Abstract
Purpose
Sleep disturbance, fatigue and depression are common complaints in patients with cancer, and often contribute to worse quality of life (QoL). Circadian activity rhythms (CARs) are often disrupted in cancer patients. These symptoms worsen during treatment, but less is known about their long-term trajectory.
Methods
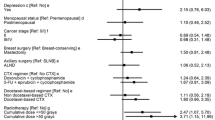
Sixty-eight women with stage I-III breast cancer (BC) scheduled to receive ≥4 cycles of chemotherapy, and age-, ethnicity-, and education-matched normal, cancer-free controls (NC) participated. Sleep was measured with actigraphy (nocturnal total sleep time [nocturnal TST] and daytime total nap time [NAPTIME]) and with the Pittsburgh Sleep Quality Index (PSQI); fatigue with the Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF); depression with the Center of Epidemiological Studies-Depression (CES-D). CARs were derived from actigraphy. Several measures of QoL were administered. Data were collected at three time points: before (baseline), end of cycle 4 (cycle 4), and 1 year post-chemotherapy (1 year).
Results
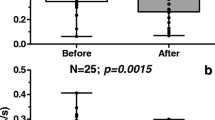
Compared to NC, BC had longer NAPTIME, worse sleep quality, more fatigue, more depressive symptoms, more disrupted CARs, and worse QoL at baseline (all p values <0.05). At cycle 4, BC showed worse sleep, increased fatigue, more depressive symptoms, and more disrupted CARs compared to their own baseline levels and to NC (all p values <0.05). By 1 year, BC’s fatigue, depressive symptoms, and QoL returned to baseline levels but were still worse than those of NC, while NAPTIME and CARs did not differ from NC’s.
Conclusion
Additional research is needed to determine if beginning treatment of these symptoms before the start of chemotherapy will minimize symptom severity over time.




Similar content being viewed by others
References
Fernandes R, Stone P, Andrews P, Morgan R, Sharma S (2006) Comparison between fatigue, sleep disturbance, and circadian rhythm in cancer inpatients and healthy volunteers: evaluation of diagnostic criteria for cancer-related fatigue. J Pain Symptom Manage 32:245–254
Esther Kim JE, Dodd MJ, Aouizerat BE, Jahan T, Miaskowski C (2009) A review of the prevalence and impact of multiple symptoms in oncology patients. J Pain Symptom Manage 37:715–736
Ancoli-Israel S, Liu L, Marler M, Parker BA, Jones V, Robins Sadler G, Dimsdale JE, Cohen-Zion M, Fiorentino L (2006) Fatigue, sleep and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer 14:201–209
Berger AM, Farr LA, Kuhn BR, Fischer P, Agrawal S (2007) Values of sleep/wake, activity/rest, circadian rhythms, and fatigue prior to adjuvant breast cancer chemotherapy. J Pain Symptom Manage 33:398–409
Miaskowski C, Lee K, Dunn L, Dodd M, Aouizerat BE, West C, Paul SM, Cooper B, Wara W, Swift P (2011) Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients before the initiation of radiation therapy. Cancer Nurs 34:255–268
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR (2000) Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol 18:743–753
Byar KL, Berger AM, Bakken SL, Cetak MA (2006) Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol Nurs Forum 33:E18–E26
Dodd MJ, Cho MH, Cooper BA, Miaskowski C (2010) The effect of symptom clusters on functional status and quality of life in women with breast cancer. Eur J Oncol Nurs 14:101–110
Sandadi S, Frasure HE, Broderick MJ, Waggoner SE, Miller JA, von Gruenigen VE (2011) The effect of sleep disturbance on quality of life in women with ovarian cancer. Gynecol Oncol 123:351–355
Fiorentino L, Ancoli-Israel S (2006) Insomnia and its treatment in women with breast cancer. Sleep Med Rev 10:419–429
Savard J, Simard S, Blanchet J, Ivers H, Morin CM (2001) Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep 24:583–590
Liu L, Marler M, Parker BA, Jones V, Johnson S, Cohen-Zion M, Fiorentino L, Sadler GR, Ancoli-Israel S (2005) The relationship between fatigue and light exposure during chemotherapy. Support Care Cancer 13:1010–1017
Liu L, Fiorentino L, Natarajan L, Parker BA, Mills PJ, Sadler GR, Dimsdale JE, Rissling M, He F, Ancoli-Israel S (2009) Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during chemotherapy. Psycho-oncology 18:187–194
Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR (2007) Cancer-related fatigue: the scale of the problem. Oncologist 12(1):4–10, 4-10
Berger AM, Gerber LH, Mayer DK (2012) Cancer-related fatigue: implications for breast cancer survivors. Cancer 118:2261–2269
Morrow GR, Andrews PLR, Hickok JT, Roscoe JA, Matteson S (2002) Fatigue associated with cancer and its treatment. Support Care Cancer 10:389–398
Trudel-Fitzgerald C, Savard J, Ivers H (2013) Which symptoms come first? Exploration of temporal relationships between cancer-related symptoms over an 18-month period. Ann Behav Med 45:329–337
So WK, Marsh G, Ling WM, Leung FY, Lo JC, Yeung M, Li GK (2009) The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum 36:E205–E214
Massie MJ (2004) Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 2004:57–71
Gehrman PR, Marler M, Martin JL, Shochat T, Corey-Bloom J, Ancoli-Israel S (2004) The timing of activity rhythms in patients with dementia is related to survival. Journal of Gerontology: Medical Sciences 59A:1050–1055
