Summary
Survival in cancer is continuously improving due to evolving oncological treatment. Therefore, cardiovascular short-term and long-term side effects gain crucial importance for overall outcome. Cardiotoxicity not only presents as heart failure, but also as treatment-resistant hypertension, acute coronary ischemia with plaque rupture or vasospasm, thromboembolism, arrhythmia, pulmonary hypertension, diastolic dysfunction, acute myocarditis and others. Recent recommendations have proposed baseline cardiac risk assessment and surveillance strategies. Major challenges are the availability of monitoring and imaging resources, including echocardiography with speckle tracking longitudinal strain (GLS), serum biomarkers such as natriuretic peptides (NT-proBNP) and highly sensitive cardiac troponins. This Austrian consensus encompasses cardiotoxicity occurrence in frequent antiproliferative cancer drugs, radiotherapy, immune checkpoint inhibitors and cardiac follow-up considerations in cancer survivors in the context of the Austrian healthcare setting. It is important to optimize cardiovascular risk factors and pre-existing cardiac diseases without delaying oncological treatment. If left ventricular ejection fraction (LVEF) deteriorates during cancer treatment (from >10% to <50%), or myocardial strain decreases (>15% change in GLS), early initiation of cardioprotective therapies (angiotensin-converting enzyme inhibitors, angiotensin or beta receptor blockers) is recommended, and LVEF should be reassessed before discontinuation. Lower LVEF cut-offs were recently shown to be feasible in breast cancer patients to enable optimal anticancer treatment. Interdisciplinary cardio-oncology cooperation is pivotal for optimal management of cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Survival in cancer is continuously improving with evolving oncological therapies. Cardiovascular short-term and long-term side effects therefore gain crucial importance for overall outcome [1]. Recent recommendations have proposed surveillance strategies for the timely detection of cardiotoxicity in patients undergoing chemotherapy or other oncological treatment [2]. Controversy remains about the optimal methods and when to initiate cardiac medication in order to continue life-saving cancer therapies [3]. Major challenges are the availability of monitoring and imaging resources [4]. Furthermore, cancer and heart diseases interact with each other [5]. Interdisciplinary cardio-oncology cooperation is needed to improve the management and long-term outcome of cancer patients and prevent cardiovascular complications of anticancer therapies.
The present paper reviews the current literature for detection and treatment of cardiotoxicity in patients undergoing cancer treatment in the context of the Austrian healthcare setting.
Definition of cardiotoxicity
Cardiotoxicity due to anti-cancer therapy is not only defined as heart failure (HF), but frequently presents as arrhythmia, e.g. atrial fibrillation (AF), atrioventricular (AV) block or ventricular tachycardia (VT), QT-prolongation, arterial hypertension, plaque rupture with acute coronary syndromes, coronary vasospasm, takotsubo syndrome, thromboembolism, pulmonary hypertension, diastolic dysfunction, HFpEF and myocarditis.
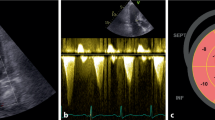
Although different cut-offs have been suggested, in the current ESC position statements [2, 6] cancer therapy-related cardiac dysfunction (CTRCD) is defined as any reduction of LVEF < 50% or > 10% absolute reduction from baseline falling below LVEF 50% (EACVI 53%) considered as the lower limit of normal. In addition, an impairment of > 15% from baseline global longitudinal strain in speckle tracking echocardiography is suggested for early detection of myocardial functional deterioration [6].
The onset of cardiotoxicity has been described as acute, during e.g. chemotherapy, early short-term within 1 year, and long-term after 1 year. Traditionally, cardiotoxicity was characterized as irreversible (type I), e.g. in anthracyclines, due to myocardial cell apoptosis and necrosis, or reversible (type II), e.g. in trastuzumab due to additive stunning of myocardial function; however, these categories are debated, as overlap exists. Cancer therapy related to myocardial injury and dysfunction is a continuous process and is also reflected by increased biomarkers [7, 8].
Specific potentially cardiotoxic anti-cancer agents
Anthracyclines
Anthracyclines are cytotoxic drugs with a 4-ring structure that interfere with the DNA and RNA synthesis, leading to cell death of rapidly proliferating cells. Anthracyclines such as doxorubicin, daunorubicin, epirubicin and idarubicin are effective in treating, e.g. leukemia, lymphomas, or solid cancers of the lungs, breast, stomach, uterus, ovaries and bladder [9]. The two main dose-limiting side effects include myelosuppression and cardiotoxicity. Introduction of cytokine treatment with the granulocyte colony-stimulating factor (G-CSF) has facilitated the management of myelosuppression. Multiple mechanisms of cardiotoxicity have been identified including increased oxidative stress with reactive oxygen species (ROS) formation, mitochondrial iron accumulation, and inhibition of topoisomerase II leading to myocardial cell apoptosis [10,11,12]. In experimental models, transcriptional activation of collagen synthesis and thus fibrogenesis was shown [13]. Typically, myocardial wall thinning, and interstitial fibrosis may develop after anthracycline treatment leading to remodeling and dilated cardiomyopathy, especially in younger patients or children [14].
Anthracyclines can cause acute (within 24 h after administration), subchronic (1–3 days), early chronic (< 1 year) and late onset chronic (> 1 year after treatment) cardiac toxicity. The incidence of LV dysfunction and decline in LVEF is dependent on the total cumulative doses and varies, i.e. for doxorubicin from 3–5% at a dose of 400 mg/m2 to 18–48% incidence at a dose of 700 mg/m2 ([2, 15]; table 1 and Fig. 1). A significant exponential risk increases even at a total anthracycline dose ≥ 250 mg/m2 of doxorubicin equivalent.
Cardiovascular side effects of anti-neoplastic therapies, overview. Frequency depending on baseline cardiovascular risk and dose of drug (modified after [2, 16, 18, 19]). This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/). This Table is not included under the Creative Commons CC BY license of this publication
Risk factors for anthracycline-related cardiotoxicity include age > 65 years or < 18 years, female sex, baseline LV dysfunction (asymptomatic LVEF < 50%, or high natriuretic peptide), prior cardiovascular disease (e.g. coronary artery disease, myocardial infarction; cardiac conditions associated with increased myocardial wall stress, such as arterial hypertension with LV hypertrophy, moderate or severe valvular disease), presence of cardiovascular risk factors (diabetes, hypertension, obesity, smoking, dyslipidemia), significant arrhythmia (e.g. ventricular tachyarrhythmia, AF), renal failure, prior or following chest irradiation, other potentially cardiotoxic drugs (e.g.. trastuzumab, concomitant alkylating or anti-microtubule agents or immunotherapy and targeted therapy), and genetic factors [2, 20]. The onset of cardiotoxicity most frequently occurs within the first year of treatment with the majority of patients remaining asymptomatic; however, overt HF may develop early or late even after decades [21, 22]. Importantly, if HF is detected early, functional recovery, when combined with sufficient HF treatment, is good, whereas late diagnosis is associated with a poorer prognosis [23].
Furthermore, pericarditis, myocarditis and acute arrhythmia as well as ECG(electrocardiogram)-ST changes may also be induced after anthracycline infusion. Right ventricular HF also frequently occurs late after anthracyclines and after combined treatment with radiation [2, 9].
Longer infusion rates of anthracyclines instead of rapid bolus administration can help to avoid cardiotoxicity. Liposomal doxorubicin formulations have been suggested as well as upfront dexrazoxane administration in high-risk patients or with previous high dose exposition [24, 25]. Controversy over dexrazoxane remains due to possible interference with efficacy and high costs. The avoidance of anthracyclines is a current research focus in oncology.
Recommendations for anthracycline treatment
A baseline echocardiography should be performed to assess LV function or any structural cardiac disease in all patients [6, 20]. After the end of treatment, echocardiography should be repeated. The biomarkers troponin and NT-proBNP (N-terminal pro B type natriuretic peptide) should be tested at baseline and at the end of treatment in all patients [8]. In high-risk cardiac patients, earlier assessment of cardiac function by echocardiography and biomarkers troponin and NT-proBNP should be repeated after every 2–4 cycles, and after end of treatment at 3 months and 6–12 months [6, 8, 20]. Similarly, in higher dose anthracycline regimens, earlier assessment of cardiac function (echocardiography) after a cumulative doxorubicin or equivalent dose of 240 mg/m2 should be considered. Troponin measurement has been suggested with each cycle of anthracyclines for high-risk patients and is easily feasible.
HER2 targeted therapy
Human epidermal growth factor receptors (HERs or ErbBs) have crucial roles in numerous cellular processes. HER2, a ligandless receptor of the HER family, is encoded by the ErbB2 gene (also known as HER2/NEU). Overexpression and/or gene amplification of HER2 is present in up to 20–25% of breast cancers, conferring poor prognosis and diagnosed more often in younger patients or at more advanced stages. Research has led to drugs specifically targeting HER2, such as the monoclonal antibodies trastuzumab and pertuzumab and small molecule tyrosine kinase inhibitors, such as lapatinib, neratinib and tucatinib [26,27,28,29,30,31]. Further treatment options include the antibody drug conjugates trastuzumab-DM1 and trastuzumab-deruxtecan. Together, these drugs have yielded a massive reduction of recurrence risk in early stage disease and a prolongation of overall survival in patients with metastatic HER2-positive breast cancer. Therefore, cardiac toxicity linked to HER2-directed treatment is of special concern.
Trastuzumab is a humanized monoclonal antibody that targets ErbB2, binding to its extracellular domain IV. It can cause cardiotoxicity that spans from asymptomatic decreases in LVEF to overt congestive HF, especially after previous exposure to anthracyclines or a short time (3 weeks vs. 3 months) between anthracycline and anti-HER2 treatment [32, 33]. The mechanism of anti-HER2 drug-induced cardiotoxicity includes structural and functional changes in contractile proteins and mitochondria, but it rarely leads to myocardial cell death, explaining the potential for reversibility [34]. The inhibition of the neuregulin-1/ErbB2 axis weakens myocardial repair mechanisms making it vulnerable to myocardial injury [35]. The role of neuregulin‑1 in the modulation of doxorubicin-induced oxidative damage with an impact on antioxidant enzymes was demonstrated, suggesting that trastuzumab acts as a modulator of anthracycline-related toxicity in a “dual hit” fashion [36].
Important factors for anti-HER2 drug-induced cardiotoxicity are of high risk in previous cardiovascular disease (very high in pre-existent HF or cardiomyopathy, high after myocardial infarction or in severe valvular disease, reduced LVEF < 50%), and medium risk even in borderline LVEF, arterial hypertension, obesity, smoking, chronic kidney disease, older age > 65 years (high risk > 80 years) or after radiation to the chest [2, 20, 37]. The implementation of different cardiotoxicity surveillance protocols has been proposed [2, 3, 6, 20, 38].
Trastuzumab cardiotoxicity typically already manifests during ongoing treatment but may also present after 1 year. Although trastuzumab-associated cardiotoxicity is not considered to be cumulative dose-related, a doubled rate of LV dysfunction was reported in treatment for 24 months compared to 12 months [39, 40]. In patients with HER2-positive breast cancer receiving adjuvant trastuzumab, cardiotoxicity was the most common reason for treatment interruption in 13.5% of patients (30% for HF and 70% for asymptomatic LVEF decline). In breast cancer patients who developed HF, an association between treatment with ACE inhibitors and beta-blockers and LVEF recovery at 12 months was seen, a further rechallenge with trastuzumab did not necessarily lead to redevelopment of HF, although the risk is in general highly increased [21, 41,42,43].
