Summary
Background and objectives
The aim of this retrospective study was to analyze differences in the initial hemodynamic assessment and its impact on the treatment in patients aged 80 years or older compared to younger patients during the first 6 h after admission to the medical intensive care unit (ICU).
Results
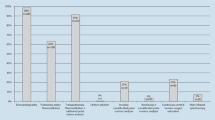
We analyzed 615 consecutive patients admitted to the medical ICU of which 124 (20%) were aged 80 years or more. The older group had a significantly higher acute physiology and chronic health evaluation (APACHE II) score, an overall mortality in the ICU and a presence of pre-existing cardiac disease. Both groups did not differ in the presence of shock and shock types on admission. In 57% of older and in 56% of younger patients, transthoracic echocardiography was performed with a higher therapeutic impact in the older patients. Transesophageal echocardiography was performed in 3% of the patients in both groups for specific diagnostic problems. Early reassessment with transthoracic echocardiography was necessary in 5% of the older and in 6% of the younger patients and resulted in a change of the treatment in one third of the patients. Continuous invasive hemodynamic monitoring was used in 11% of the older and in 10% of the younger patients and resulted in a therapeutic change in 71% of the older and in 64% of the younger patients.
Conclusion
Patients aged 80 years or older represent 20% of all admissions to the medical ICU. Once admitted the older patients were similarly hemodynamically assessed as the younger ones with a similar impact on the treatment.


Similar content being viewed by others
Abbreviations
- CCO:
-
Continuous cardiac output
- CO:
-
Cardiac output
- CVC:
-
Central venous catheter
- CVP:
-
Central venous pressure
- EVLW:
-
Extravascular lung water
- GEDV:
-
Global end-diastolic volume
- ICU:
-
Intensive care unit
- ITBV:
-
Intrathoracic blood volume
- IVC:
-
Inferior vena cava
- PAC:
-
Pulmonary artery catheter
- PAOP:
-
Pulmonary artery occlusion pressure
- PiCCO:
-
Pulse-induced continuous cardiac output
- LVEF:
-
Left ventricular ejection fraction
- ScvO2 :
-
Central venous oxygen saturation
- SvO2 :
-
Mixed venous oxygen saturation
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
- VTI:
-
Velocity time integral
References
Bose EL, Hravnak M, Pinsky MR. The interface between monitoring and physiology at the bedside. Crit Care Clin. 2015;31:1–24.
Sevransky J. Clinical assessment of hemodynamically unstable patients. Curr Opin Crit Care. 2009;15:234–8.
AzuRea group, Muller L, Bobbia X, Toumi M, et al. Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care. 2012;16:R188.
Osman D, Ridel C, Ray P, Monnet X, ANguel N, Richard C, Teboul JL. Cardiac filling pressures are not appropriate to predict hemodynamic support to volume challege. Crit Care Med. 2007;35:64–8.
Bakker J, Nijsten MWN, Jansen TC. Clinical use of lactate monitoring in critically ill patients. Ann Intensive Care. 2013;3:12.
Reinhart K, Kuhn HJ, Hartog C, Bredle DL. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30:1572–8.
Alhashemi JA, Cecconi M, Hofer C. Cardiac output monitoring: an integrative perspective. Crit Care. 2011;15:214.
Funcke S, Sander M, Goepfert SM, et al. Practice of hemodynamic monitoring and management in German, Austrian, and Swiss intensive care unit: the multicenter cross-sectional ICU-CardioMan Study. Ann Intensive Care. 2016;6:49–58.
Cecconi M, Hofer C, Teboul JL, et al. Fluid challenges in intensive care: the FENICE study A global inception cohort study. Intensive Care Med. 2015;41:1529–37.
Garrouste-Orgeas M, Boumendil A, Pateron D, Aergerter P, Somme D, Simon T, Guidet B. Selection of intensive care unit admission criteria for patients aged 80 years and over and compliance of emergency and intensive care unit physicians with the selected criteria: an observational, multicenter, prospective study. Crit Care Med. 2009;37(11):2919–28.
Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92.
Lerolle N, Trinquart L, Bornstain C, et al. Increased intensity of reatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med. 2010;38:59–64.
Cecconi M, De Backer D, Antonelli M, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–815.
Ihra GC, Lehberger J, Hochrieser H, et al. Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med. 2012;38:620–6.
Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care. 2011;1:29–36.
Sprung CL, Artigas A, Kesecioglu J, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: intensive care benefit for the elderly. Crit Care Med. 2012;40:132–8.
Brunner-Ziegler S, Heinze G, Ryffel M, Kompatscher M, Slany J, Valentin A. “Oldest old” patients in intensive care: prognosis and therapeutic activity. Wien Klin Wochenschr. 2007;119:14–9.
Becker S, Müller J, de Heer G, Braune S, Fuhrmann V, Kluge S. Clinical characteristics and outcome of very elderly patients ≥90 years in intensive care: a retrospective observational study. Ann Intensive Care. 2015;5:53–61.
De Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, de Jonge E. Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc. 2008;56:816–22.
Dawson NV, Connors AF, Speroff T, Kemka A, Shaw P, Arkes HR. Hemodynamic assessment in managing the critically ill: Is physician confidence warranted? Med Decis Making. 1993;13:258–66.
Joseph MX, Disney PJ, Da Costa R, Hutchison SJ. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest. 2004;126:1592–7.
Poelaert JI, Trouerbach J, De Buyzere M, Everaert J, Colardyn FA. Evaluation of transesophageal echocardiography as a diagnostic and therapeutic aid in a critical care setting. Chest. 1995;107:774–9.
Fuchs JB, Goerge G, Morschel C, Bruch C, Erbel R. Wert der echocardiography auf einer algemeininternistischen intensivstation. Intensivmed Notfallmed. 1997;34:549–55.
Manasia A, Cucu D, Oropello J, DelGiudice R, Hufanda J, Benjamin E. Clinical impact of early goal-directed echocardiography in shock patients performed by non-cardiologist intensivists free to view. Chest. 2005;128:222.
De Backer D. Ultrasonic evaluation of the heart. Curr Opin Crit Care. 2014;20:309–3014.
Takala J, Roukonen E, Tenhunen JJ, Parviainen I, Jakob SM. Early non-invasive cardiac output monitoring in hemodynamically unstable patients: A multi-center randomized controlled trial. Crit Care. 2011;15:R148.
Cecconi M, Bennett D. Should we use early less invasive hemodynamic monitoring in unstable ICU patients? Crit Care. 2011;15:173–4.
Marx G, Reinhart K. Venous oximetry. Curr Opin Crit Care. 2006;12:263–8.
Hofer CK, Cecconi M, Marx G, della Roca G. Minimally invasive hemodynamic monitoring. Eur J Anesthesiol. 2009;26:996–1002.
Shah MR, Hasselblad V, Stevenson LW, et al. Impact of the pulmonary artery catheter in critically ill patients. JAMA. 2005;294:1664–70.
Chittock DR, Dhingra VK, Ronco JJ, et al. Severity of illness and risk of death associated with pulmonary artery catheter use. Crit Care Med. 2004;32:911–5.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Tánczos K, Németh M, Molnár Z. The Multimodal concept of hemodynamic stabilization. Front Public Health. 2014;2:34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G. Voga and L. Gabršček-Parežnik declare that they have no competing interests.
Additional information
Author´s contribution G. Voga prepared the manuscript; L. Gabršček-Parežnik analyzed and collected the data and revised the manuscript.
Rights and permissions
About this article
Cite this article
Voga, G., Gabršček-Parežnik, L. Early hemodynamic assessment and treatment of elderly patients in the medical ICU. Wien Klin Wochenschr 128 (Suppl 7), 505–511 (2016). https://doi.org/10.1007/s00508-016-1131-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-016-1131-5