Abstract
Background
Acute kidney injury (AKI) is common in children with sepsis, chronic kidney disease, poisoning or other conditions. Wasp stings are recognized as an important etiology. Several retrospective studies have investigated AKI after wasp stings in adults, but research on children remains limited.
Methods
The study included 48 children with multiple organ dysfunction syndrome after wasp stings. Demographic data, clinical manifestations, laboratory findings, management and clinical outcomes were collected, and analyzed to identify early indicators or risk factors for AKI.
Results
20 children (41.7%) developed AKI, and 28 (58.3%) did not. Serum creatine levels elevated mostly within 24 h from stings in children with AKI (16/20, 80%). Compared with non-AKI group, AKI group exhibited more cases with cola-colored urine, jaundice, and had higher sting numbers/body surface area (BSA) and higher revised sequential organ failure assessment scores (rSOFA) as well as higher levels of C-reactive protein (CRP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), lactate dehydrogenase (LDH), troponin (cTnI), creatine kinase (CK), and longer prothrombin time (PT). Both univariable and multivariable logistic regression analysis identified cola-colored urine as a potential early risk factor for AKI.
Conclusions
The AKI group exhibited higher sting numbers/BSA, higher levels of CRP, ALT, AST, TBIL, LDH, cTnI, and CK, as well as longer PT (p < 0.05). Our findings also suggest that cola-colored urine may serve as an early indicator or potential risk factor for AKI after wasp stings in children, which is very easy to identify for first aiders or pediatricians.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is common in children in nephrology departments and intensive care units (ICU), often resulting from infection, cardiovascular diseases, hypovolemia or other conditions. Wasp stings are also recognized as an important cause of AKI. Studies have shown that wasp stings are a growing public health problem worldwide with the global climate change, particularly in countries in Asia and Latin America, ever since the first report by Sitprijafrs & Boonpucknavigin, 1972 [1]. Zhang et al. reported a series of wasp sting cases in adults, revealing a mortality rate of 9.3%, and a rate of 10.7% progressing to chronic kidney disease (CKD) [2]. Dhanapriya et al. reported 11 cases with wasp sting-induced AKI in adults from India [3]. Xie et al. contributed the largest amount of data with wasp stings and concluded that the occurrence of AKI in wasp stings was 21.0%, based on a series of 1091 cases [4].
The mechanisms of wasp sting-induced AKI include direct venom toxicity to the kidney, renal tubular damage, obstruction by hemoglobulin and myoglobin or secondary inflammation induced by wasp-stings. In clinical practice, nephrologists are concerned about the risk factors for AKI induced by wasp stings, as timely treatment can make the prognosis completely different. However, the few studies addressing this issue are concerning adults. In a retrospective study of 508 adult patients with wasp stings, Tang et al. found several independent risk factors for AKI: the number of stings, aspartate aminotransferase (AST) > 147 U/L, lactate dehydrogenase (LDH) > 477 U/L, time from stings to admission > 12 h, and activated partial thromboplastin time (APTT) > 49 s [5]. In addition, Yuan suggested that elevated leukocytes, high myoglobin and high urinary monocyte chemotactic protein-1 (MCP-1) were independent risk factors for AKI following wasp stings [6]. For pediatricians, we are eager to obtain the relevant data focused on children. But so far, information about the risk factors of AKI in children with wasp stings is still lacking.
Outcomes vary according to the severity, ranging from complete recovery, to chronic kidney disease, to death. Vikrant et al. reported 10 deaths among 35 patients (10/35, 28.6%) due to acute respiratory distress syndrome (ARDS), massive bleeding, metabolic causes and stroke [7]. Zhang et al. reported 7 deaths among 75 patients (mortality rate 9.3%), 8 patients (10.7%) progressing to CKD, and 60 patients achieving complete recovery [2]. The situation in children still needs to be elucidated.
This study retrospectively analyzed the clinical data of 48 children who experienced severe wasp stings and developed multiple organ dysfunction syndrome (MODS). The aim was to identify risk factors for AKI, providing early predictors of AKI for pediatricians and nephrologists. We hypothesized that children with wasp stings might exhibit unique characteristics. As MODS itself was related to AKI and might be considered as a confounding factor, we just included the cases with MODS in conducting a stratified analysis. Thus, we focused solely on the children with MODS, aiming to obtain more accurate risk factors through this management strategy.