Given the major oncological advance that HER2-targeted therapies constitute, the potential negative impact on survival when delaying or discontinuing these therapies should always be considered [44]. The SAFE-HEaRt is the first trial to prospectively examine the safety of HER2-targeted therapies in breast cancer and already compromised cardiac function, a situation often encountered in everyday clinical practice [45, 46]. Importantly, the current results support continuation of HER2-targeted therapies in asymptomatic patients with LVEF 40–49% with cardioprotective HF medication in close cardiology collaboration.
The smaller SCHOLAR study also showed that it is feasible to continue trastuzumab uninterrupted in patients with mild cardiotoxicity (LVEF 40–50% or drop ≥ 15% from baseline), when administered in combination with ACE inhibitors and/or beta-blockers in a cardiology setting performing intensified monitoring, such as a cardio-oncology service [47]. The risk of moderate to severe HF is approximately 10%, and LVEF improved following trastuzumab discontinuation. In these studies, however, 90% of patients were able to complete the trastuzumab therapy and LVEF frequently improved with cardiac medication. As single arm trials, neither SCHOLAR nor SAFE-HEaRT can definitely evaluate if the cancer benefit outweighs the risk of lasting HF when continuing trastuzumab. Therefore, large randomized controlled trials are warranted. Based on the available studies the prescribing information of trastuzumab recommends assessing LVEF before initiation and at regular intervals during treatment. The reversibility of LV dysfunction and the opportunity to resume trastuzumab administration after improvement with HF treatment needs to be evaluated promptly and management should be individualized considering each patient’s characteristics [2, 38, 43, 48]. The cardiotoxicity risk of other anti-HER2-targeted therapies (e.g. lapatinib, pertuzumab, trastuzumab-emtansine, trastuzumab-emtansine (T‑DM1)) appears similar to that of trastuzumab and different combinations are currently applied [2, 37, 49, 50].
Recommendations for HER2-targeted therapies
Baseline risk factors should be assessed in all patients without delaying the begin of oncological therapy [20]. Pre-existent cardiac diseases or cardiac risk factors such as hypertension, diabetes or older age, borderline LVEF, previous cardiotoxicity with e.g. anthracyclines, chest radiation, pose an increased risk of cardiotoxicity. Serial monitoring by echocardiography including LVEF (3D if available) and global longitudinal strain (if available), as well as biomarkers (NT-proBNP and troponin) and symptom assessment should be implemented [2, 3, 6, 8, 20, 38]. The surveillance frequency depends on the baseline risk factors and any cardiac symptoms [6, 51].
In low-risk patients, echocardiography and biomarkers should be obtained every 3 months (at every 4 cycles of trastuzumab) [2, 6, 38]. In low-risk patients without cardiac history, it has been suggested that cardiac symptoms follow-up with biomarkers alone (NT-proBNP, troponin) may be sufficient, also especially during the corona virus (COVID-19) pandemic [50, 52]. In high-risk patients, frequent echocardiography monitoring and biomarkers are recommended every 2–3 cycles (about 6–9 weeks). In the case of LVEF drop, strain impairment > 15% and/or biomarker increases, prompt initiation of HF medication (ACEI/ARB, betablockers) is recommended [2, 8, 48, 53]. Controversies remain about the efficacy of early preventive treatment at the begin of chemotherapy if there is no cardiac risk [54].
Hormone modulating endocrine therapies
Breast cancer in women and prostate cancer in men are the most common types of cancer in Europe [55]. Endocrine interventions are cornerstones in their treatment and cardiovascular side effects become more important due to increasing incidence and improved survival [56,57,58,59]. Approximately two thirds of breast cancers are estrogen receptor positive.
Tamoxifen, a selective estrogen receptor modulator (SERM), reduces the risk of breast cancer recurrence and improves survival [54]. Although tamoxifen has been associated with a reduction in acute myocardial infarction, infarct-related mortality and lower rates of death from ischemic heart disease [60], extended tamoxifen treatment over 3–4 years has recently been demonstrated to be associated with an increased risk of stroke or TIA (HR 2.00, 95% CI 1.05–3.84), pulmonary embolism and venous thrombosis [56, 60,61,62]. Furthermore, an increase in body fat, hepatic steatosis, serum lipids/triglycerides and risk of diabetes has been reported with SERMs [56]. Aromatase inhibitors (AIs), such as anastrozole, letrozole and exemestane have further improved the cancer-specific outcome in postmenopausal women [63, 64] and were associated with less thromboembolic events [65]; however, an increased risk for acute ischemic heart disease (HR 2.03; 95% CI: 1.15–3.58) and arrhythmias were reported after long-term AI treatment over more than 4 years [62]. The estrogen receptor downregulator fulvestrant has been associated with less risk of cardiotoxicity, but some possible risk of hypertension [56] and ovarian function suppression, e.g. with triptorelin, has also been associated with risk of hypertension [56].
Prolongation of QTc and possible torsade de pointes ventricular tachycardia present an additional possible side effect of estrogen modulators. Despite the low absolute numbers of QTc prolongation occurrence, this is potentially harmful especially in patients with pre-existing cardiac arrhythmia and possible drug interactions with comedication that might affect the QTc time, e.g. antiarrhythmic agents, or CDK4/6 inhibitors (especially, ribociclib) in metastatic breast cancer [66].
Similarly, androgen blockade in men, especially with LHRH antagonists or abiraterone, is associated with QTc prolongation and has been related to an increased risk for supraventricular arrhythmia and conduction disease [56, 67].
Several other cardiovascular side effects of androgen deprivation therapy, such as hypertension, hypokalemia and edema may appear based on the resulting mineralocorticoid excess. Furthermore, androgen blockage was repeatedly shown to be associated with diabetes and dyslipidemia [68]. Prospective cohort studies and meta-analyses showed conflicting results concerning an increased risk of cardiovascular diseases [69, 70]. In patients without pre-existing cardiovascular disease androgen deprivation was associated with a 27% increased risk for HF, whereas in patients with pre-existing cardiovascular disease androgen blockade was associated with higher rates of arrhythmia and conduction disorders [71]. The LHRH agonists/antagonists are related to weight gain, hypertension, metabolic syndrome and coronary artery disease [56]. In the recent PRONOUNCE study of prostate cancer patients with concomitant atherosclerotic cardiovascular diseases, major adverse cardiovascular events at 1 year occurred in 5.5% of patients assigned to the GnRH antagonist degarelix and similarly in 4.1% assigned to the GnRH agonist leuprolide [72].
Recommendations for hormone modulating therapy
The cardiac risk profile should be optimized and monitored in all patients receiving a long-term endocrine therapy [56]. Statins, antihypertensive medication and platelet inhibitors should be initiated when indicated in addition to promoting a healthy lifestyle, non-smoking and exercising.
VEGF and tyrosine kinase inhibitors
Tyrosine kinases (TKs) are often overexpressed or mutated in cancer, a rationale to the development of tyrosine kinase inhibitors (TKIs), which are a class of small molecule drugs [73, 74]. The primary mechanism of action is through competitive inhibition at the adenosine triphosphate (ATP) binding pocket, leading to mitochondrial energy depletion stopping signaling that results in cellular proliferation [74]. While TKIs have been beneficial in improving patient outcomes, clinical trials have documented multiple cardiotoxicities. The phenotype of the cardiotoxicity varies across the available TKIs and the TKs targeted, indicating that no single mechanism is responsible for driving adverse reactions [73,74,75]. Below we highlight cardiotoxicities often reported with the use of TKIs.
-
Hypertension, ischemia, left ventricular dysfunction, HF
One of the most common cardiovascular side effects reported in clinical trials using TKIs is the development of hypertension in up to 80% of patients, with an incidence of symptomatic HF and LVEF decline in 2–15% with sunitinib [2, 38, 73, 74]. The risk of arterial thrombotic events (coronary/myocardial infarction, stroke, peripheral arteries) is increased threefold, especially in pre-existing atherosclerosis [76, 77]. TKIs targeting the vascular endothelial growth factor receptor (VEGFR-TKIs), such as sunitinib, ponatinib, pazopanib and sorafenib are commonly associated with severe hypertension as well as the anti-VEGF monoclonal antibody bevacizumab [73,74,75,76,77,78]. VEGF plays an essential role in maintaining the blood supply to solid tumors as they grow, so harnessing the ability to cut off angiogenesis and an essential cessation of the tumor blood supply is a strong therapeutic target. Hypertension during anti-VEGFR-TKI therapy is dose-dependent with a rapid onset of just hours or days after the start of treatment and has been related to the release of the vasoconstrictive agonist endothelin [73, 76, 79]. Clinical trials using sunitinib or sorafenib especially in renal cell cancer highlight the importance of monitoring the development of hypertension. Sorafenib inhibits a wide range of TKs including VEGFR‑2, VEGFR‑3, PDGFR (Platelet-derived growth factor receptor), c‑KIT (stem cell factor receptor), RAG (recombination activating gene), and BRAF (B‑Raf proto-oncogene). It is approved for unresectable hepatocellular carcinoma and advanced renal cell carcinoma. In trials, 17% of patients developed hypertension with sorafenib and 3% had an incidence of cardiac ischemia or myocardial infarction [75]. Vandetanib, used in thyroid cancer presents a high rate of hypertension and also QT prolongation, similarly to lenvatinib [80].
Close monitoring of the individual patients is important based on cardiac risk factors, with especially high risk in pre-existing coronary disease, hypertension, or other cardiovascular diseases [20]. Starting adequate antihypertensive treatment to avoid LVD, HF, myocardial ischemia, venous and arterial thromboembolic events, and acute coronary syndromes is crucial. Diltiazem should not be used in patients with TKIs due to possible interaction.
-
Arrythmias, AF and QT prolongation
A recent pharmacovigilance study provided evidence that several anticancer drugs represent potential independent risk factors for the development of AF [81]. While both atrial and ventricular arrythmias have been reported with TKI treatment, AF (AF) is more common.
Ibrutinib has revolutionized treatment for several B‑cell malignancies, such as chronic lymphocytic leukemia, mantle cell lymphoma or Waldenstrom’s macroglobulinemia, and inhibits Bruton’s TK protein. Ibrutinib is associated with the development of AF and other types of atrial arrhythmia [82, 83]. A study encompassing 4 large randomized controlled trials reported that at the 36-month follow-up, there was an incidence of 10.4% for AF that was increased with the duration of the treatment [84]. A potential mechanism for AF during ibrutinib is the inhibition of Bruton’s TK protein and tec protein-TK inhibition, which leads to a decrease in phosphoinositide 3‑kinase (PI3k)-Akt activity. Ventricular arrhythmias have also been reported in patients with ibrutinib, e.g. in the HELIOS trial (7 occurrences), as well as other arrhythmias overreported in the international pharmacovigilance database of real-life data [82]. Ibrutinib has also been related to bleeding events, which is important in anticoagulation due to AF [82, 84]. Sorafenib has also been associated with AF (incidence 5.1%), as well as ponitinib [73,74,75]. QT prolongation has been reported with dasatinib, sunitinib, vandetanib and nilotinib, which now has a black box warning for both QT prolongation and sudden cardiac death [85]. Studies have reported up to 26% of patients having QT prolongation longer than 30 ms with nilotinib treatment.
