Summary
Background
Inflammatory bowel disease (IBD), a multisystemic inflammatory disorder, has been associated with increased risk of cardiovascular problems, including complications such as conduction defects and arrhythmias. Therefore, the early assessment of the risk factors predisposing to ventricular arrhythmias is crucial, since it can improve clinical outcomes. The objective of the present study is to evaluate ventricular repolarization by using Tp‑e interval and Tp-e/QTc ratio as candidate markers of ventricular arrhythmias in patients with IBD.
Methods
The presented study was designed as a single-center prospective cohort study. The study population consisted of 175 patients with IBD and 175 healthy volunteers. The Tp‑e interval, corrected QT (QTc), and Tp-e/QTc ratio were measured from the 12-lead electrocardiogram. These parameters were compared between groups.
Results
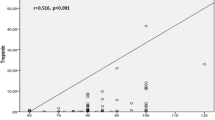
The groups were similar in terms of electrocardiographic findings such as heart rate, QRS interval, and QTc interval. However, Tp‑e interval (87.0 ms, interquartile range, IQR 81.0–105.0 ms vs. 84.0 ms, IQR 74.0–92.0 ms; p < 0.001) and Tp-e/QTc ratio (0.21 ± 0.04 vs. 0.19 ± 0.05; p < 0.001) were significantly increased in IBD patient group compared to control group. Notably, a positive correlation was demonstrated between Tp‑e interval, Tp-e/QTc ratio and disease duration (Spearman’s Rho = 0.36, p < 0.001 for Tp‑e; Spearman’s Rho = 0.28, p < 0.001 for Tp-e/QTc).
Conclusion
This study demonstrated that IBD patients are at increased risk of disrupted ventricular repolarization (increased Tpe, Tpe/QTc ratio). In addition, a positive correlation was demonstrated between Tp‑e interval, Tp-e/QTc ratio, and disease duration. Therefore, IBD patients, especially those with long-standing diseases, should be more closely screened for ventricular arrhythmias.




Similar content being viewed by others
References
Kaser A, Zeissig S, Blumberg RS. Inflammatory bowel disease. Annu Rev Immunol. 2010;28:573–621.
Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–34.
Vavricka SR, Schoepfer A, Scharl M, et al. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1982–92.
Bunu DM, Timofte CE, Ciocoiu M, et al. Cardiovascular manifestations of inflammatory bowel disease: pathogenesis, diagnosis, and preventive strategies. Gastroenterol Res Pract. 2019;2019:3012509.
Lewek J, Kaczmarek K, Cygankiewicz I, et al. Inflammation and arrhythmias: potential mechanisms and clinical implications. Expert Rev Cardiovasc Ther. 2014;12:1077–85.
Castro-Torres Y, Carmona-Puerta R, Katholi RE. Ventricular repolarization markers for predicting malignant arrhythmias in clinical practice. World J Clin Cases. 2015;3:705–20.
Acar G, Yorgun H, Inci MF, et al. Evaluation of Tp‑e interval and Tp-e/QT ratio in patients with ankylosing spondylitis. Mod Rheumatol. 2014;24:327–30.
Acar GR, Akkoyun M, Nacar AB, et al. Evaluation of Tp‑e interval and Tp-e/QT ratio in patients with rheumatoid arthritis. Turk Kardiyol Dern Ars. 2014;42:29–34.
Hidayet Ş, Demir V, Turan Y, et al. Evaluation of Tp‑e interval, Tp-e/QT ratio, and Tp-e/QTc ratio in patients with Behçet’s disease. Anatol J Cardiol. 2019;22:85–90.
Ott C, Schölmerich J. Extraintestinal manifestations and complications in IBD. Nat Rev Gastroenterol Hepatol. 2013;10:585–95.
Danese S, Semeraro S, Papa A, et al. Extraintestinal manifestations in inflammatory bowel disease. World J Gastroenterol. 2005;11:7227–36.
Harbord M, Annese V, Vavricka SR, et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohns Colitis. 2016;10:239–54.
Patel RS, Rohit Reddy S, Llukmani A, et al. Cardiovascular manifestations in inflammatory bowel disease: a systematic review of the pathogenesis and management of pericarditis. Cureus. 2021;13:e14010.
Greuter T, Rieder F, Kucharzik T, et al. Emerging treatment options for extraintestinal manifestations in IBD. Gut. 2021;70:796–802.
Nevulis MG, Baker C, Lebovics E, et al. Overview of link between inflammatory bowel disease and cardiovascular disease. Cardiol Rev. 2018;26:287–93.
Singh S, Singh H, Loftus EV, et al. Risk of cerebrovascular accidents and ischemic heart disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:382–93.
Karmiris K, Avgerinos A, Tavernaraki A, et al. Prevalence and characteristics of extra-intestinal manifestations in a large cohort of Greek patients with inflammatory bowel disease. J Crohns Colitis. 2016;10:429–36.
Mitchell NE, Harrison N, Junga Z, et al. Heart under attack: cardiac manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2018;24:2322–6.
Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Rungoe C, Nyboe Andersen N, Jess T. Inflammatory bowel disease and risk of coronary heart disease. Trends Cardiovasc Med. 2015;25:699–704.
Zanoli L, Rastelli S, Granata A, et al. Arterial stiffness in inflammatory bowel disease: a systematic review and meta-analysis. J Hypertens. 2016;34:822–9.
Neurath MF. Cytokines in inflammatory bowel disease. Nat Rev Immunol. 2014;14:329–42.
Tan VP, Chung A, Yan BP, Gibson PR. Venous and arterial disease in inflammatory bowel disease. J Gastroenterol Hepatol. 2013;28:1095–113.
Engel T, Ben-Horin S, Beer-Gabel M. Autonomic dysfunction correlates with clinical and inflammatory activity in patients with Crohn’s disease. Inflamm Bowel Dis. 2015;21:2320–6.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2017;2018(72):e91–e220.
Arteyeva NV. Dispersion of ventricular repolarization: Temporal and spatial. World J Cardiol. 2020;12:437–49.
Erikssen G, Liestøl K, Gullestad L, et al. The terminal part of the QT interval (T peak to T end): a predictor of mortality after acute myocardial infarction. Ann Noninvasive Electrocardiol. 2012;17:85–94.
Gupta P, Patel C, Patel H, et al. T(p-e)/QT ratio as an index of arrhythmogenesis. J Electrocardiol. 2008;41:567–74.
Zhao X, Xie Z, Chu Y, et al. Association between Tp-e/QT ratio and prognosis in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Clin Cardiol. 2012;35:559–64.
Candemir M, Candemir B, Ertürk A. Evaluation of cardiac autonomic nervous system in patients with ankylosing spondylitis using 12-lead electrocardiography and Holter monitoring. Clin Rheumatol. 2020;39:2631–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
İ. E. Güven, M. Candemir, B. Başpınar, R. E. Cankurtaran, and E. Kayaçetin declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Güven, İ.E., Candemir, M., Başpınar, B. et al. Evaluation of Tp-e interval and Tp-e/QTc ratio in patients with inflammatory bowel disease. Wien Klin Wochenschr 135, 14–21 (2023). https://doi.org/10.1007/s00508-022-02100-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-022-02100-4