Summary
Objective
To examine the association between third trimester cervical length (CL) measurement and duration of the first stage of labor.
Methods
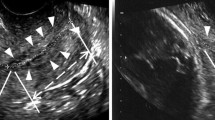
This prospective cohort study included women with a singleton pregnancy who had routine CL measurements taken by transvaginal ultrasonography between 37 and 39 weeks gestation. Subjective duration of the first stage of labor was defined as the duration of contractions that the women subjectively had from the onset of regular contractions to full effacement of the cervix. Objective duration of first stage of labor was defined as 3 cm cervical dilation independent of cervical effacement until full effacement of the cervix. Associations between variables were analyzed using nonparametric correlations coefficients. A model relating the duration of labor to predictors was built using linear regression.
Results
In this analysis a total of 129 women were included. There was no significant correlation between CL and subjective duration of labor (ρ = −0.037, p = 0.695); however, a reduction in CL increased the objective duration of the first stage of labor (ρ = −0.269, p = 0.013). In univariate analysis parity (p = 0.018), hypertensive disorders (p = 0.013) and induction of labor (p = 0.022) were significantly associated with subjective duration of the first stage of labor.
Conclusion
A long cervix in the third trimester is not associated with a prolonged first stage of labor. Induction of labor and multiparity were associated with a shorter first stage of labor while hypertension was associated with a longer duration of labor.


Similar content being viewed by others
References
Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016;21:74–9.
Parry S, Strauss JF 3rd. Premature rupture of the fetal membranes. N Engl J Med. 1998;338:663–70.
Mahendroo M. Cervical remodeling in term and preterm birth: Insights from an animal model. Reproduction. 2012;143:429–38.
Mella MT, Berghella V. Prediction of preterm birth: Cervical sonography. Semin Perinatol. 2009;33:317–24.
Silver RM. Implications of the first Cesarean: Perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol. 2012;36:315–23.
Meijer-Hoogeveen M, Van Holsbeke C, Van Der Tweel I, et al. Sonographic longitudinal cervical length measurements in nulliparous women at term: Prediction of spontaneous onset of labor. Ultrasound Obstet Gynecol. 2008;32:652–6.
Saccone G, Simonetti B, Berghella V. Transvaginal ultrasound cervical length for prediction of spontaneous labour at term: A systematic review and meta-analysis. BJOG. 2016;123:16–22.
Mukherji J, Bhadra A, Ghosh SK, et al. Cervical length measurement in nulliparous women at term by ultrasound & its relationship to spontaneous onset of labour. Indian J Med Res. 2017;146:498–504.
Miller ES, Sakowicz A, Grobman WA. Association between second-trimester cervical length and primary Cesarean delivery. Obstet Gynecol. 2013;122:863–7.
Smith GC, Celik E, To M, et al. Cervical length at mid-pregnancy and the risk of primary Cesarean delivery. N Engl J Med. 2008;358:1346–53.
Tolaymat LL, Gonzalez-Quintero VH, Sanchez-Ramos L, et al. Cervical length and the risk of spontaneous labor at term. J Perinatol. 2007;27:749–53.
Pereira S, Frick AP, Poon LC, et al. Successful induction of labor: Prediction by preinduction cervical length, angle of progression and cervical elastography. Ultrasound Obstet Gynecol. 2014;44:468–75.
Timmons B, Akins M, Mahendroo M. Cervical remodeling during pregnancy and parturition. Trends Endocrinol Metab. 2010;21:353–61.
Vink J, Mourad M. The pathophysiology of human premature cervical remodeling resulting in spontaneous preterm birth: Where are we now? Semin Perinatol. 2017;41:427–37.
Hanley GE, Munro S, Greyson D, et al. Diagnosing onset of labor: A systematic review of definitions in the research literature. BMC Pregnancy Childbirth. 2016;16:71.
AWMF. Vorgehen bei Terminüberschreitung und Übertragung. 2014. https://www.awmf.org/leitlinien/detail/ll/015-065.html, in Überarbeitung, gültig bis 27.02.2019.
van der Ven AJ, van Os MA, Kleinrouweler CE, et al. Midpregnancy cervical length in nulliparous women and its association with postterm delivery and Intrapartum Cesarean delivery. Am J Perinatol. 2016;33:40–6.
Cubal A, Carvalho J, Ferreira MJ, et al. Value of Bishop score and ultrasound cervical length measurement in the prediction of Cesarean delivery. J Obstet Gynaecol Res. 2013;39:1391–6.
Rane SM, Guirgis RR, Higgins B, et al. Models for the prediction of successful induction of labor based on pre-induction sonographic measurement of cervical length. J Matern Fetal Neonatal Med. 2005;17:315–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G. Léhner, P. Reif, A. Avian, M. Kollmann, I.-C. Lakovschek, U. Lang, and D. Ulrich declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Léhner, G., Reif, P., Avian, A. et al. Does third trimester cervical length predict duration of first stage of labor?. Wien Klin Wochenschr 131, 468–474 (2019). https://doi.org/10.1007/s00508-019-1527-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-019-1527-0