Basic science—mechanistic insights
Cardiotoxicities are multifactorial due to multiple targets of TKIs. In mice, sorafenib led to myocyte death due to necrosis [86]. Mice with myocardial ischemia and sorafenib developed pathological hypertrophy and had a significant increase in mortality [86]. Concomitant administration of metoprolol reversed the mortality increase, counteracting sorafenib-induced myocyte death [86]. In a direct assessment on human myocardium, sorafenib treatment affected contractility and decreased the concentration of systolic cytoplasmic calcium [87]. Sunitinib is a TKI targeting platelet-derived growth factor receptors (PDFGR) and VEFGRs on both human myocardium and isolated mouse cardiomyocytes. Sunitinib had a dose-dependent effect leading to worsening contractile function in human myocardium and had a negative impact on calcium homeostasis and sarcomere shortening in isolated mouse cardiomyocytes [88].
Recommendations for TKIs
Due to exacerbation of pre-existing CVD, direct myocardial toxicity, and hypertension, 5–10% of patients receiving VEGFi (vascular endothelial growth factor inhibitors) TKIs develop LVD [6, 74]. Therefore, a standardized baseline CV risk assessment prior to starting anti-cancer therapy is crucial. Specific evidence-based and practical risk assessment tools have been developed which are easy to use in clinical routine [20]. Echocardiography should be considered early after treatment initiation (2–4 weeks) in high-risk patients, and in all patients every 4 months during the first year. In asymptomatic patients after the first year, echocardiography should be performed 1–2 times/year. Natriuretic peptides (NTproBNP, BNP) should be measured at baseline, followed by at least 3‑monthly measurements depending on CV risk stratification. Markers of cardiac injury, such as troponins are less thoroughly validated but may be considered as well. Daily blood pressure measurements (at home) and monthly ECG recordings should be performed. Initiation of an ACEI/ARB, beta-blocker and statin for cardioprotection prior to starting TKI treatment is a potential option but warrants further investigations. Diltiazem or verapamil are not recommended due to interactions.
Taken together, patients receiving treatment with TKIs should be closely monitored and promptly treated for any acute negative response, such as hypertension or ischemia, and any adverse effects that may develop after a longer duration of treatment, such as AF or HF.
Immune checkpoint inhibitors
Immune checkpoint inhibitors (ICIs) are antibodies that block negative regulators of the T cell immune response, including cytotoxic T lymphocyte-associated protein‑4 (CTLA-4), programmed cell death protein‑1 (PD-1) and PD‑1 ligand (PD-L1) [89]. ICIs have revolutionized therapies in an increasing number of cancers entities or metastatic settings with an impressive improvement in overall survival with often many years of remission in metastatic melanoma, lung cancer, or refractory Hodgkin’s lymphoma [90,91,92,93]. Currently, 7 ICIs are FDA approved (10 in EU, Japan and China) with presently over 50 indications and rapidly expanding, e.g. gastric, colorectal, renal cell, laryngeal, breast cancer and urogenital; however, the augmented immune response has led to a range of immune-related adverse events (irAE), e.g. interstitial pneumonia, colitis, hypothyroidism, hypophysitis, hepatitis, cutaneous dermatitis, nephritis, uveitis, myocarditis, myasthenia gravis and myositis. CTLA‑4 inhibitors include ipilimumab, PD‑1 inhibitors nivolumab or pembrolizumab, and PD-L1 inhibitors avelumab, atezolizumab or durvalumab.
ICI-associated cardiovascular toxicity was rare in trials or pharmacovigilance databases (1% with up to 2.4% in ICI combinations), but potentially life threatening in fulminant autoimmune myocarditis (25–>50% mortality rate), with an increasing incidence of cardiac events reported in growing use of ICIs [94,95,96]. A higher real-life rate of cardiovascular events was assessed in a recent Danish registry in lung cancer or melanoma patients (1-year absolute risk of cardiac events of 9.7% and 6.6% with PD‑1 inhibitors, respectively, and melanoma 7.5% with CTLA‑4 inhibitors) [97]. Statistically, cardiac side effects occur early, with a median time to onset of 27–65 days (range 2–454 days) [95, 96, 98]. Approximately 2/3 of ICI-associated myocarditis cases were evident after the first or second ICI dose, or within the first 6–8 weeks of therapy [99]. Combination immunotherapy (CTLA‑4 with PD‑1 inhibitor) is a predominant risk factor for ICI-associated myocarditis. The combination of nivolumab and ipilimumab conferred a 4.74-fold risk of developing myocarditis compared with treatment with nivolumab alone, with more severe grade and higher fatality, as well as higher rates of other concomitant immune-induced effects ,such as myasthenia gravis or myositis [100].
The regional distribution of ICI cardiotoxicity and local inflammation may occur in different variations and severity, and include pericarditis and/or pericardial effusion, coronary or other arterial vasculitis, e.g. temporal arteritis, coronary acute plaque rupture and myocardial infarction (myocardial ischemia, subendocardial necrosis), takotsubo syndrome, arterial vasospasm, arrhythmias, high-grade AV block or acute HF [101]. The typical immune-mediated, lymphocytic acute myocarditis may appear as patchy, edematous, and necrotizing. Elevated troponin was observed in 10% of patients with ICI also without symptoms, which might reflect subclinical cardiac dysfunction due to ICI-induced myocardial inflammation [99, 102]. In the presence of other irAEs in a patient with cardiac symptoms, elevated biomarkers, new ECG or echocardiography findings, the probability of ICI-associated myocarditis increases [102, 103]. Importantly, a normal LVEF does not rule out ICI myocarditis, as LVEF was observed as normal in a very high percentage (38%) of cases. Echocardiography may show diffuse LV systolic dysfunction or new regional wall motion abnormalities at development of myocarditis. Preservation of normal cardiac dimensions may be suggestive of an acute process, whereas remodeling and dilatation suggest a chronic myocardial process.
Cardiac magnetic resonance imaging (CMR) is important for tissue characterization and identification of myocarditis; however, not always reliable [104,105,106]. Indeed, CMR may be unremarkable in a substantial proportion of patients (in up to 50% of cases) and repetitive imaging may increase sensitivity [106]. The presence of LGE increased from 21.6% in CMR performed within 4 days of admission to 72.0% on day 4 or later [106]. Of course, this will cause difficulties in available resources, not only in Austria. In patients where CMR is contraindicated or not available, a cardiac FDG-PET-CT (fluorodeoxyglucose-positron emission tomography-computed tomography) is an alternative image modality to assess inflammation [104]. The gold standard is the histopathological diagnosis by endomyocardial biopsy, and should be pursued in experienced centers, considering the potential consequences of immunosuppression treatment and/or withholding life-saving ICIs [104, 107]. It is essential to clarify the diagnosis of myocarditis, as potentially life-threatening, and the possible rechallenge with ICI after recovery [107]. Furthermore, as was identified in a pharmacovigilance database, patients can suffer from concomitant coronary artery disease, progression of atherosclerosis with plaque rupture induced by ICI inflammation, or vasculitis and ICI-associated myocarditis, so that a biopsy can be performed during angiography in symptomatic patients with troponin, ECG and/or echocardiography abnormalities [104, 108].
ICI myocarditis is usually, but not always, accompanied by elevations in serum biomarkers of myocardial injury (troponin) and LV stress (NT-pro-BNP or BNP) [8, 96, 104]. Biomarkers are not highly specific, at present troponin is considered more specific for myocarditis [8, 99, 104]. Troponin was elevated in 94% of ICI myocarditis [96]. ICI-associated myocarditis can present with various forms of arrhythmia including AF, ventricular arrhythmias and conduction disease, therefore strict ECG monitoring is indicated [98,99,100,101, 108, 109].
Recommendations for surveillance and treatment of ICI myocarditis
Currently, no prospective trial data are available. Recently, surveillance and immunosuppressive treatment algorithms have been suggested [16, 38, 107, 110, 111].
Prior to initiating ICI, baseline cardiac history and cardiovascular risk factors should be assessed [20]. Baseline troponin, NT-pro BNP, ECG and echocardiography prior to ICI initiation should be obtained in all patients for comparison reference in case of cardiac complications. After ICI initiation, troponin measurement has been proposed on a weekly basis for 6 weeks, then every 2 cycles, especially in high-risk cardiac patients, e.g. in ICI combination therapies [108].
In asymptomatic patients with elevated troponin on surveillance, a 12-lead ECG, serum CK(creatinin kinase)/CK-MB(creatine kinase myocardial band) and serial troponin should be assessed. Patients should be referred to a cardiologist, and echocardiography or CMR considered. In asymptomatic patients and isolated troponinemia, resuming ICI therapy can be considered if troponin returns to normal within 2 weeks and no cardiac pathologies are present in work-up [16, 102].
In symptomatic patients (e.g. chest pain, dyspnea, palpitations, presyncope, syncope), abnormal ECG or echocardiography or CMR findings, hold ICI treatment and admit patient to hospital with cardiac monitoring. Myocardial infarction and other etiologies should be ruled out (coronary CT and/or angiography), echocardiography and CMR obtained, and endomyocardial biopsy considered (even with unremarkable echocardiography or CMR if clinical suspicion is high) [110].
In hemodynamically stable ICI myocarditis without arrhythmia and concomitant signs of potential fulminant course (myositis, myasthenia) start patients with i.v. methylprednisolone 500–1000 mg i.v. bolus for 3 days and continue with 2 mg/kg/day [16, 38, 100, 110, 111]. If abnormalities resolve, methylprednisolone should be tapered over at least 4 weeks. If no improvement in 24 h or patient unstable (hypotension, arrhythmia, or sudden EF decrease), a transfer to ICU and begin i.v. methylprednisolone at 1 g daily is recommended. If the patient continues to be unstable, adding alternative agents, such as antithymocyte globulin (ATG), tacrolimus, infliximab, mycophenolate mofetil, or rituximab should be considered early. Recently, especially abatacept has been reported for severe immune myocarditis, also in an experimental concept, and tocilizumab [111,112,113,114]. Pacemaker insertion may be necessary due to high degree AV block. Importantly, treatment should not be delayed and contact to experienced centers sought early.
New immune therapies, chimeric antigen receptor (CAR) T-cell therapies
Immunotherapy is revolutionizing oncology by harnessing the native immune system for treating even advanced malignancies. The emerging chimeric antigen receptor T cell (CAR‑T, e.g. tisagenlecleucel, axicabtagene ciloleucel) therapies induce tumor cell apoptosis, but may provoke severe cytokine release syndromes (CRS) with acute HF, hypotension, multiorgan dysfunction and high fatality rates [115,116,117]. Interleukin‑6 (IL-6) is a primary driver of inflammation in CRS, and also associated with cardiovascular complications [116].
Bispecific T cell engager therapy (BiTE, e.g. blinatumomab) showed grade 3–4 CRS in 19% of patients [116]. Surveillance for adverse cardiovascular effects is warranted in these evolving immunotherapies, and further knowledge is needed.
Alkylating, antimicrotubule agents, fluoropyrimidines
Other common chemotherapies bearing a cardiotoxicity risk are the alkylating substances cyclophosphamide, ifosfamide, the platinum-based cisplatin and carboplatin, the antimicrotubule taxanes, i.e. paclitaxel and docetaxel, and the antimetabolites fluoropyrimidines (5-FU fluorouracil) ([118]; Table 1).
Cardiotoxicity of cyclophosphamides is mainly associated with higher doses, previous anthracyclines, radiation, trastuzumab combinations and older age, with an incidence of HF up to 28% [118]. Cisplatin or ifosfamide can induce myocardial ischemia and coronary plaque rupture. Combining docetaxel and cyclophosphamide is in general less cardiotoxic than a combination with anthracyclines. The non-anthracycline regimen in breast cancer with docetaxel, carboplatin, and trastuzumab (TCH) was less cardiotoxic than with anthracycline [119].