Methods
Patients
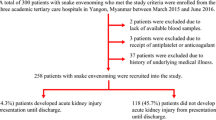
This retrospective cohort study initially collected data of wasp or bee sting cases in the Pediatric nephrology department of West China Second Hospital of Sichuan University from January 2014 to January 2022. Yet, the cases involving bee stings were excluded because bee venom is much less toxic than wasp venom, thus we focused on the cases with wasp stings. Eventually only the children with severe wasp stings (defined as cases with MODS) were included. The study finally included 48 cases, categorized into two groups: the AKI group and the non-AKI group (Fig. 1).
This research was in accordance with the Medical Ethics Committee of West China Second Hospital of Sichuan University and complied with the 1964 Helsinki Declaration and its subsequent amendments.
Definition of AKI in children
The diagnosis of AKI complied with Kidney Disease Improving Global Outcomes (KDIGO) guidelines (2012). KDIGO guidelines define AKI as a state with abnormal structure or function of the kidney, characterized by a sudden decline in kidney function. Specifically, AKI can be identified by an increase in serum creatinine of ≥ 0.3 mg/dl (> 26.5 μmol/L) within 48 h, an increase in serum creatinine levels ≥ 1.5 times the baseline within 7 days, or a urine output of < 0.5 ml/(kg.h) for a duration of 6 h. In our department, not all children had indwelling urethral catheters, thus it was hard for us to obtain real-time urine output. As such, serum creatinine levels ≥ 1.5 times baseline was chosen as the criterion for AKI. For a child with known baseline creatinine values within the last three months, we considered the patient’s lowest creatinine value as the baseline. However, for patients with unknown baseline values, we considered the lowest creatinine value during hospitalization or normal value from children with the same body weight as the baseline.
Clinical manifestations
Demographic data, including age, gender, body weight, and blood pressure (both systolic blood pressure (SBP) and diastolic blood pressure (DBP)) were collected. Clinical manifestations such as cola-colored urine, vomiting, fatigue, lethargy, jaundice, headache, dizziness, fever, dyspnea, edema, irritability, wheal, coma, convulsion, anorexia, and abdominal pain were recorded. Hypertension was assessed according to the Guideline for Screening and Management of High Blood Pressure in Children and Adolescents [8]. Hypotension in SBP was defined as follows: 1 ~ 12 months < 70 mmHg, 1 ~ 10 years < 70 mmHg + 2 × age in years, 10 ~ 14 years < 90 mmHg [9]. Hypotension in DBP was defined as follows: 1 ~ 12 months < 40 mmHg, 1 ~ 10 years < 50 mmHg, 10 ~ 14 years < 60 mmHg. The sting numbers/body surface area (BSA) were calculated instead of recording the absolute numbers of stings, as we believed that sting number/BSA might be a more appropriate indicator to estimate the severity of wasp stings in children.
Laboratory findings, such as peripheral total white blood cell count (WBC), neutrophil count (N), hemoglobin (Hb), platelet count (Plt), C-reactive protein (CRP, serum), alanine aminotransferase (ALT, serum), aspartate aminotransferase (AST, serum), total bilirubin (TBIL, serum), conjugated bilirubin (DBIL, serum), unconjugated bilirubin (IBIL, serum), troponin (cTnI, serum), creatine kinase (CK, serum), myoglobin (Mb, serum), lactate dehydrogenase (LDH, serum), prothrombin time (PT, plasma), activated partial thromboplastin time (APTT, plasma) and blood glucose (Glu, serum) were also collected. Blood urea nitrogen (BUN, serum) and blood creatinine (Cr, serum) were not included as potential risk factors for AKI, as they were used for the definition of AKI.
Sequential organ failure assessment scoring (SOFA)
SOFA scoring involved the detection and evaluation of various systems, including the respiratory function, nervous system, cardiovascular system, coagulation function, liver and kidney function. Each component was assigned a score ranging from 0 to 4 points, resulting in a total score of 24 points. A higher score indicated a more severe condition. However, considering that the kidney score might affect the SOFA results, we excluded it from the revised SOFA score (rSOFA).
