Abstract
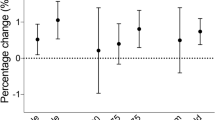
The health effects of air pollution have become a major public health problem. Studies on the relationship between short-term exposure to air pollutants and upper respiratory tract infection (URTI) related clinic visits and expenditures were scarce. From January 1, 2019, to December 31, 2021, we included all the URTI cases that turned to 11 public hospitals in Kunshan, and summarized individual medical cost. Daily meteorological factors and 24-h mean concentrations of four common air pollutants, including particulate matter with an aerodynamic diameter less than 2.5 μm (PM2.5) and 10 μm (PM10), sulfur dioxide (SO2), and nitrogen dioxide (NO2), were consecutively recorded. Generalized additive regression model was adopted to quantify the associations between each air pollutant and the daily clinic visits of URTI cases. We further calculated attributable number (AN) and attributable fraction, and performed sensitivity analysis by gender, age, and season. A total of 934,180 cases were retrieved during the study period. PM2.5, PM10, SO2, and NO2 showed significant associations with hospital visits and expenditures due to URTI. Relative risks for them were 1.065 (95% confidence interval [CI] 1.055, 1.076), 1.045 (95% CI 1.037, 1.052), 1.098 (95% CI 1.038, 1.163), and 1.098 (95% CI 1.085, 1.111) on lag 0–5 days, respectively. Thirty-one thousand four hundred fifty-five (95% CI 27,457, 35,436) cases could be ascribed to increased NO2 and accounted for 3.37% (95% CI 2.94%, 3.79%) of all clinic visits. Sensitivity analyses indicated that the effects of air pollution were generally consistent for male and female. PM2.5, PM10, and NO2 had stronger associations among people aged ≤ 18 years, followed by those aged 19–64 years and ≥ 65 years. The association strengths of air pollution varied seasonally. Short-term exposure to ambient air pollutants had significant associations with clinic visits and expenditures owing to URTI. Children and adolescents appeared to be more susceptible to adverse health effects of air pollution. NO2 may be a priority when formulating pollution control measures.


Similar content being viewed by others
Data availability
Data will be made available on request.
References
Bhatnagar A (2022) Cardiovascular effects of particulate air pollution. Annu Rev Med 73:393–406
Bramley TJ, Lerner D, Sarnes M (2002) Productivity losses related to the common cold. Am Coll Occup Environ Med 44:822–829
Cao D, Zheng D, Qian ZM, Shen H, Liu Y, Liu Q, Sun J, Zhang S, Jiao G, Yang X, Vaughn MG, Wang C, Zhang X, Lin H (2022) Ambient sulfur dioxide and hospital expenditures and length of hospital stay for respiratory diseases: a multicity study in China. Ecotoxicol Environ Saf 229:113082
Chang Q, Liu S, Chen Z, Zu B, Zhang H (2020) Association between air pollutants and outpatient and emergency hospital visits for childhood asthma in Shenyang city of China. Int J Biometeorol 64:1539–1548
Chang Q, Zhang H, Zhao Y (2020) Ambient air pollution and daily hospital admissions for respiratory system-related diseases in a heavy polluted city in Northeast China. Environ Sci Pollut Res Int 27:10055–10064
Chen R, Chu C, Tan J, Cao J, Song W, Xu X, Jiang C, Ma W, Yang C, Chen B, Gui Y, Kan H (2010) Ambient air pollution and hospital admission in Shanghai, China. J Hazard Mater 181:234–240
Cheng J, Su H, Xu Z (2021) Intraday effects of outdoor air pollution on acute upper and lower respiratory infections in Australian children. Environ Pollut 268:115698
Clougherty JE (2010) A growing role for gender analysis in air pollution epidemiology. Environ Health Perspect 118:167–176
Feng S, Gao D, Liao F, Zhou F, Wang X (2016) The health effects of ambient PM2.5 and potential mechanisms. Ecotoxicol Environ Saf 128:67–74
Gasparrini A, Armstrong B, Kovats S, Wilkinson P (2012) The effect of high temperatures on cause-specific mortality in England and Wales. Occup Environ Med 69:56–61
Ghozikali MG, Mosaferi M, Safari GH, Jaafari J (2015) Effect of exposure to O3, NO2, and SO2 on chronic obstructive pulmonary disease hospitalizations in Tabriz. Iran Environ Sci Pollut Res Int 22:2817–2823
Giannossa LC, Cesari D, Merico E, Dinoi A, Mangone A, Guascito MR, Contini D (2022) Inter-annual variability of source contributions to PM(10), PM(2.5), and oxidative potential in an urban background site in the central mediterranean. J Environ Manage 319:115752
Guarnieri M, Balmes JR (2014) Outdoor air pollution and asthma. Lancet 383:1581–1592
Guascito MR, Lionetto MG, Mazzotta F, Conte M, Giordano ME, Caricato R, De Bartolomeo AR, Dinoi A, Cesari D, Merico E, Mazzotta L, Contini D (2023) Characterisation of the correlations between oxidative potential and in vitro biological effects of PM(10) at three sites in the central Mediterranean. J Hazard Mater 448:130872
Huang ZH, Liu XY, Zhao T, Jiao KZ, Ma XX, Ren Z, Qiu YF, Liao JL, Ma L (2022) Short-term effects of air pollution on respiratory diseases among young children in Wuhan city, China. World J Pediatr 18:333–342
Jain N, Lodha R, Kabra SK (2001) Upper respiratory tract infections. Indian J Pediatr 68:1135–1138