Cancer including radiation and chemotherapies may lead to accelerated coronary atherosclerosis and a prothrombotic state [5]. The anti-metabolites 5‑FU and the oral prodrug capecitabine can frequently cause chest pain usually early within hours or days after initiation of 5‑FU, and a work-up for ischemia should be initiated. ECG changes and/or biomarker increases were found in up to 43% of patients, the risk of mortality ranged from 2–13% [118]. Risk factors include high dose of 5‑FU or continuous infusion, pre-existing cardiovascular disease and concurrent other chemotherapies. The capecitabine-induced cardiotoxicity was lower and ranged between 3–9%. Coronary vasospasm is also caused via endothelial injury and vasoconstriction by 5‑FU infusion. Second to anthracyclines, 5‑FU has been considered as one of the most common cardiotoxic agents [120, 121].
In taxanes, myocardial ischemia and infarction have been reported less frequently in 3% of patients receiving paclitaxel, and after docetaxel in 1.7%, as well as HF in 2.3–8% [118].
Recommendations during cisplatin or fluoropyrimidine treatment
In chest pain, new ECG changes, elevated biomarkers with troponin, a coronary syndrome needs to be excluded. Higher risk is present in patients with previous cardiovascular disease and atherosclerosis risk factors.
Proteasome inhibitors (PI) and immunomodulatory agents (IMID)
Inhibition of proteasome blocks cell proliferation and induces apoptosis in tumor cells [118]. Bortezomib, carfilzomib and ixazomib are targeted therapies for multiple myeloma. Proteasome inhibition perturbs protein homeostasis and function of cardiomyocytes, significant in already present cardiac stressors. Especially carfilzomib, an irreversible PI, has a higher risk of cardiovascular toxicity including myocardial ischemia or infarction, LV dysfunction and symptomatic HF (about 7%) [122]. Cardiotoxicity occurred early during PI treatment and was largely reversible with (intermittent) cessation and initiation of HF medication [123]. A high risk is present in previous CVD, older age, reduced or borderline LVEF, and previous venous thrombosis or embolism [20]. Elevated BNP levels predict major adverse cardiac events (MACE) [8, 124].
The immunomodulators lenalidomide, as well as thalidomide or pomalidomide, are associated with an increased risk of venous thromboembolism, acute coronary artery thrombosis, as well as AF or bradycardia [125,126,127]. Combination regimes with bortezomib and lenalidomide are a standard therapy for multiple myeloma, or with carfilzomib and lenalidomide in relapsed or refractory myeloma. Main cardiovascular complications of the combinations of PI and IMIDs are LVD, HF, ischemia, infarction, atrial and ventricular arrhythmia, venous thromboembolism and arterial thrombosis [2, 81, 123].
Recommendations for PI and IMID
Due to relatively high cardiovascular event rates, a baseline echocardiography is recommended in all multiple myeloma patients scheduled to receive a PI, also assessing for cardiac AL amyloidosis, and surveillance in medium to high-risk patients especially in carfilzomib [6, 20]. Echocardiography is strongly recommended if new cardiac symptoms appear. Measurement of BNP at baseline and during the first few cycles in patients receiving PIs should be considered [8]. Thromboprophylaxis is recommended in lenalidomide-based regimens.
Cyclin-dependent kinase 4/6 inhibitors
CDK 4/6 inhibitors are a major milestone for hormone receptor-positive and HER2-negative metastatic breast cancer [128]. Palbociclib, ribociclib, and abemaciclib, have significantly improved progression-free survival combined with endocrine therapy [125]. CDK 4/6 inhibitors, especially ribociclib, have been associated with QT prolongation [129].
Recommendations for CDK 4/6 inhibitors
For ribociclib, ECG monitoring is recommended (baseline, day 15, and begin of cycle 2) with QTc value of ≤ 450 ms at initiation. Other QT prolonging concomitant drugs should be considered in CDK 4/6 inhibitors, as well as electrolyte imbalance, e.g. in diarrhea or emesis.
Therapy of cardiotoxicity and general recommendations in oncological agents
In all cancer patients treated with potentially cardiotoxic therapy, it is generally recommended to strictly control cardiovascular risk factors without delaying the oncological therapy [2, 20, 38].
In potential CTRCD and HF risk, LVEF should be determined before and periodically during treatment, usually by echocardiography and biomarker surveillance ([6, 8, 38, 51]; Table 2). If LVEF deteriorates, LVEF should be reassessed after 2 weeks before stopping the life-saving oncological treatment, especially in asymptomatic patients [2, 6]. If LVEF deteriorates > 10% to values < 50%, or in impaired strain (> 15% change in GLS), ACE inhibitors or ARB and beta-blockers are promptly recommended to prevent further deterioration as these patients are at high risk to develop manifest HF [21, 23, 48, 130,131,132]. Patients with asymptomatic or symptomatic deterioration of LVF during or after tumor treatment should be treated according to current HF guidelines [130]. Optimal and early initiation of HF treatment is associated with improved LV function after chemotherapy [21], Currently, sacubitril/valsartan in cardiotoxicity has only been evaluated in few studies [133, 134].
In general, patients with cancer therapy cardiotoxicity should be referred to a cardio-oncology specialist in close cooperation with the oncology team to commonly assess the duration or even interruption of chemotherapy until the patient is clinically stable. It is important to critically discuss risk versus benefits of further treatment with the previous cancer regimen based on clinical factors, such as LV dysfunction, NYHA status, prognosis of the disease, and alternative treatment options considering the spectrum of side effects.
In case an anticancer drug previously causing cardiotoxicity is readministered, it is recommended that concomitant cardioprotective therapy with ACEI or ARB and beta-blockers is provided and continued indeterminately.
Radiation therapy: early and late cardiotoxicity
Irradiation of the heart is unavoidable when the target volume is close, as in left breast cancer or frequently mediastinal in e.g. Hodgkin’s lymphoma or thymus cancer. After irradiation, patients are at risk of long-term radiation-induced heart disease (RIHD, e.g. valvular, pericardial, myocardial, coronary disease, conduction system) and peripheral artery disease depending on the field of radiation [136, 137]. Risk factors for RIHD include anterior or left chest radiation, a high cumulative radiation dose, age < 50 years, tumor in or near to the heart, lack of shielding, concomitant chemotherapy particularly with anthracyclines, smoking and medical comorbidities (diabetes mellitus, hyperlipidemia, hypertension, and obesity) [137]. The effects of radiation of the heart typically manifest years after exposure [136,137,138]. Current strategies to prevent cardiac impairment are limiting cardiac exposure by shielding and modern radiation techniques, e.g. breathing maneuvers.
LVD and HF are relatively common serious side effects of radiation therapy. The actual incidence of radiation-induced cardiotoxicity is difficult to evaluate due to long delay between exposure and clinical manifestation of heart disease, concomitant cardiotoxic chemotherapy and continuous improvements in radiation techniques. Studies found a relative risk of fatal cardiovascular events of 2.2–12.7 in survivors of Hodgkin lymphoma and 1–2.2 in patients with breast cancer [136, 139, 140]. In breast cancer treated in the era 1980–2000, the risk of cardiotoxicity was highest in patients treated with both left breast radiotherapy and cardiotoxic chemotherapy, suggesting a synergistic effect on cardiac risk. LVD is generally observed when radiotherapy is combined with anthracyclines.
In the acute phase, acute myocarditis related to radiation-induced inflammation with transient repolarization abnormalities and mild myocardial dysfunction can occur. In the long term, diffuse myocardial fibrosis with relevant systolic and diastolic dysfunction (including restrictive cardiomyopathy) and conduction disturbances can occur, e.g. AV block necessitating pacemaker [136,137,138].
Supradiaphragmal and, in certain patient groups, even infradiaphragmal radiotherapy may be associated with a higher incidence of ischemic heart disease through the development of severe atherosclerotic and non-atherosclerotic disease. Radiation-related cardiac disease in patients with lymphoma typically manifests 15–20 years after the initial treatment, and younger patients are more susceptible than older patients [139]. Survivors of Hodgkin’s lymphoma have a 4–7-fold increased risk of CAD compared with the general population and a cumulative incidence of CVD up to 50% 40 years after treatment. Presentation of CAD is more often atypical with diffuse sclerosis [137, 138]. The prevalence of silent ischemia may be higher than in conventional CAD, possibly because of concomitant neurotoxicity of radiotherapy or chemotherapy affecting the patient’s perception of angina. Sudden cardiac death in irradiated patients has been reported and linked to diffuse intimal hyperplasia of all coronary arteries or to significant left main coronary artery stenosis [136,137,138]. Ostial lesions are frequent and a potentially life-threatening complication. The most exposed coronaries are the left anterior descending artery during left breast irradiation and the left main stem, circumflex and right coronary arteries during treatment for Hodgkinʼs lymphoma. A higher prevalence of stress test abnormalities and impaired LV strain has been found among women irradiated for left breast cancer compared with right-sided cancer [141].
Radiation-induced valvular heart disease is common, affecting 10% of treated patients, and includes fibrosis and calcification of the aortic root, aortic valve cusps, mitral valve annulus and typically the base and middle portions of the anterior mitral valve leaflets, sparing the mitral valve tips and commissures, allowing distinction from rheumatic disease [137]. Many patients will later need valvular or coronary interventions [142, 143]. Transcatheter aortic valve replacement may be preferable to surgical procedures. In contrast, in mediastinal involvement treated today with 20 or 30 Gy, the 30-year risk may be less increased only by 1.4% [143, 144]. Radiation calcified valve disease and heart failure are frequently encountered years after radiation [145].
Any type of supraventricular arrhythmia may arise acutely, of which AF is the most common. Ventricular arrhythmias can be related to QT prolongation, to acute and chronic toxicity of radiotherapy (mainly LV dysfunction and ischemia) and to predisposing factors. Sinus node dysfunction and conduction defects may arise following radiotherapy and are often permanent [137, 138].
Acute pericarditis with typical chest pain, fever, ST‑T changes and large effusions may develop 2–145 months after thoracic radiotherapy, with an absolute cumulative incidence of 2–5%. Treatment of pericardial effusion consists primarily of non-steroidal anti-inflammatory drugs and colchicine. Pericardiocentesis may be required in hemodynamic compromise, followed by surgical pericardial windowing if needed. Chronic thickening and constrictive pericarditis may develop after high-dose radiotherapy [136, 144].
Endothelial damage and thrombus formation may occur also after irradiation of small cerebral vessels, leading to increased carotid stiffness and intima media thickness and direct irradiation to advanced carotid atherosclerosis at around 10 years after radiotherapy. The risk of stroke is increased, at least doubled, after mediastinal, cervical or cranial radiotherapy [146]. Similar consequences are reported for the aorta (porcelain aorta) and other peripheral arteries, including the subclavian and iliofemoral vessels [136, 137, 146]. Also, the mammary artery may be affected, which is relevant in planning of coronary artery bypass surgery [142]. Additional pericardial adhesions and pulmonary irradiation-induced fibrosis lead to higher perioperative complications and bleeding in heart surgery [137, 138, 142]. Newer radiation procedures today lead to significantly lower cardiac side effects.
Recommendations after radiation therapy
Especially younger survivors of breast cancer, lymphoma or other mediastinal cancers after chest radiation need to be followed for cardiovascular late effects including coronary disease, valve disease and pericardial constriction by echocardiography, clinical symptoms evaluation, stress test and biomarkers after 3–5 years and long term after that, with coronary evaluation by CT or angiography as needed [137, 138]. Measures for cardiovascular disease prevention should be considered early. Risk factors such as high lipids should be treated early by statins, smoking cessation, antihypertensive medication and platelet inhibitors started where indicated. Transcatheter procedures may be preferable to surgical interventions after chest irradiation.