Management
For children with MODS, appropriate management is very important. In addition to supportive treatments such as removing the stingers, taking JiDesheng anti-venom tablets (a widely used Chinese herb in China), anti-allergic treatment, rehydration, maintaining electrolyte balance and nutritional support, blood purification treatments were deemed to be the most important therapy.
Each vascular access for blood purification was established by inserting Gambro single-needle double lumen catheter (6F, 8F or 11F) into the femoral vein or subclavian vein. There were four modes of blood purification treatments, including ⑴ hemoperfusion: performed using the Fresenius blood purification machine (5008S, Germany) and hemoperfusion column (YTS-100 or YTS-160, China). This method facilitates the removal of large molecular toxins by adsorption; ⑵ therapeutic plasma exchange (TPE): carried out using either the Prismaflex blood purification machine with its plasma separator (TPE1000 or TPE2000, Gambro, Germany) or the Multifiltrate blood purification machine with its plasma separator (P1 or P2, produced by Fresenius, Germany). Each TPE treatment involved removing plasma volume approximately 5% of the body weight and replacing it with an equal volume of fresh frozen plasma (FFP). TPE eliminates the toxins present in the blood plasma; ⑶sustained low efficiency dialysis (SLED): employed for children with an elevated level of serum nitrogen or creatine, by using the Fresenius hemodialysis machine (5008S, Germany). Although SLED has a lower clearing efficiency than continuous kidney replacement therapy (CKRT), it is a cost-effective option; ⑷ CKRT: utilized for children with AKI, volume overload, or acute pulmonary edema. Prismaflex or Multifiltrate blood purification machines were employed to manage these critical conditions. We recorded the modes and sessions in both groups, and compared them and the clinical outcomes between the groups. Besides, we also recorded the durations of hospitalization.
Statistics
All data were processed using SPSS 23.0 statistical software (IBM Corporation, Armonk, NY, USA). The data were presented in the form of numbers (percentages), means ± standard deviation, or median (minimum, maximum) according to their distributions. Measurement data were analyzed using the t-test or Wilcoxon test, while categorical data were analyzed using Pearson χ2 test or Fisher’s exact test. Potential risk factors were analyzed by univariable and multivariable logistic regression. The association between potential risk factors and AKI was quantified using odds ratios (OR) and 95% confidence intervals (CI). P values < 0.05 were considered statistically significant.
Results
Basic information
From January 2014 to January 2022, a total of 118 cases of hospitalized children with wasp or bee stings in the Pediatric Nephrology department of West China Second Hospital of Sichuan University were enrolled. Among these cases, 48 children (48/118, 40.7%) experienced severe wasp stings (Fig. 1). The median age of the 48 children was 5.3 years (IQR: 2.8 ~ 10.3 years), median body weight was 18.8 kg (IQR: 15 ~ 29.8 kg) (Table 1).
Among the severe wasp sting cases, there were 27 males (56.2%) and 21 females (43.8%). The majority of the children experienced wasp stings in Autumn (August to November) (46/48, 95.8%). Blood pressure measurements revealed that SBP varied from 79 to 140 mmHg (mean 110.6 mmHg) and DBP from 45 to 97 mmHg (mean 65.3 mmHg). There was no significant difference between the two groups in terms of age, gender, weight, and SBP. However, a statistically significant difference was found in DBP, where the AKI group had relatively higher DBP (Table 1).
Acute kidney injury
According to the 2012 KDIGO Guidelines for AKI, 20 children (41.7%) with severe wasp sting injuries were diagnosed with AKI. Among them, 9 children (45.0%) were classified as stage 1; 5 children (25.0%) stage 2; and 6 cases (30.0%) stage 3. The other 28 children (58.3%) did not develop AKI. Among the children with AKI, 80% exhibited elevated serum creatine levels within 24 h. The median time of serum creatine elevation in children after wasp stings was 17.5 h (5 ~ 75 h), and the median time for peak serum creatine value was 28.5 h (5, 137 h). Five cases in the AKI group and five cases in the non-AKI group reported prehospital oliguria, but oliguria or anuria was observed in only 7 cases from the AKI group during the initial 24 h of hospitalization. Urinary glucose was found to be positive in 5 cases with AKI (5/20, 25%) and 3 cases without AKI (3/28, 10.7%). However, in all the 8 cases, the urinary glucose disappeared within one week (1 ~ 7 d).
