, Lennon FE, Siegler J, Mirzapoiazova T, Mambetsariev N, Sammani S, Gerhold LM, LaRiviere PJ, Chen CT, Garcia JGN, Salgia R, Moss J, Singleton PA (2011) The novel role of the mu opioid receptor in lung cancer progression: a laboratory investigation. Anesth Analg 112(3):558–567. https://doi.org/10.1213/ANE.0b013e31820568af
Singleton PA, Mirzapoiazova T, Hasina R, Salgia R, Moss J (2014) Increased mu-opioid receptor expression in metastatic lung cancer. Br J Anaesth 113(Suppl 1):i103–i108. https://doi.org/10.1093/bja/aeu165
Bortsov AV, Millikan RC, Belfer I, Boortz-Marx RL, Arora H, McLean SA (2012) mu-Opioid receptor gene A118G polymorphism predicts survival in patients with breast cancer. Anesthesiology 116(4):896–902. https://doi.org/10.1097/ALN.0b013e31824b96a1
Singleton PA, Moss J, Karp DD, Atkins JT, Janku F (2015) The mu opioid receptor: a new target for cancer therapy? Cancer 121(16):2681–2688. https://doi.org/10.1002/cncr.29460
Janku F, Johnson LK, Karp DD, Atkins JT, Singleton PA, Moss J (2016) Treatment with methylnaltrexone is associated with increased survival in patients with advanced cancer. Ann Oncol 27(11):2032–2038. https://doi.org/10.1093/annonc/mdw317
Boehnke KF, Litinas E, Clauw DJ (2016) Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain 17(6):739–744. https://doi.org/10.1016/j.jpain.2016.03.002
Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Lichtman AH, Kornyeyeva E (2017) Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain 11(3):119–133. https://doi.org/10.1177/2049463717710042
Haroutounian S, Ratz Y, Ginosar Y, Furmanov K, Saifi F, Meidan R, Davidson E (2016) The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain 32(12):1036–1043. https://doi.org/10.1097/AJP.0000000000000364
Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT (2017) Results of a double-blind, randomized, placebo-controlled study of nabiximols oromucosal spray as adjunctive therapy in advanced cancer patients with chronic uncontrolled pain. J Pain Symptom Manag. https://doi.org/10.1016/j.jpainsymman.2017.09.001
Acknowledgments
The authors thank Arkadiusz Dudek, MD, PhD, and Jim Zacny for their critical review of this manuscript.
Funding
This study was supported by the Park Nicollet Foundation and HealthPartners Institute.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare that they have no conflict of interest.
Data control
We have full control of all primary data and agree to allow the journal to review this data if requested.
Ethical statement
All institutional guidelines for the proper conduction of clinical research were followed for this study.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Zylla, D., Steele, G., Shapiro, A. et al. Impact of opioid use on health care utilization and survival in patients with newly diagnosed stage IV malignancies. Support Care Cancer 26, 2259–2266 (2018). https://doi.org/10.1007/s00520-018-4062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4062-z