Survivors of childhood cancer
Survival of childhood malignancies has considerably increased in the last decades with current 5‑year survival rates > 80% [147]. After exposure to cardiotoxic medication and/or radiation early in their lifetime, survivors are at risk for late adverse events. Although many patients after childhood cancer may still die due to recurrence of the primary malignancy or secondary neoplasm, cardiovascular diseases are the most common non-neoplastic cause of premature mortality in this population [148, 149]. Survivors of pediatric cancers have a higher prevalence of cardiovascular risk factors, predominantly hypertension and dyslipidemia, as well as obesity and diabetes, also due to growth factor and other metabolic impairments after chemotherapy or whole body irradiation in hematopoietic stem cell transplantation [150, 151]. Moreover, a 2–5-fold increase of relative risk for cardiovascular diseases (7–10% cumulative long-term risk) has been reported in these patients [149, 151, 152]. Cardiomyopathies and venous thromboembolism account for more than 50%, with highest risk after exposure to anthracyclines, chest or cerebral radiation [151]. Although Scandinavian data have demonstrated a reduction of the increased cardiovascular risk over time, others have shown that the risk remains beyond the age of 60 years and an increase with age [149, 151, 152]. Based on these observations, it is recommended that adult survivors of childhood cancers should be regularly screened for traditional cardiovascular risk factors and examined for cardiomyopathy and coronary disease [2, 6, 147, 153, 154].
Surveillance by NT-proBNP may have only moderate sensitivity and troponin less useful, therefore regular echocardiography at intervals of no more than 5 years is advised (Table 2; [2, 8, 147, 153, 155, 156]). Global longitudinal strain was impaired in 9–30% of childhood cancer survivors even in normal LVEF [157]. Despite lack of randomized trials, asymptomatic reduction of LVEF should be treated with RAAS inhibition and beta-blockers and followed closely [2, 158]. Apart from medical therapy, regular exercise is recommended for survivors treated with anthracyclines and/or chest radiation [153]. Female adult survivors treated with cardiotoxic chemotherapy or chest radiation are strongly advised to consult a cardiologist before planning pregnancy and echocardiography and biomarkers should be considered [6, 8, 153].
Recommendations in survivors of childhood cancer
Regular follow-up in adult survivors of childhood cancer is advised with ECG, echocardiography and cardiac risk factor treatment, e.g. statins in hyperlipidemia, metabolic syndrome, every 5 years, biomarkers if available and evaluation for early coronary disease at least by the age of 40 years.
Special aspects
Long-term cardiovascular monitoring
Survival, especially in breast cancer and lymphomas, has substantially increased over the past decade [159]. It is imperative to raise awareness of possible cardiac sequences among cancer survivors in general, as well as to provide appropriate follow-up in clinical practice, as in survivorship programs managed by oncology or hematology centers, but not always available [2,3,4]. Cardio-oncology centers should work with such survivorship programs to assure optimal cardiac follow-up after potentially cardiotoxic therapies. Patients should be informed of their increased risk of CVD at the end of their oncological therapy and should be advised and supported to make appropriate lifestyle modifications. They should be instructed to promptly report early signs and symptoms of CVD. A yearly history and physical examination to assess for early signs of CVD, as well as regular follow-up with imaging is recommended in the recent consensus documents [2, 3]. Personalized echocardiographic surveillance and long-term follow-up according to the baseline cardiotoxicity risk (low, medium or high) aligned to therapy-related and patient-related factors is recommended [6, 20].
In breast cancer or Hodgkin’s lymphoma, echocardiography is recommended at 12 months and 5 years post-completion of anthracycline chemotherapy in patients with low or medium baseline risk, in patients with high baseline risk at 6 and 12 months, annually for 2 or 3 years thereafter, and then in 3–5-year intervals for life. In breast cancer asymptomatic patients after HER2-targeted treatment with medium or high baseline cardiotoxicity risk, a follow-up echocardiogram and clinical assessment should be considered 3–6 months and 12 months after the final dose [3, 6, 20, 51]. In patients who require long-term trastuzumab treatment in the setting of metastatic disease, regular long-term echocardiographic surveillance is recommended [3, 6]. Cardiac biomarkers and imaging are synergistic and should be applied together [8]. Biomarker surveillance after anthracycline therapy with BNP/NT-proBNP and troponin is recommended 12 months after the final cycle, in high-risk patients also 3 and/or 6 months after the final cycle. A similar biomarker surveillance after HER2-targeted therapies is recommended [8].
Following radiation, evaluation for CAD and ischemia is recommended in patients with a history of mediastinal radiation as in breast cancer or Hodgkinʼs lymphoma, even if asymptomatic, starting 3–5 years post-treatment and then at least every 5 years thereafter [2, 137, 154]. Patients irradiated for head and neck cancer or lymphoma should undergo cerebrovascular ultrasound screening, especially beyond 5 years after irradiation. Duplex imaging may be considered at least every 5 years or earlier and/or more frequently if the results of the first examination are abnormal. Stringent risk factor management is required to halt plaque progression. Antiplatelet drugs and statins should be considered where indicated.
Exercise therapy for oncological patients
The efficacy of exercise therapy during and after cancer therapy has been confirmed in a number of trials [160, 161]. Despite some limitations, even prediagnosis exercise exposure is associated with a significant reduction in subsequent cardiovascular events in long-term survivors of primary breast cancer [162]. An analysis of 56 trials involving 4826 participants demonstrated an improvement in quality of life and physical ability during and after an exercise-training program [160]. In particular, aerobic exercise is considered a promising non-pharmacological strategy to prevent and/or treat chemotherapy-induced cardiotoxicity [163]. The importance of exercise as a safe and effective strategy to improve physical, muscular, and cardiovascular fitness in adult patients with cancer improving their quality of life (QOL) has been emphasized [164]; however, the timing, type, intensity, and frequency of exercise that gives maximum cognitive and physical benefit are still unclear. The recent AHA statement introduces the concept of cardio-oncology rehabilitation and points out that low cardiorespiratory fitness is associated with a higher incidence of short-term and long-term treatment-related toxicities (e.g. cardiovascular disease), higher symptom burden (e.g. fatigue) and increased risk of all-cause and cancer-specific mortality in patients with cancer [165]. Ongoing trials will determine the role of exercise to prevent and ameliorate cardiac and other side effects of chemotherapy, e.g. in breast cancer or other cancer entities [166].
Conclusions and gaps of evidence
As oncology therapies rapidly evolve and cancer survival improves dramatically, cardiac side effects emerge as important determinants of long-term QOL and outcome.
Open questions remain concerning the correct timing and which medication should be administered to avoid or treat overt cardiotoxicity in oncology treatment.
Biomarker elevations need to be differentiated to other cardiac comorbidities (e.g. pulmonary embolism, coronary syndromes, arrhythmias) or volume changes in intravenous infusions, diarrhea or emesis in cancer therapies. Suggested timepoints of biomarker assessment during cancer therapy are summarized (Table 3), although further studies will be needed [8].
Availability and increasing costs of repeated frequent cardiac imaging, biomarkers and other examinations for cardiovascular surveillance during and after cancer treatments are limiting factors, not only in Austria.
Considering that outcome in cardiac diseases has also strikingly ameliorated in the last decade, patients with pre-existing HF and other CVD are increasingly in need of special cardio-oncology care when developing additional cancer [167, 168]. Baseline assessment of risk factors for cardiotoxicity and regular surveillance during oncological treatment are recommended. Cooperation of oncologists and cardiologists is mandatory to provide optimal care to patients with cancer and/or heart diseases and their follow-up in long-term survivors.
Outlook in Austria
The necessity of frequent cardio-oncology surveillance with cardiac imaging, biomarkers, ECG and clinical examinations of patients with increasing age and comorbidities opens issues of costs and feasibility with current resources in Austria.
Increased imaging availability of echocardiography, CMR and CCT will be crucial in the future. Reimbursement issues concerning echocardiography and biomarker (troponin, BNP) assessment need to be clarified in the Austrian healthcare system, especially outside of hospitals. Currently, very few specialized cardio-oncology units are available in Austrian hospitals, and further infrastructure and collaboration need to be established [169].
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- AF:
-
Atrial fibrillation
- AI:
-
Aromatase inhibitor
- ARB:
-
Angiotensin receptor blocker
- CAD:
-
Coronary artery disease
- CMRI:
-
Cardiac magnetic resonance imaging
- CTRCD:
-
Cancer therapeutics-related cardiac dysfunction
- CVD:
-
Cardiovascular disease
- EACVI:
-
European Association of Cardiovascular Imaging
- ESC:
-
European Society of Cardiology
- HER:
-
Human epidermal growth factor receptor
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- ICI:
-
Immune checkpoint inhibitor
- LV:
-
Left ventricle
- LVD:
-
Left ventricular dysfunction
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major cardiac events
- RIHD:
-
Radiation-induced heart disease
- TKI:
-
Tyrosine kinase inhibitor
References
Shapiro CL. Cancer survivorship. N Engl J Med. 2018;379(25):2438–50.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC committee for practice guidelines: the task force for cancer treatments and cardiovascular toxicity of the European society of cardiology (ESC). Eur Heart J. 2016;37(36):2768–801.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2014;15(10):1063–93.
Stankovic I, Dweck MR, Marsan NA, Bergler-Klein J, Holte E, Manka R, et al. The EACVI survey on cardiac imaging in cardio-oncology. Eur Heart J Cardiovasc Imaging. 2021;22(4):367–71.
de Boer RA, Hulot JS, Tocchetti CG, Aboumsallem JP, Ameri P, Anker SD, et al. Common mechanistic pathways in cancer and heart failure. A scientific roadmap on behalf of the translational research committee of the heart failure association (HFA) of the European society of cardiology (ESC). Eur J Heart Fail. 2020;22(12):2272–89.
Čelutkienė J, Pudil R, López-Fernández T, Grapsa J, Nihoyannopoulos P, Bergler-Klein J, et al. Role of cardiovascular imaging in cancer patients receiving cardiotoxic therapies: a position statement on behalf of the heart failure association (HFA), the European association of cardiovascular imaging (EACVI) and the cardio-oncology council of the European society of cardiology (ESC). Eur J Heart Fail. 2020;22(9):1504–24.
López-Sendón J, Álvarez-Ortega C, Zamora Auñon P, Buño Soto A, Lyon AR, Farmakis D, et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: the CARDIOTOX registry. Eur Heart J. 2020;41(18):1720–9.
Pudil R, Mueller C, Čelutkienė J, Henriksen PA, Lenihan D, Dent S, et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: a position statement from the cardio-oncology study group of the heart failure association and the cardio-oncology council of the European society of cardiology. Eur J Heart Fail. 2020;22(11):1966–83.
Henriksen PA. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart. 2018;104(12):971–7.
Vejpongsa P, Yeh ET. Topoisomerase 2β: a promising molecular target for primary prevention of anthracycline-induced cardiotoxicity. Clin Pharmacol Ther. 2014;95(1):45–52.
Murabito A, Hirsch E, Ghigo A. Mechanisms of anthracycline-induced cardiotoxicity: is mitochondrial dysfunction the answer? Front Cardiovasc Med. 2020;7:35.
Cardinale D, Iacopo F, Cipolla CM. Cardiotoxicity of anthracyclines. Front Cardiovasc Med. 2020;7:26.
Gyöngyösi M, Lukovic D, Zlabinger K, Spannbauer A, Gugerell A, Pavo N, et al. Liposomal doxorubicin attenuates cardiotoxicity via induction of interferon-related DNA damage resistance. Cardiovasc Res. 2020;116(5):970–82.