Clinical manifestations
The 48 patients exhibited various clinical manifestations. All of the cases suffered pain in the sting areas (48/48, 100%), and nearly one-third had cola-colored urine (19/48, 39.6%) and vomiting (18/48, 37.5%). The specific clinical manifestations of both groups are listed in Table 1. Of note, most of the 19 patients with cola-colored urine (12/19, 63.2%) had no hematuria upon urinalysis, i.e. urine red blood cells (RBC) < 3/HP (high power field, × 400). Five children had slightly elevated RBC in urine (urine RBC 3 ~ 10/HP, × 400), and two children had significantly elevated RBC with urine RBC 3 + ~ 4 + /HP (3 + : urine red blood cells seen up to 3/4 per HP, × 400; 4 + : urine RBC seen in each HP, × 400). CK was also analyzed among the 19 cases with cola-colored urine, and we found an interesting phenomenon: the average level of CK in the 2 cases with significant hematuria (26,557.5 U/L) was much higher than that of the 12 cases (7597.5 U/L) without hematuria, suggesting that the higher the CK level was, the more severe the hematuria. The numbers of wasp stings were recorded, ranging from 1 to 75 stings. Two children with 1 sting were a 4-month-old boy and 7-month-old girl. The sting numbers/BSA varied from 1.36/m2 to 74.4/m2, and the ratios were significantly higher in AKI group (P < 0.01) (Table 1).
Revised SOFA scores were also recorded within the first 24 h after the wasp stings in the 48 children. In total, rSOFA scores in the AKI group (median 3.5) were higher than those in the non-AKI group (median 1).
There were significant differences in incidences of cola-colored urine and jaundice, in the sting numbers/BSA and rSOFA scores between the two groups. The AKI group appeared to have higher incidences of cola-colored urine and jaundice, higher sting numbers/BSA and higher rSOFA scores (Table 1).
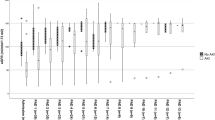
Changes in laboratory indicators
Laboratory findings included WBC (× 109/L), N (× 109/L), Hb (g/L), Plt (× 109/L), CRP (mg/L), ALT (U/L), AST (U/L), TBIL (μmol/L), IBIL (μmol/L), DBIL (μmol/L), LDH (U/L), cTnI (μg/L), CK (U/L), Mb (μg/L), PT (s), APTT (s) and Glu (mmol/L). The results showed statistically significant differences between the AKI and non-AKI groups in CRP, ALT, AST, TBIL, LDH, UN, Scr, cTnI, CK, and PT. Compared with the non-AKI group, the AKI group exhibited significantly elevated ALT, AST, TBIL, DBIL, LDH, and CK levels and moderately elevated CRP, cTnI IBIL, and PT levels (Table 2).
Logistic regression
In the multiple rounds of multivariable logistic regression analysis, due to the limited sample size, two to three confounders were included each round. All confounders included age, gender, weight, clinical manifestations and laboratory indicators. In each round of multivariable logistic regression analysis, cola-colored urine was always found to be significantly different between the two groups, thus was considered to be a potential risk factor for AKI with MODS (p < 0.05). However, jaundice and sting numbers/BSA could not be considered as potential risk factors for AKI (p > 0.05) (Table 3).