Paudel M, Taylor BC, Ancoli-Israel S, Blackwell T, Stone KL, Tranah G, Redline SS, Cummings SR, Ensrud KE, For the Osteoporotic Fractures in Men(MrOS) Study Group (2010) Rest/activity rhythms and mortality rates in older men: the MrOs sleep study. Chronobiol Int 27:363–377
Tranah GJ, Blackwell TL, Ancoli-Israel S, Paudel M, Ensrud K, Cauley JA, Hillier TA, Cummings SR, Stone KL, For the SOF Research Group (2010) Circadian activity rhythms and mortality: the study of osteoporotic fractures. J Am Geriatr Soc 58:282–291
Mormont MC, Waterhouse J, Bleuzen P, Giacchetti S, Jami A, Bogdan A, Touitou Y, Levi F (2000) Marked 24-h rest/activity rhythms are associated with better quality of life, better response and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res 6:3038–3045
Berger AM, Hertzog M, Geary CR, Fischer P, Farr L (2012) Circadian rhythms, symptoms, physical functioning, and body mass index in breast cancer survivors. J Cancer Surviv 6:305–314
Savard J, Liu L, Natajaran L, Rissling M, Neikrug AB, He F, Dimsdale JE, Mills PJ, Parker BA, Sadler GR, Ancoli-Israel S (2009) Breast cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep 32:1155–1160
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR (2000) Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol 18:743–753
Broeckel J, Jacobsen PB, Horton J, Balducci L, Lyman GH (1998) Characteristics and correlates of fatigue after adjuvant chemotherapy for breast cancer. Journal of Cinical Oncology 16:1689–1696
Pockaj BA, Degnim AC, Boughey JC, Gray RJ, McLaughlin SA, Dueck AC, Perez EA, Halyard MY, Frost MH, Cheville AL (2009) Quality of life after breast cancer surgery: what have we learned and where should we go next. J Surg Oncol 99:447–455
Trentham-Dietz A, Sprague BL, Klein R, Klein BE, Cruickshanks KJ, Fryback DG, Hampton JM (2008) Health-related quality of life before and after a breast cancer diagnosis. Breast Cancer Res Treat 109:379–387
Ancoli-Israel S, Cole R, Alessi CA, Chambers M, Moorcroft WH, Pollak C (2003) The role of actigraphy in the study of sleep and circadian rhythms. Sleep 26:342–392
Liu L, Rissling MB, Neikrug AB, Fiorentino L, Natarajan L, Faierman M, Sadler GR, Dimsdale JE, Mills PJ, Parker BA, Ancoli-Israel S (2013) Fatigue and circadian activity rhythms in breast cancer patients before and after chemotherapy: a controlled study. Fatigue: Biomedicine, Health & Behavior 1:12–26
Buysse DJ, Reynolds CRI, Monk TH, Hoch CC, Yeager AL, Kupfer DJ (1991) Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14(4):331–338
Buysse DJ, Reynolds CFI, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Stein KD, Martin SC, Hann DM, Jacobsen PB (1998) A multidimensional measure of fatigue for use with cancer patients. Cancer Pract 6:143–152
Stein KD, Jacobsen PB, Blanchard CM, Thors C (2004) Further validation of the multidimensional fatigue symptom inventory-short form. J Pain Symptom Manage 27:14–23
Radloff LS (1977) The CES-D scale: A self-report depression scale for research in the general population. Applied Psychol Measurement 1:385–401
Marler MR, Martin JL, Gehrman PR, Ancoli-Israel S (2006) The sigmoidally-transformed cosine curve: a mathematical model for circadian rhythms with symmetric non-sinusoidal shapes. Stat Med 25:3893–3904
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, Smith PL, Schwartz AR, Redline S, Pack AI, Dinges DF (1997) An instrument to measure functional status outcome for disorders of excessive sleepiness. Sleep 20:835–843
Ware JE, Kosinski M, Gandek B (2002) SF-36 Health survey: manual & interpretation guide. QualityMetric Incorporated, Lincoln, RI
Diggle PJ, Liang KY, Zeger SL (1994) Analysis of longitudinal data. Oxford University Press, New York, NY
Savard J, Morin CM (2001) Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol 19:895–908
Roscoe JA, Morrow GR, Hickok JT, Bushunow P, Matteson S, Rakita D, Andrews PLR (2002) Temporal interrelationships among fatigue, circadian rhythm and depression in breast cancer patients undergoing chemotherapy treatment. Support Care Cancer 10:329–336
Berger AM, Wielgus K, Hertzog M, Fischer P, Farr L (2009) Patterns of circadian activity rhythms and their relationships with fatigue and anxiety/depression in women treated with breast cancer adjuvant chemotherapy. Support Care Cancer 18(1):105–114
Acknowledgments
This study was supported by the National Cancer Institute (CA112035 and P30 CA023100), the UCSD Clinical and Translational Research Institute (UL1RR031980), and the Department of Veterans Affairs San Diego Center of Excellence for Stress and Mental Health (CESAMH). The authors would like to thank all women who participated in this study either as patients or controls. The study was funded by NIH
Conflict of interest
The corresponding author has full control of all primary data and agrees to allow the Journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ancoli-Israel, S., Liu, L., Rissling, M. et al. Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer 22, 2535–2545 (2014). https://doi.org/10.1007/s00520-014-2204-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2204-5