Bansal N, Blanco JG, Sharma UC, Pokharel S, Shisler S, Lipshultz SE. Cardiovascular diseases in survivors of childhood cancer. Cancer Metastasis Rev. 2020;39(1):55–68.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97:2869–79.
Lyon AR, Yousaf N, Battisti NML, Moslehi J, Larkin J. Immune checkpoint inhibitors and cardiovascular toxicity. Lancet Oncol. 2018;19(9):e447–e4.
Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med. 2016;375(15):1457–67.
Suter TM, Ewer MS. Cancer drugs and the heart: importance and management. Eur Heart J. 2013;34(15):1102–11.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53(24):2231–47.
Lyon AR, Dent S, Stanway S, Earl H, Brezden-Masley C, Cohen-Solal A, et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the cardio-oncology study group of the heart failure association of the European society of cardiology in collaboration with the international cardio-oncology society. Eur J Heart Fail. 2020;22(11):1945–60.
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131(22):1981–8.
de Azambuja E, Ameye L, Diaz M, Vandenbossche S, Aftimos P, Bejarano Hernandez S, et al. Cardiac assessment of early breast cancer patients 18 years after treatment with cyclophosphamide-, methotrexate-, fluorouracil- or epirubicin-based chemotherapy. Eur J Cancer. 2015;51:2517–24.
Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacomi G, et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol. 2010;55(3):213–20.
Schettini F, Giuliano M, Lambertini M, Bartsch R, Pinato DJ, Onesti CE, et al. Anthracyclines strike back: rediscovering non-pegylated liposomal doxorubicin in current therapeutic scenarios of breast cancer. Cancers (Basel). 2021;13(17):4421.
Macedo AVS, Hajjar LA, Lyon AR, Nascimento BR, Putzu A, Rossi L, et al. Efficacy of dexrazoxane in preventing anthracycline cardiotoxicity in breast cancer. J Am Coll Cardiol. 2019;1(1):68–79.
Cuomo A, Rodolico A, Galdieri A, et al. Heart failure and cancer: mechanisms of old and new cardiotoxic drugs in cancer patients. Card Fail Rev. 2019;5(2):112–8.
Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389(10087):2415–29.
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin adjuvant (HERA) trial. Lancet. 2017;389(10075):1195–205.
Saura C, Oliveira M, Feng YH, Dai MS, Chen SW, Hurvitz SA, et al. Neratinib plus capecitabine versus lapatinib plus capecitabine in HER2-positive metastatic breast cancer previously treated with ≥ 2 HER2-directed regimens: phase III NALA trial. J Clin Oncol. 2020;38(27):3138–49.
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2020;382(7):597–609.
Cortes J, Kim SB, Chung WP, et al. Trastuzumab deruxtecan (T-DXd) vs trastuzumab emtansine (T-DM1) in patients (Pts) with HER2+ metastatic breast cancer (mBC): Results of the randomized phase III DESTINY-Breast03 study. Ann Oncol. 2021;32(suppl_5):S1283–346. https://doi.org/10.1016/annonc/annonc741.
Cote GM, Sawyer DB, Chabner BA. ERBB2 inhibition and heart failure. N Engl J Med. 2012;367:2150–3.
Goel S, Liu J, Guo H, Barry W, Bell R, Murray B, et al. Decline in left ventricular ejection fraction following anthracyclines predicts trastuzumab cardiotoxicity. JACC Heart Fail. 2019;7(9):795–804.
Ewer MS, Lippman SM. Type II chemotherapy-related cardiac dysfunction: time to recognize a new entity. J Clin Oncol. 2005;23:2900–2.
Chien KR. Herceptin and the heart—a molecular modifier of cardiac failure. N Engl J Med. 2006;354(8):789–90.
Timolati F, Ott D, Pentassuglia L, Giraud M‑N, Perriard J‑C, Suter TM, et al. Neuregulin‑1 beta attenuates doxorubicin-induced alterations of excitation contraction coupling and reduces oxidative stress in adult rat cardiomyocytes. J Mol Cell Cardiol. 2006;41:845–54.
Dempsey N, Rosenthal A, Dabas N, Kropotova Y, Lippman M, Bishopric NH. Trastuzumab-induced cardiotoxicity: a review of clinical risk factors, pharmacologic prevention, and cardiotoxicity of other HER2-directed therapies. Breast Cancer Res Treat. 2021;188(1):21–36.
Curigliano G, Lenihan D, Fradley M, Ganatra S, Barac A, Blaes A, et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann Oncol. 2020;31(2):171–90.
Goldhirsch A, Gelber RD, Piccart-Gebhart MJ, de Azambuja E, Procter M, Suter TM, et al. 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet. 2013;382(9897):1021–8.
de Azambuja E, Procter MJ, van Veldhuisen DJ, Agbor-Tarh D, Metzger-Filho O, Steinseifer J, et al. Trastuzumab-associated cardiac events at 8 years of median follow-up in the herceptin adjuvant trial (BIG 1‑01). J Clin Oncol. 2014;32:2159–65.
Seicean S, Seicean A, Alan N, Plana JC, Budd GT, Marwick TH. Cardioprotective effect of beta-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy: follow-up study of heart failure. Circ Heart Fail. 2013;6:420–6.
Guglin M, Krischer J, Tamura R, Fink A, Bello-Matricaria L, McCaskill-Stevens W, et al. Randomized trial of lisinopril versus carvedilol to prevent trastuzumab cardiotoxicity in patients with breast cancer. J Am Coll Cardiol. 2019;73(22):2859–68.
Santoro C, Esposito R, Lembo M, Sorrentino R, De Santo I, Luciano F, et al. Strain-oriented strategy for guiding cardioprotection initiation of breast cancer patients experiencing cardiac dysfunction. Eur Heart J Cardiovasc Imaging. 2019;20(12):1345–52.
Rushton M, Lima I, Tuna M, Johnson C, Ivars J, Pritchard K, et al. Impact of stopping trastuzumab in early breast cancer: a population-based study in Ontario, Canada. J Natl Cancer Inst. 2020;112(12):1222–30.
Lynce F, Barac A, Geng X, Dang C, Yu AF, Smith KL, et al. Prospective evaluation oft he cardiac safety of HER2-targeted therapies in patients with HER2-positive breast cancer and compromised heart function: the SAFE-HEaRt study. Breast Cancer Res Treat. 2019;175:595–603.
Khoury K, Lynce F, Barac A, Geng X, Dang C, Yu AF, et al. Long-term follow-up assessment of cardiac safety in SAFE-HEaRt, a clinical trial evaluating the use of HER2-targeted therapies in patients with breast cancer and compromised heart function. Breast Cancer Res Treat. 2021;185(3):863–8.
Leong DP, Cosman T, Alhussein MM, Tyagi NK, Karampatos S, Barron CC, et al. Safety of continuing trastuzumab despite mild cardiotoxicity. J Am Coll Cardiol. 2019;1:1–10.
Thavendiranathan P, Negishi T, Somerset E, Negishi K, Penicka M, Lemieux J, et al. Strain-guided management of potentially cardiotoxic cancer therapy. J Am Coll Cardiol. 2021;77(4):392–401.
Piccart-Gebhart M, Holmes E, Baselga J, de Azambuja E, Dueck AC, Viale G, et al. Adjuvant lapatinib and trastuzumab for early human epidermal growth factor receptor 2‑positive breast cancer: results from the randomized phase III adjuvant lapatinib and/or trastuzumab treatment optimization trial. J Clin Oncol. 2016;34:1034–42.
Dent SF, Morse A, Burnette S, Guha A, Moore H. Cardiovascular toxicity of novel HER2-targeted therapies in the treatment of breast cancer. Curr Oncol Rep. 2021;23(11):128.
Frey MK, Bergler-Klein J. Echocardiographic evaluation of patients undergoing cancer therapy. Eur Heart J Cardiovasc Imaging. 2021;22(4):375–82.
Addison D, Campbell CM, Guha A, Ghosh AK, Dent SF, Jneid H. Cardio-oncology in the era of the COVID-19 pandemic and beyond. J Am Heart Assoc. 2020;9(19):e17787.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Heck SL, Mecinaj A, Ree AH, Hoffmann P, Schulz-Menger J, Fagerland MW, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): extended follow-up of a 2×2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Circulation. 2021;143(25):2431–40.
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87.
Okwuosa TM, Morgans A, Rhee JW, Reding KW, Maliski S, Plana JC, et al. Impact of hormonal therapies for treatment of hormone-dependent cancers (breast and prostate) on the cardiovascular system: effects and modifications: a scientific statement from the American heart association. Circ Genom Precis Med. 2021;14(3):e82.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-updagger. Ann Oncol. 2019;30(8):1194–220.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71(4):618–29.
Quante AS, Ming C, Rottmann M, Engel J, Boeck S, Heinemann V, et al. Projections of cancer incidence and cancer-related deaths in Germany by 2020 and 2030. Cancer Med. 2016;5(9):2649–56.
Braithwaite RS, Chlebowski RT, Lau J, George S, Hess R, Col NF. Meta-analysis of vascular and neoplastic events associated with tamoxifen. J Gen Intern Med. 2003;18(11):937–47.
Decensi A, Maisonneuve P, Rotmensz N, Bettega D, Costa A, Sacchini V, et al. Effect of tamoxifen on venous thromboembolic events in a breast cancer prevention trial. Circulation. 2005;111(5):650–6.
Sund M, Garcia-Argibay M, Garmo H, Ahlgren J, Wennstig AK, Fredriksson I, et al. Aromatase inhibitors use and risk for cardiovascular disease in breast cancer patients: a population-based cohort study. Breast. 2021;59:157–64.
Barrett-Connor E, Mosca L, Collins P, Geiger MJ, Grady D, Kornitzer M, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355(2):125–37.
Ewer MS, Gluck S. A woman’s heart: the impact of adjuvant endocrine therapy on cardiovascular health. Cancer. 2009;115(9):1813–26.
Matthews A, Stanway S, Farmer RE, Strongman H, Thomas S, Lyon AR, et al. Long term adjuvant endocrine therapy and risk of cardiovascular disease in female breast cancer survivors: systematic review. BMJ. 2018;363:k3845.
Grouthier V, Lebrun-Vignes B, Glazer AM, Touraine P, Funck-Brentano C, Pariente A, et al. Increased long QT and torsade de pointes reporting on tamoxifen compared with aromatase inhibitors. Heart. 2018;104(22):1859–63.
Barber M, Nguyen LS, Wassermann J, Spano JP, Funck-Brentano C, Salem JE. Cardiac arrhythmia considerations of hormone cancer therapies. Cardiovasc Res. 2019;115(5):878–94.
Gupta D, Lee Chuy K, Yang JC, Bates M, Lombardo M, Steingart RM. Cardiovascular and metabolic effects of androgen-deprivation therapy for prostate cancer. J Oncol Pract. 2018;14(10):580–7.
Nguyen PL, Alibhai SM, Basaria S, D’Amico AV, Kantoff PW, Keating NL, et al. Adverse effects of androgen deprivation therapy and strategies to mitigate them. Eur Urol. 2015;67(5):825–36.
Hu JR, Duncan MS, Morgans AK, Brown JD, Meijers WC, Freiberg MS, et al. Cardiovascular effects of androgen deprivation therapy in prostate cancer: contemporary meta-analyses. Arterioscler Thromb Vasc Biol. 2020;40:e55–e64.