Management and prognosis
Blood purification treatment: The modes and sessions of blood purification treatment depended on the clinical manifestations and the consents from the guardians of the patients. In AKI group (n = 20), a total of 106 sessions were performed in 18 patients (most cases underwent more than one session): 3 hemoperfusions (3/106, 2.8%), 42 TPE (42/106, 39.6%), 13 SLED (13/106, 12.3%), and 48 CKRT (48/106, 45.3%). Thus, among these sessions, mostly TPE and CKRT were performed in the AKI group. Of the 8 cases who underwent a single mode of blood purification, 5 cases receiving only TPE recovered within 3 ~ 5 days; 2 cases receiving only SLED and having increased creatinine levels did not recover in one-month follow-up period; and 1 case receiving only CKRT recovered within 8 d. Of the 10 cases who underwent more than one mode of blood purification (each mode 1 ~ 17 sessions), 1 patient died; 6 patients recovered in 7 ~ 11 d; and the other 3 patients’ creatinine did not recover in one-month follow-up period. Of the 2 cases who did not receive any blood purification, one patient died quickly after admission and the other refused to receive any therapy and was lost to follow-up. In the non-AKI group (n = 28), 46 sessions of blood purification treatment were performed: 4 hemoperfusions (4/46, 8.7%), 39 TPE (39/46, 84.8%), 0 SLED and 3 CKRT (3/46, 6.5%). Of the non-AKI cases, 2 underwent more than one mode of blood purification (each mode 1 ~ 3 sessions); 15 underwent only one mode of blood purification (each mode 2 ~ 4 sessions); and 11 did not receive any blood purification. All of the cases in non-AKI group recovered and were discharged within 2 weeks. Regarding hospitalization durations, the average length of hospital stay in the AKI group was 13.5 d, compared to 6.2 d in the non-AKI group (P < 0.05). Of the two patients who died with AKI (2/20, 10%), one was a five-year-old boy who died from cardiac arrest, and the other was a four-year-old boy who died from acute pulmonary edema. No death was found in the non-AKI group.
Discussion
It has been reported that patients suffering from wasp stings often develop AKI. However, AKI induced by wasp stings has its own characteristics compared to AKI in other conditions, such as sepsis-associated acute kidney injury [10], obstructive nephropathy, underlying chronic renal diseases, etc. In this study, the pediatric cases did not have any underlying diseases and the wasp stings were the only pathogenic factors.
Although there are almost 5,000 species of wasp known all over the world, the components of venom are similar. Wasp venom is a transparent complicated mixture stored in a venom sac, and is 20 times more toxic than bee venom. Wasp venom’s chemical composition includes amines (melittin, histamine, dopamine), peptides (kinin, mast cell degranulation polypeptide), and high molecular weight proteins (neurotoxic protein, phospholipase A2, hyaluronidase) [11]. The most important substances leading to organ lesions are melittin, phospholipase A2, hyaluronidase, and antigen 5 [12]. Melittin, which has been recently found to play an active role in cancer and infection [13,14,15], is an antimicrobial peptide that strongly damages cell membranes, leading to leakage of cell contents, and eventually cell death [16, 17]. It can also cause central nervous system damage through the blood–brain barrier due to its small molecular weight [18]. Phospholipase A2 mainly cooperates with melittin to cause acute hemolysis. Both phospholipase A2 and histamine can cause allergic reactions [19]. Undoubtedly, these toxins can stimulate the body to produce inflammatory reactions. Li et al. found that the levels of IL-2, IL-6, IL-10, TNF-α and IL-17 were elevated in wasp sting patients; in particular, IL-6, IL-10 and IL-17 levels were significantly increased in the AKI group compared with the non-AKI group [20]. Both the toxins in the venom and secondary inflammatory factors can lead to damage to vital organs like the kidney.
AKI is a common phenomenon in patients following wasp stings and attracts attention from physicians and researchers. Vikrant and Parashar reported a series of 32 adults with wasp stings, and concluded that AKI was a serious complication with a high mortality rate (50%), and that severe cases might progress to MODS, affecting liver, lung, kidney, and coagulation systems [7, 21]. Although concerned about AKI in wasp stings, few researchers have investigated the risk factors associated with AKI. In a retrospective study conducted by Liu et al., which included 1,131 adults with wasp stings, it was suggested that tea-colored urine, number of stings, LDH, and TBIL were risk factors for developing a severe case of wasp stings [22]. After observation of 11 farmers with multiple wasp stings, Dhanapriya et al. concluded that AKI was most commonly associated with rhabdomyolysis [3]. On the analysis of 112 adult patients with hospital admissions resulting from wasp stings, Yuan et al. suggested that high leukocytes, high myoglobin, and high urinary MCP-1 upon admission, were risk factors for AKI [6]. This study is the first study focusing on children with AKI induced by severe wasp stings. We found that cola-colored urine, oliguria, jaundice. and higher rSOFA scores, as well as a higher level of CRP, ALT, AST, TBIL, LDH, cTnI, CK and PT might be candidate risk factors for AKI in children.