Kawano A, Kim Y, Meas M, Sokal-Gutierrez K (2022) Association between satellite-detected tropospheric nitrogen dioxide and acute respiratory infections in children under age five in Senegal: spatio-temporal analysis. BMC Public Health 22:178
Kim K-H, Kabir E, Kabir S (2015) A review on the human health impact of airborne particulate matter. Environ Int 74:136–143
King D, Mitchell B, Williams CP, Spurling GK (2015) Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev 2015:CD006821
Li YR, Xiao CC, Li J, Tang J, Geng XY, Cui LJ, Zhai JX (2018) Association between air pollution and upper respiratory tract infection in hospital outpatients aged 0–14 years in Hefei, China: a time series study. Public Health 156:92–100
Li Y, Sun J, Lei R, Zheng J, Tian X, Xue B, Luo B (2023) The interactive effects between drought and air pollutants on children’s upper respiratory tract infection: a time-series analysis in Gansu, China. Int J Environ Res Public Health 20:1959
Liu Y, Wang Y, Dong J, Wang J, Bao H, Zhai G (2022) Association between air pollution and emergency department visits for upper respiratory tract infection in Lanzhou, China. Environ Sci Pollut Res Int 29:28816–28828
Münzel T, Gori T, Al-Kindi S, Deanfield J, Lelieveld J, Daiber A, Rajagopalan S (2018) Effects of gaseous and solid constituents of air pollution on endothelial function. Eur Heart J 39:3543–3550
Murray CJL et al (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396:1223–1249
Nhung NTT, Schindler C, Dien TM, Probst-Hensch N, Perez L, Kunzli N (2018) Acute effects of ambient air pollution on lower respiratory infections in Hanoi children: an eight-year time series study. Environ Int 110:139–148
Rebuli ME, Speen AM, Martin EM, Addo KA, Pawlak EA, Glista-Baker E, Robinette C, Zhou H, Noah TL, Jaspers I (2019) Wood smoke exposure alters human inflammatory responses to viral infection in a sex-specific manner. A randomized, placebo-controlled study. Am J Respir Crit Care Med 199:996–1007
Schuster JE, Williams JV (2018) Emerging respiratory viruses in children. Infect Dis Clin North Am 32:65–74
Shin S, Bai L, Burnett RT, Kwong JC, Hystad P, van Donkelaar A, Lavigne E, Weichenthal S, Copes R, Martin RV, Kopp A, Chen H (2021) Air pollution as a risk factor for incident chronic obstructive pulmonary disease and asthma. A 15-year population-based cohort study. Am J Respir Crit Care Med 203:1138–1148
Sierra-Vargas MP, Teran LM (2012) Air pollution: impact and prevention. Respirology 17:1031–1038
Suryadhi MAH, Abudureyimu K, Kashima S, Yorifuji T (2020) Nitrogen dioxide and acute respiratory tract infections in children in Indonesia. Arch Environ Occup Health 75:274–280
Tian Y, Liu H, Wu Y, Si Y, Song J, Cao Y, Li M, Wu Y, Wang X, Chen L, Wei C, Gao P, Hu Y (2019) Association between ambient fine particulate pollution and hospital admissions for cause specific cardiovascular disease: time series study in 184 major Chinese cities. BMJ 367:l6572
Xie Y, Li Z, Zhong H, Feng XL, Lu P, Xu Z, Guo T, Si Y, Wang J, Chen L, Wei C, Deng F, Baccarelli AA, Zheng Z, Guo X, Wu S (2021) Short-term ambient particulate air pollution and hospitalization expenditures of cause-specific cardiorespiratory diseases in China: a multicity analysis. Lancet Reg Health West Pac 15:100232
Xu H, Liu Y, Wang J, Jin X (2023) Short-term effects of ambient air pollution on emergency department visits for urolithiasis: a time-series study in Wuhan. China Front Public Health 11:1091672
Yao M, Wu G, Zhao X, Zhang J (2020) Estimating health burden and economic loss attributable to short-term exposure to multiple air pollutants in China. Environ Res 183:109184
Zhang F, Zhang H, Wu C, Zhang M, Feng H, Li D, Zhu W (2021) Acute effects of ambient air pollution on clinic visits of college students for upper respiratory tract infection in Wuhan, China. Environ Sci Pollut Res Int 28:29820–29830
Zheng P-w, Wang J-b, Zhang Z-y, Shen P, Chai P-f, Li D, Jin M-j, Tang M-L, Lu H-c, Lin H-b, Chen K (2017) Air pollution and hospital visits for acute upper and lower respiratory infections among children in Ningbo, China: a time-series analysis. Environ Sci Pollut Res 24:18860–18869
Ziou M, Tham R, Wheeler AJ, Zosky GR, Stephens N, Johnston FH (2022) Outdoor particulate matter exposure and upper respiratory tract infections in children and adolescents: a systematic review and meta-analysis. Environ Res 210:112969
Author information
Authors and Affiliations
Contributions
Study design: H. W., G. Q., J. S., K. Z.; data collection: W. L., Y. C., K. F., Y. S., H. R., X. H., Y. F., W. Z.; data analyses: H. W., K. Z.; results visualization: K. Z.; results interpretations: all authors; manuscript writing: K. Z., H. W.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors approved the final version of this manuscript and consent to publish.
Conflict of interest
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Qian, G., Shi, J. et al. Association between short-term exposure to ambient air pollution and upper respiratory tract infection in Kunshan. Int J Biometeorol 68, 189–197 (2024). https://doi.org/10.1007/s00484-023-02582-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-023-02582-5