Haque R, UlcickasYood M, Xu X, Cassidy-Bushrow AE, Tsai HT, Keating NL, et al. Cardiovascular disease risk and androgen deprivation therapy in patients with localised prostate cancer: a prospective cohort study. Br J Cancer. 2017;117(8):1233–40.
Lopes RD, Higano CS, Slovin SF, Nelson AJ, Bigelow R, Sørensen PS, et al. Cardiovascular safety of degarelix versus leuprolide in patients with prostate cancer: the primary results of the PRONOUNCE randomized trial. Circulation. 2021;144(16):1295–307.
Dobbin SJH, Cameron AC, Petrie MC, Jones RJ, Touyz RM, Lang NN. Toxicity of cancer therapy: what the cardiologist needs to know about angiogenesis inhibitors. Heart. 2018;104:1995–2002.
Hahn VS, Zhang KW, Sun L, Narayan V, Lenihan DJ, Ky B. Heart failure with targeted cancer therapies: mechanisms and cardioprotection. Circ Res. 2021;128(10):1576–93.
Chaar M, Kamta J, Ait-Oudhia S. Mechanisms, monitoring, and management of tyrosine kinase inhibitors-associated cardiovascular toxicities. Onco Targets Ther. 2018;11:6227–37.
Touyz RM, Herrmann SMS, Herrmann J. Vascular toxicities with VEGF inhibitor therapies-focus on hypertension and arterial thrombotic events. J Am Soc Hypertens. 2018;12(6):409–25.
Wu MD, Moslehi JJ, Lindner JR. Arterial thrombotic complications of tyrosine kinase inhibitors. Arterioscler Thromb Vasc Biol. 2021;41(1):3–10.
Schmidinger M, Bergler-Klein J. Therapy management of cardiovascular adverse events in the context of targeted therapy for metastatic renal cell carcinoma. Int J Urol. 2012;19:796–804.
Sourdon J, Facchin C, Certain A, Viel T, Robin B, Lager F, et al. Sunitinib-induced cardiac hypertrophy and the endothelin axis. Theranostics. 2021;11(8):3830–8.
Hou W, Ding M, Li X, Zhou X, Zhu Q, Varela-Ramirez A, et al. Comparative evaluation of cardiovascular risks among nine FDA-approved VEGFR-TKIs in patients with solid tumors: a Bayesian network analysis of randomized controlled trials. J Cancer Res Clin Oncol. 2021;147(8):2407–20.
Alexandre J, Salem JE, Moslehi J, Sassier M, Ropert C, Cautela J, et al. Identification of anticancer drugs associated with atrial fibrillation: analysis of the WHO pharmacovigilance database. Eur Heart J Cardiovasc Pharmacother. 2021;7(4):312–20.
Salem JE, Manouchehri A, Bretagne M, Lebrun-Vignes B, Groarke JD, Johnson DB, et al. Cardiovascular toxicities associated with Ibrutinib. J Am Coll Cardiol. 2019;74(13):1667–78.
Bergler-Klein J. Real-life insight into ibrutinib cardiovascular events: defining the loose ends. J Am Coll Cardiol. 2019;74:1679–81.
Brown JR, Moslehi J, O’Brien S, Ghia P, Hillmen P, Cymbalista F, et al. Characterization of atrial fibrillation adverse events reported in ibrutinib randomized controlled registration trials. Haematologica. 2017;102(10):1796–805.
Guha A, Armanious M, Fradley MG. Update on cardio-oncology: novel cancer therapeutics and associated cardiotoxicities. Trends Cardiovasc Med. 2019;29:29–39.
Duran JM, Makarewich CA, Trappanese D, Gross P, Husain S, Dunn J, et al. Sorafenib cardiotoxicity increases mortality after myocardial infarction. Circ Res. 2014;114(11):1700–12.
Schneider C, Wallner M, Kolesnik E, Herbst V, Mächler H, Pichler M, et al. The anti-cancer multikinase inhibitor sorafenib impairs cardiac contractility by reducing phospholamban phosphorylation and sarcoplasmic calcium transients. Sci Rep. 2018;8(1):5295.
Rainer PP, Doleschal B, Kirk JA, Sivakumaran V, Saad Z, Groschner K, et al. Sunitinib causes dose-dependent negative functional effects on myocardium and cardiomyocytes. BJU Int. 2012;110(10):1455–62.
Sharma P, Allison JP. Immune checkpoint targeting in cancer therapy: toward combination strategies with curative potential. Cell. 2015;161(2):205–14.
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018;359(6382):1350–5.
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(1):23–34.
Steininger J, Gellrich FF, Schulz A, Westphal D, Beissert S, Meier F. Systemic therapy of metastatic melanoma: on the road to cure. Cancers (Basel). 2021;13(6):1430.
Borghaei H, Gettinger S, Vokes EE, Chow LQM, Burgio MA, de Castro Carpeno J, et al. Five-year outcomes from the randomized, phase III trials checkmate 017 and 057: nivolumab versus docetaxel in previously treated non-small-cell lung cancer. J Clin Oncol. 2021;39(7):723–33.
Johnson DB, Balko JM, Compton ML, Chalkias S, Gorham J, Xu Y, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749–55.
Moslehi JJ, Salem JE, Sosman JA, Lebrun-Vignes B, Johnson DB. Increased reporting of fatal immune checkpoint inhibitor-associated myocarditis. Lancet. 2018;391(10124):933.
Mahmood SS, Fradley MG, Cohen JV, Nohria A, Reynolds KL, Heinzerling LM, et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71:1755–64.
D’Souza M, Nielsen D, Svane IM, Iversen K, Rasmussen PV, Madelaire C, et al. The risk of cardiac events in patients receiving immune checkpoint inhibitors: a nationwide Danish study. Eur Heart J. 2021;42(16):1621–31.
Escudier M, Cautela J, Malissen N, Ancedy Y, Orabona M, Pinto J, et al. Clinical features, management, and outcomes of immune checkpoint inhibitor-related cardiotoxicity. Circulation. 2017;36:2085–7.
Palaskas N, Lopez-Mattei J, Durand JB, Iliescu C, Deswal A. Immune checkpoint inhibitor myocarditis: pathophysiological characteristics, diagnosis, and treatment. J Am Heart Assoc. 2020;9(2):e13757.
Hu JR, Florido R, Lipson EJ, Naidoo J, Ardehali R, Tocchetti CG, et al. Cardiovascular toxicities associated with immune checkpoint inhibitors. Cardiovasc Res. 2019;115(5):854–68.
Shalata W, Abu-Salman A, Steckbeck R, Mathew Jacob B, Massalha I, Yakobson A. Cardiac toxicity associated with immune checkpoint inhibitors: a systematic review. Cancers (Basel). 2021;13(20):5218.
Delombaerde D, Vervloet D, Franssen C, Croes L, Gremonprez F, Prenen H, et al. Clinical implications of isolated troponinemia following immune checkpoint inhibitor therapy. ESMO Open. 2021;6(4):100216.
Pathak R, Katel A, Massarelli E, Villaflor VM, Sun V, Salgia R. Immune checkpoint inhibitor-induced myocarditis with myositis/myasthenia gravis overlap syndrome: a systematic review of cases. Oncologist. 2021;26(12):1052–61.
Bonaca MP, Olenchock BA, Salem JE, Wiviott SD, Ederhy S, Cohen A, et al. Myocarditis in the setting of cancer therapeutics: proposed case definitions for emerging clinical syndromes in cardio-oncology. Circulation. 2019;140(2):80–91.
Thavendiranathan P, Zhang L, Zafar A, Drobni ZD, Mahmood SS, Cabral M, et al. Myocardial T1 and T2 mapping by magnetic resonance in patients with immune checkpoint inhibitor-associated Myocarditis. J Am Coll Cardiol. 2021;77(12):1503–16.
Zhang L, Awadalla M, Mahmood SS, Nohria A, Hassan MZO, Thuny F, et al. Cardiovascular magnetic resonance in immune checkpoint inhibitor-associated myocarditis. Eur Heart J. 2020;41(18):1733–43.
Palaskas NL, Segura A, Lelenwa L, Siddiqui BA, Subudhi SK, Lopez-Mattei J, et al. Immune checkpoint inhibitor myocarditis: elucidating the spectrum of disease through endomyocardial biopsy. Eur J Heart Fail. 2021;23(10):1725–35.
Salem JE, Manouchehri A, Moey M, et al. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018;19(12):1579–89.
Power JR, Alexandre J, Choudhary A, Ozbay B, Hayek S, Asnani A, et al. International ICI-myocarditis registry. Electrocardiographic manifestations of immune checkpoint inhibitor myocarditis. Circulation. 2021;144(18):1521–3.
Lehmann LH, Cautela J, Palaskas N, Baik AH, Meijers WC, Allenbach Y, et al. Clinical strategy for the diagnosis and treatment of immune checkpoint inhibitor-associated myocarditis: a narrative review. JAMA Cardiol. 2021;6(11):1329–37.
Brahmer JR, Lacchetti C, Schneider BJ, et al. National comprehensive cancer network. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. J Clin Oncol. 2018;36(17):1714–68.
Salem JE, Allenbach Y, Vozy A, Brechot N, Johnson DB, Moslehi JJ, et al. Abatacept for severe immune checkpoint inhibitor-associated myocarditis. N Engl J Med. 2019;380(24):2377–9.
Wei SC, Meijers WC, Axelrod ML, Anang NAAS, Screever EM, Wescott EC, et al. A genetic mouse model recapitulates immune checkpoint inhibitor–associated myocarditis and supports a mechanism-based therapeutic intervention. Cancer Discov. 2021;11:614–25.
Doms J, Prior JO, Peters S, Obeid M. Tocilizumab for refractory severe immune checkpoint inhibitor-associated myocarditis. Ann Oncol. 2020;31(9):1273–5.
Brammer JE, Braunstein Z, Katapadi A, Porter K, Biersmith M, Guha A, et al. Early toxicity and clinical outcomes after chimeric antigen receptor T‑cell (CAR-T) therapy for lymphoma. J Immunother Cancer. 2021;9(8):e2303.
Stein-Merlob AF, Rothberg MV, Ribas A, Yang EH. Cardiotoxicities of novel cancer immunotherapies. Heart. 2021;107(21):1694–703.
Goldman A, Maor E, Bomze D, Liu JE, Herrmann J, Fein J, et al. Adverse cardiovascular and pulmonary events associated with chimeric antigen receptor T‑cell therapy. J Am Coll Cardiol. 2021;78(18):1800–13.
Chang HM, Moudgil R, Scarabelli T, Okwuosa TM, Yeh ETH. Cardiovascular complications of cancer therapy: best practices in diagnosis, prevention, and management: part 1. J Am Coll Cardiol. 2017;70(20):2536–51.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
Zamorano JL, Gottfridsson C, Asteggiano R, Atar D, Badimon L, Bax JJ, et al. The cancer patient and cardiology. Eur J Heart Fail. 2020;22(12):2290–309.
Sara JD, Kaur J, Khodadadi R, Rehman M, Lobo R, Chakrabarti S, et al. 5‑fluorouracil and cardiotoxicity: a review. Ther Adv Med Oncol. 2018;10:1758835918780140.
Siegel DS, Dimopoulos MA, Ludwig H, Facon T, Goldschmidt H, Jakubowiak A, et al. Improvement in overall survival with carfilzomib, lenalidomide, and dexamethasone in patients with relapsed or refractory multiple myeloma. J Clin Oncol. 2018;36:728–34.
Grandin EW, Ky B, Cornell RF, Carver J, Lenihan DJ. Patterns of cardiac toxicity associated with irreversible proteasome inhibition in the treatment of multiple myeloma. J Card Fail. 2015;21:138–44.