In order to exclude confounding factors, this study only included children with severe wasp stings who developed MODS. Children without MODS were excluded. The children with MODS were divided into the AKI group and the non-AKI group, ensuring conditions of both groups were well-balanced. Although this management resulted in exclusion of some cases with wasp stings, it might be better for accurate identification of potential risk factors for AKI in wasp sting patients.
Previously known pathogenesis of AKI in wasp sting patients included hypotension, which was thought to play an important role in prerenal acute renal insufficiency. However, recent findings suggested that hypotension was not as common as previously thought [23,24,25]. This study suggested that hypertension was more common in children affected by wasp stings and hypotension or hypoperfusion caused by the inflammatory response in wasp sting patients did not play a major role in the mechanism of AKI.
Cola-colored urine is a prominent clinical manifestation after wasp stings. In a series of adult cases, Wang et al. suggested that macroscopic hematuria could be considered as a surrogate marker of deteriorating clinical outcomes in wasp sting patients [26]. In this study, cola-colored urine was identified as a potential risk factor for AKI in children following wasp stings. Cola-colored urine, occurring as an early symptom, can also be considered an early predictor of AKI after multiple wasp stings. Here we described cola-colored urine instead of macroscopic hematuria. As in this study, 19 children exhibited cola-colored urine, but the majority (12 cases) showed no hematuria by urinalysis (urine RBC < 3/HP) with 5 children having slightly elevated RBC in urine (urine RBC 3 ~ 10/HP) and only 2 children having significantly elevated RBC in urine (urine RBC 3 + ~ 4 + /HP). It at least indicated that glomerular injury did not play a major role in the occurrence of AKI, which is consistent with the previously reported kidney injury mechanism [27,28,29]. For rural village hospitals or health centers, this early indicator does not require a laboratory test and is very easy for rural doctors to judge, to estimate the high risk of kidney injury, and to make timely and correct decisions on referral [30].
Jaundice, as another symptom after wasp stings, appeared to be a risk factor according to our χ2 test, but logistic regression did not show a significant difference. Different from the study by Yuan et al. [6], no significant differences in the levels of WBC, N, Hb, and PLT were observed between AKI and non-AKI groups, possibly due to the inclusion of only MODS cases in our study.
In our data, the fact that one sting induced MODS in 2 children (4-month-old boy and 7-month-old girl) attracted our attention, and we realized the absolute sting numbers might not be appropriate in assessing the sting severity in children. Different from the variables in adults, we introduced the concept of the sting number/BSA, due to the fact that children are constantly growing individuals and there are significant differences among children. From the results in this study, the median ratio of the sting number/BSA in AKI group (mean 29.3/m2) was more than 2 times of that in non-AKI group (mean 13.1/m2).
Pathology of kidney biopsy in AKI patients after wasp stings has been investigated by researchers. Based on literature reports, wasp sting patients showed mostly mild tubulointerstitial nephritis [31, 32], while others showed pigment nephropathy [33], mesangial proliferative glomerulonephritis [34], acute tubular necrosis [35,36,37], minimal-change disease [38], and glomerulonephritis. In some rare conditions, acute renal cortical necrosis occurred.
Though this is the first study to analyze the risk factors of AKI in children after wasp stings, it has some limitations. First, the limited number of cases might lead to ignorance of some other risk factors, thus more studies and cases are needed to address this issue. Second, we did not include the data concerning markers of tubular damage and urine myoglobin. Third, kidney biopsy was not performed in these children and would otherwise undoubtedly enhance our knowledge of wasp sting-induced AKI in children.
Conclusion
In conclusion, this study retrospectively explored the risk factors of AKI in 48 pediatric cases with MODS after wasp stings. The findings suggest that cola-colored urine is a potential risk factor and an early indicator for AKI in children following wasp stings. Additionally, the AKI group presented more jaundice cases, higher sting numbers/BSA, higher levels of CRP, ALT, AST, TBIL, LDH, cTnI, and CK. Therefore, the findings are helpful for pediatricians to identify cases with a higher risk of AKI and enable prompt management of this serious condition.
Data Availability
All data included in this study are available upon request by contact with the corresponding author.
Abbreviations
- ALT :
-
Alanine aminotransferase
- APTT :
-
Activated partial thromboplastin time
- ARDS :
-
Acute respiratory distress syndrome
- AST :
-
Aspartate aminotransferase
- BSA :
-
Body surface area
- BUN :
-
Blood urea nitrogen
- CK :
-
Creatine kinase
- CKD :
-
Chronic kidney disease
- CRP :
-
C-reactive protein
- CKRT :
-
Continuous kidney replacement therapy
- cTnI :
-
Troponin
- DBIL :
-
Conjugated bilirubin
- IBIL :
-
Unconjugated bilirubin
- LDH :
-
Lactate dehydrogenase
- MCP-1 :
-
Monocyte chemotactic protein-1
- MODS :
-
Multiple organ dysfunction syndrome
- PT :
-
Prothrombin time
- rSOFA :
-
Revised SOFA
- SLED :
-
Sustained low efficiency dialysis
- SOFA :
-
Sequential organ failure assessment scoring
- TBIL :
-
Total bilirubin
- TPE :
-
Therapeutic plasma exchange
References
Sitprija V, Boonpucknavig V (1972) Renal failure and myonecrosis following wasp-stings. Lancet 1:749–750. https://doi.org/10.1016/s0140-6736(72)90267-x
Zhang L, Yang Y, Tang Y et al (2013) Recovery from AKI following multiple wasp stings: a case series. Clin J Am Soc Nephrol 8:1850–1856
Dhanapriya J, Dineshkumar T, Sakthirajan R, Shankar P, Gopalakrishnan N, Balasubramaniyan T (2016) Wasp sting-induced acute kidney injury. Clin Kidney J 9:201–204
Xie C, Xu S, Ding F et al (2013) Clinical features of severe wasp sting patients with dominantly toxic reaction: analysis of 1091 cases. PLoS One 8:e83164
Tang X, Lin L, Yang YY et al (2022) Development and validation of a model to predict acute kidney injury following wasp stings: A multicentre study. Toxicon 209:43–49
Yuan H, Lu L, Gao Z, Hu F (2020) Risk factors of acute kidney injury induced by multiple wasp stings. Toxicon 182:1–6
Vikrant S, Parashar A (2017) Acute kidney injury due to multiple Hymenoptera stings-a clinicopathological study. Clin Kidney J 10:532–538
Flynn JT, Kaelber DC, Baker-Smith CM et al (2017) Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 140:e20171904
Badjatia N, Carney N, Crocco TJ et al (2008) Guidelines for prehospital management of traumatic brain injury 2nd edition. Prehosp Emerg Care 12 Suppl 1:S1–52
Poston JT, Koyner JL (2019) Sepsis associated acute kidney injury. BMJ 364:k4891
Abd El-Wahed A, Yosri N, Sakr HH et al (2021) Wasp Venom Biochemical Components and Their Potential in Biological Applications and Nanotechnological Interventions. Toxins (Basel) 13:206
Golden DB (2005) Insect sting allergy and venom immunotherapy: a model and a mystery. J Allergy Clin Immunol 115:439–447; quiz 448
Memariani H, Memariani M, Moravvej H, Shahidi-Dadras M (2020) Melittin: a venom-derived peptide with promising anti-viral properties. Eur J Clin Microbiol Infect Dis 39:5–17
Rady I, Siddiqui IA, Rady M, Mukhtar H (2017) Melittin, a major peptide component of bee venom, and its conjugates in cancer therapy. Cancer Lett 402:16–31
Yu X, Dai Y, Zhao Y et al (2020) Melittin-lipid nanoparticles target to lymph nodes and elicit a systemic anti-tumor immune response. Nat Commun 11:1110
van den Bogaart G, Guzmán JV, Mika JT, Poolman B (2008) On the mechanism of pore formation by melittin. J Biol Chem 283:33854–33857
Lee MT, Sun TL, Hung WC, Huang HW (2013) Process of inducing pores in membranes by melittin. Proc Natl Acad Sci U S A 110:14243–14248
Hong J, Lu X, Deng Z, Xiao S, Yuan B, Yang K (2019) How Melittin Inserts into Cell Membrane: Conformational Changes, Inter-Peptide Cooperation, and Disturbance on the Membrane. Molecules 24:1775
Ma D, Li Y, Dong J et al (2011) Purification and characterization of two new allergens from the salivary glands of the horsefly, Tabanus yao. Allergy 66:101–109
Li F, Liu L, Guo X et al (2019) Elevated cytokine levels associated with acute kidney injury due to wasp sting. Eur Cytokine Netw 30:34–38