Cornell RF, Ky B, Weiss BM, Dahm CN, Gupta DK, Du L, et al. Prospective study of cardiac events during proteasome inhibitor therapy for relapsed multiple myeloma. J Clin Oncol. 2019;37(22):1946–55.
Reneau JC, Asante D, van Houten H, Sangaralingham LR, Buadi FK, Lerman A, et al. Cardiotoxicity risk with bortezomib versus lenalidomide for treatment of multiple myeloma: a propensity matched study of 1,790 patients. Am J Hematol. 2017;92(2):E15–E7.
Kumar SK, Jacobus SJ, Cohen AD, Weiss M, Callander N, Singh AK, et al. Carfilzomib or bortezomib in combination with lenalidomide and dexamethasone for patients with newly diagnosed multiple myeloma without intention for immediate autologous stem-cell transplantation (ENDURANCE): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2020;21(10):1317–30.
Gevaert SA, Halvorsen S, Sinnaeve PR, Sambola A, Gulati G, Lancellotti P, et al. Evaluation and management of cancer patients presenting with acute cardiovascular disease: a consensus document of the acute cardiovascular care (ACVC) association and the ESC council of cardio-oncology-part 1: acute coronary syndromes and acute pericardial diseases. Eur Heart J Acute Cardiovasc Care. 2021;10(8):947–59.
Spring LM, Wander SA, Andre F, Moy B, Turner NC, Bardia A. Cyclin-dependent kinase 4 and 6 inhibitors for hormone receptor-positive breast cancer: past, present, and future. Lancet. 2020;395(10226):817–27.
Ball S, Swarup S, Sultan A, Thein KZ. Increased risk of cardiac conduction abnormalities with ribociclib in patients with metastatic breast cancer: a combined analysis of phase III randomized controlled trials. Hematol Oncol Stem Cell Ther. 2021;14(3):260–2.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Pituskin E, Mackey JR, Koshman S, Jassal D, Pitz M, Haykowsky MJ, et al. Multidisciplinary approach to novel therapies in cardio-oncology research (MANTICORE 101-breast): a randomized trial for the prevention of trastuzumab-associated cardiotoxicity. J Clin Oncol. 2017;35(8):870–7.
Gulati G, Heck SL, Ree AH, Hoffmann P, Schulz-Menger J, Fagerland MW, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37(21):1671–80.
Gregorietti V, Fernandez TL, Costa D, Chahla EO, Daniele AJ. Use of sacubitril/valsartan in patients with cardio toxicity and heart failure due to chemotherapy. Cardiooncology. 2020;6(1):24.
Frey MK, Arfsten H, Pavo N, Han E, Kastl S, Hülsmann M, et al. Sacubitril/valsartan is well tolerated in patients with longstanding heart failure and history of cancer and improves ventricular function: real-world data. Cardiooncology. 2021;7(1):35.
Bergler-Klein J. Cardiotoxicity—current recommendations of prevention and treatment. memo – Magazine of European Medical Oncology. 2022;15:67–71.
Jaworski C, Mariani JA, Wheeler G, Kaye DM. Cardiac complications of thoracic irradiation. J Am Coll Cardiol. 2013;61:2319–28.
Lancellotti P, Nkomo VT, Badano LP, Bergler-Klein J, Bogaert J, Davin L, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European association of cardiovascular imaging and the American society of echocardiography. J Am Soc Echocardiogr. 2013;26(9):1013–32.
Mitchell JD, Cehic DA, Morgia M, Bergrom C, Toohey J, Guerrero PA, et al. Cardiovascular manifestations from therapeutic radiation: a multidisciplinary expert consensus statement from the international cardio-oncology society. J Am Coll Cardiol. 2021;3(3):360–80.
van Nimwegen FA, Schaapveld M, Cutter DJ, Janus CP, Krol AD, Hauptmann M, et al. Radiation dose-response relationship for risk of coronary heart disease in survivors of Hodgkin lymphoma. J Clin Oncol. 2016;34(3):235–43.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–98.
Erven K, Jurcut R, Weltens C, Giusca S, Ector J, Wildiers H, et al. Acute radiation effects on cardiac function detected by strain rate imaging in breast cancer patients. Int J Radiat Oncol Biol Phys. 2011;79(5):1444–51.
Dunn AN, Donnellan E, Johnston DR, Alashi A, Reed GW, Jellis C, et al. Long-term outcomes of patients with mediastinal radiation-associated coronary artery disease undergoing coronary revascularization with percutaneous coronary intervention and coronary artery bypass grafting. Circulation. 2020;142(14):1399–401.
Cutter DJ, Schaapveld M, Darby SC, Hauptmann M, van Nimwegen FA, Krol AD, et al. Risk of valvular heart disease after treatment for Hodgkin lymphoma. J Natl Cancer Inst. 2015;107(4):djv8.
Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ, Allen AM, et al. Radiation dose-volume effects in the heart. Int J Radiat Oncol Biol Phys. 2010;76(3):S77–85.
Bergler-Klein J, Badr Eslam R, Schneider M, Frey M, Gyöngyösi M, Binder T. Radiation induced valve disease and cardiotoxicity induced heart failure is frequent. Heart. 2019;3(1):136–136.
Jurado JA, Bashir R, Burket MW. Radiation-induced peripheral artery disease. Catheter Cardiovasc Interv. 2008;72:563–8.
Leerink JM, de Baat EC, Feijen EAM, Bellersen L, van Dalen EC, Grotenhuis HB, et al. Cardiac disease in childhood cancer survivors: risk prediction, prevention, and surveillance: JACC cardiooncology state-of-the-art review. J Am Coll Cardiol. 2020;2(3):363–78.
Fidler MM, Reulen RC, Winter DL, Kelly J, Jenkinson HC, Skinner R, et al. Long term cause specific mortality among 34 489 five year survivors of childhood cancer in Great Britain: population based cohort study. BMJ. 2016;354:i4351.
Fidler MM, Reulen RC, Henson K, Kelly J, Cutter D, Levitt GA, et al. Population-based long-term cardiac-specific mortality among 34 489 five-year survivors of childhood cancer in great britain. Circulation. 2017;135(10):951–63.
DeFilipp Z, Duarte RF, Snowden JA, Majhail NS, Greenfield DM, Miranda JL, et al. Metabolic syndrome and cardiovascular disease following hematopoietic cell transplantation: screening and preventive practice recommendations from CIBMTR and EBMT. Bone Marrow Transplant. 2017;52(2):173–82.
Faber J, Wingerter A, Neu MA, Henninger N, Eckerle S, Münzel T, et al. Burden of cardiovascular risk factors and cardiovascular disease in childhood cancer survivors: data from the German CVSS-study. Eur Heart J. 2018;39(17):1555–62.
Gudmundsdottir T, Winther JF, de Fine Licht S, Bonnesen TG, Asdahl PH, Tryggvadottir L, et al. Cardiovascular disease in adult life after childhood cancer in Scandinavia: a population-based cohort study of 32,308 one-year survivors. Int J Cancer. 2015;137(5):1176–86.
Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine LS, Dwyer M, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the international late effects of childhood cancer guideline harmonization group. Lancet Oncol. 2015;16(3):e123–36.
van Dalen EC, Mulder RL, Suh E, Ehrhardt MJ, Aune GJ, Bardi E, et al. Coronary artery disease surveillance among childhood, adolescent and young adult cancer survivors: a systematic review and recommendations from the international late effects of childhood cancer guideline harmonization group. Eur J Cancer. 2021;156:127–37.
Leerink JM, Verkleij SJ, Feijen EAM, Mavinkurve-Groothuis AMC, Pourier MS, Ylanen K, et al. Biomarkers to diagnose ventricular dysfunction in childhood cancer survivors: a systematic review. Heart. 2019;105(3):210–6.
Dixon SB, Howell CR, Lu L, Plana JC, Joshi VM, Luepker RV, et al. Cardiac biomarkers and association with subsequent cardiomyopathy and mortality among adult survivors of childhood cancer: a report from the St. Jude lifetime cohort. Cancer. 2021;127(3):458–66.
Merkx R, Leerink JM, de Baat EC, Feijen EAM, Kok WEM, Mavinkurve-Groothuis AMC, et al. Asymptomatic systolic dysfunction on contemporary echocardiography in anthracycline-treated long-term childhood cancer survivors: a systematic review. J Cancer Surviv. 2021; https://doi.org/10.1007/s11764-021-01028-4.
Cheuk DK, Sieswerda E, van Dalen EC, Postma A, Kremer LC. Medical interventions for treating anthracycline-induced symptomatic and asymptomatic cardiotoxicity during and after treatment for childhood cancer. Cochrane Database Syst Rev. 2016;8:CD8011.
McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, et al. American society of clinical oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31(5):631–40.
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;8:CD8465.
Scott JM, Zabor EC, Schwitzer E, Koelwyn GJ, Adams SC, Nilsen TS, et al. Efficacy of exercise therapy on cardiorespiratory fitness in patients with cancer: a systematic review and meta-analysis. J Clin Oncol. 2018;36(22):2297–305.
Okwuosa TM, Ray RM, Palomo A, Foraker RE, Johnson L, Paskett ED, et al. Pre-diagnosis exercise and cardiovascular events in primary breast cancer: women’s health initiative. J Am Coll Cardiol. 2019;1(1):41–50.
Scott JM, Nilsen TS, Gupta D, Jones LW. Exercise therapy and cardiovascular toxicity in cancer. Circulation. 2018;137(11):1176–91.
Ellahham SH. Exercise before, during, and after cancer therapy. Expert analysis, American college of cardiology. https://www.acc.org/latest-in-cardiology/articles/2019/12/04/08/22/exercise-before-during-and-after-cancer-therapy. Accessed 22 Dec 2021.
Gilchrist SC, Barac A, Ades PA, Alfano CM, Franklin BA, Jones LW, et al. Cardio-oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American heart association. Circulation. 2019;139(21):e997–e1012.
Díaz-Balboa E, González-Salvado V, Rodríguez-Romero B, Martínez-Monzonís A, Pedreira-Pérez M, Palacios-Ozores P, et al. A randomized trial to evaluate the impact of exercise-based cardiac rehabilitation for the prevention of chemotherapy-induced cardiotoxicity in patients with breast cancer: ONCORE study protocol. BMC Cardiovasc Disord. 2021;21(1):165.
Ameri P, Canepa M, Anker MS, Belenkov Y, Bergler-Klein J, Cohen-Solal A, et al. Cancer diagnosis in patients with heart failure: epidemiology, clinical implications and gaps in knowledge. Eur J Heart Fail. 2018;20(5):879–87.
Lancellotti P, Suter TM, López-Fernández T, Galderisi M, Lyon AR, Van der Meer P, et al. Cardio-oncology services: rationale, organization, and implementation. Eur Heart J. 2019;40(22):1756–63.
European Society of Cardiology. Cardio-oncology in Austria. 2022. https://www.escardio.org/Councils/council-of-cardio-oncology/cardio-oncology-in-austria. Accessed 22 Dec 2021.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Bergler-Klein, P.P. Rainer, M. Wallner, M.-M. Zaruba, J. Dörler, A. Böhmer, T. Buchacher, M. Frey, C. Adlbrecht, R. Bartsch, M. Gyöngyösi and U.-M. Fürst declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bergler-Klein, J., Rainer, P.P., Wallner, M. et al. Cardio-oncology in Austria: cardiotoxicity and surveillance of anti-cancer therapies. Wien Klin Wochenschr 134, 654–674 (2022). https://doi.org/10.1007/s00508-022-02031-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-022-02031-0