Vikrant S, Parashar A (2017) Wasp venom-induced acute kidney injury: a serious health hazard. Kidney Int 92:1288
Liu Y, Shu H, Long Y et al (2022) Development and internal validation of a Wasp Sting Severity Score to assess severity and indicate blood purification in persons with Asian wasp stings. Clin Kidney J 15:320–327
Kim YO, Yoon SA, Kim KJ et al (2003) Severe rhabdomyolysis and acute renal failure due to multiple wasp stings. Nephrol Dial Transplant 18:1235
Bhatta N, Singh R, Sharma S, Sinnha A, Raja S (2005) Acute renal failure following multiple wasp stings. Pediatr Nephrol 20:1809–1810
Nandi M, Sarkar S (2012) Acute kidney injury following multiple wasp stings. Pediatr Nephrol 27:2315–2317
Wang M, Prince S, Tang Y et al (2021) Macroscopic hematuria in wasp sting patients: a retrospective study. Ren Fail 43:500–509
Yuan H, Gao Z, Chen G et al (2022) An integrative proteomics metabolomics based strategy reveals the mechanisms involved in wasp sting induced acute kidney injury. Toxicon 205:1–10
Singh H, Chaudhary D, Dhibar DP (2021) Rhabdomyolysis and acute kidney injury following multiple wasp stings. QJM 114:53–54
Radhakrishnan H (2014) Acute kidney injury and rhabdomyolysis due to multiple wasp stings. Indian J Crit Care Med 18:470–472
Lama T, Karmacharya B, Chandler C, Patterson V (2011) Telephone management of severe wasp stings in rural Nepal: a case report. J Telemed Telecare 17:105–108
Vachvanichsanong P, Dissaneewate P (2009) Acute renal failure following wasp sting in children. Eur J Pediatr 168:991–994
Lin CJ, Wu CJ, Chen HH, Lin HC (2011) Multiorgan failure following mass wasp stings. South Med J 104:378–379
Natarajan G, Jeyachandran D, Thanigachalam D, Sakthirajan R, Balasubramaniyan T, Kurien AA (2016) Myoglobinuric renal failure after a wasp attack. Kidney Int 89:725
Tauk B, Hachem H, Bastani B (1999) Nephrotic syndrome with mesangial proliferative glomerulonephritis induced by multiple wasp stings. Am J Nephrol 19:70–72
Zhang R, Meleg-Smith S, Batuman V (2001) Acute tubulointerstitial nephritis after wasp stings. Am J Kidney Dis 38:E33
Yu F, Cui L, Gao Z, Lu X, Hu F, Yuan H (2022) A rat model of acute kidney injury caused by multiple subcutaneous injections of Asian giant hornet (Vespa mandarina Smith) venom. Toxicon 213:23–26
Zhang L, Tang Y, Liu F et al (2012) Multiple organ dysfunction syndrome due to massive wasp stings: an autopsy case report. Chin Med J (Engl) 125:2070–2072
Humeda YS, Clapp WL, Humeda H (2022) Minimal change disease after multiple wasp stings. Clin Nephrol Case Stud 10:16–20
Acknowledgements
We gratefully acknowledge the help of Xiuying Chen, Yuhong Tao and Kunhua Cui in the management of these patients.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities (SCU2022D022) and Sichuan Maternal and Child Health Association (2020YB10).
Author information
Authors and Affiliations
Contributions
Jing Lu and Hanmin Liu conceived and designed the project. Jing Lu, Yannan Guo, Liqun Dong and Lijuan Zhang collected the cases and performed the analysis. Jing Lu drafted the manuscript. Yang Liu revised the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Ethics approval was obtained from the Medical Ethics Committee of West China Second Hospital of Sichuan University. The procedures used in this study adhered to the tenets of the Declaration of Helsinki.
Competing Interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, J., Dong, L., Zhang, L. et al. Analysis of risk factors for acute kidney injury in children with severe wasp stings. Pediatr Nephrol 39, 1927–1935 (2024). https://doi.org/10.1007/s00467-023-06265-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06265-6