Abstract
Background
Many recommendations regarding peritonitis prevention in international consensus guidelines are opinion-based rather than evidence-based. The aim of this study was to examine the impact of peritoneal dialysis (PD) catheter insertion technique, timing of gastrostomy placement, and use of prophylactic antibiotics prior to dental, gastrointestinal, and genitourinary procedures on the risk of peritonitis in pediatric patients on PD.
Methods
We conducted a retrospective cohort study of pediatric patients on maintenance PD using data from the SCOPE collaborative from 2011 to 2022. Data pertaining to laparoscopic PD catheter insertion (vs. open), gastrostomy placement after PD catheter insertion (vs. before/concurrent), and no prophylactic antibiotics (vs. yes) were obtained. Multivariable generalized linear mixed modeling was used to assess the relationship between each exposure and occurrence of peritonitis.
Results
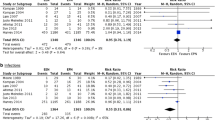
There was no significant association between PD catheter insertion technique and development of peritonitis (aOR = 2.50, 95% CI 0.64–9.80, p = 0.19). Patients who had a gastrostomy placed after PD catheter insertion had higher rates of peritonitis, but the difference was not statistically significant (aOR = 3.19, 95% CI 0.90–11.28, p = 0.07). Most patients received prophylactic antibiotics prior to procedures, but there was no significant association between prophylactic antibiotic use and peritonitis (aOR = 1.74, 95% CI 0.23–13.11, p = 0.59).
Conclusions
PD catheter insertion technique does not appear to have a significant impact on peritonitis risk. Timing of gastrostomy placement may have some impact on peritonitis risk. Further study must be done to clarify the effect of prophylactic antibiotics on peritonitis risk.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to SCOPE data use agreements but are available from the corresponding author on reasonable request.
References
Fadrowski JJ, Rees L (2021) The demographics of dialysis in children. In: Pediatric Dialysis. Springer International Publishing, Cham, pp 35–46. https://doi.org/10.1007/978-3-030-66861-7_3
Warady BA, Sullivan EK, Alexander SR (1996) Lessons from the peritoneal dialysis patient database: a report of the north american pediatric renal transplant cooperative study. Kidney Int Suppl 53:S68–S71
Chadha V, Schaefer FS, Warady BA (2010) Dialysis-associated peritonintis in children. Pediatr Nephrol 25:425–440. https://doi.org/10.1007/s00467-008-1113-6
Neu AM, Miller MR, Stuart J, Lawlor J, Richardson T, Martz K, Rosenberg C, Newland J, McAfee N, Begin B, Warady BA (2014) Design of the standardizing care to improve outcomes in pediatric end stage renal disease collaborative. Pediatr Nephrol 29:1477–1484. https://doi.org/10.1007/s00467-014-2891-7
Neu AM, Richardson T, Lawlor J, Stuart J, Newland J, McAfee N, Warady BA, Zaristky J, Kieffner S, Redpath Mahon A, Foster D, Keswani M, Majkowski N, Blaszak R, Blaszak C, Somers M, Pak T, Aviles D, Jenkins E, Lestz R, Sanchez A, Pan C, Dake J, Quigley R, Warady B, Grimes J, Mistry K, Carver J, Van De Voorde R, Irvin E, Al-Akash S, Stone B, Hidalgo G, Harrington M, Neu A, Case B, Gupta S, Baker A, Weaver J, Chua A, Wong C, Begin B, Salusky I, Gales B, Patel H, Smith B, Joseph M, Haskins D, Kenagy D, Vogt B, Hanevold C, McAfee N, Beck A, Shea M, Sethna C, Cho M, Scwartz S, Currier H, Skversky A, Eisele M, Pradhan M, Breen C, Brakeman P, Campopiano L, Jetton J, Ehrlich J, Shoemaker L, Zacharek N (2016) Implementation of standardized follow-up care significantly reduces peritonitis in children on chronic peritoneal dialysis. Kidney Int 89:1346–1354. https://doi.org/10.1016/j.kint.2016.02.015
Neu AM, Richardson T, De Souza HG, Mahon AR, Keswani M, Zaritsky J, Munshi R, Swartz S, Sethna CB, Somers MJG, Warady BA (2021) Continued reduction in peritonitis rates in pediatric dialysis centers: results of the standardizing care to improve outcomes in pediatric end stage renal disease (SCOPE) collaborative. Pediatr Nephrol 36:2383–2391. https://doi.org/10.1007/s00467-021-04924-0
Sethna CB, Bryant K, Munshi R, Warady BA, Richardson T, Lawlor J, Newland JG, Neu A (2016) Risk factors for and outcomes of catheter-associated peritonitis in children: the SCOPE collaborative. Clin J Am Soc Nephrol 11:1590–1596. https://doi.org/10.2215/CJN.02540316
Warady BA, Bakkaloglu S, Newland J, Cantwell M, Verrina E, Neu A, Chadha V, Yap H, Schaefer F (2012) Consensus guidelines for the prevention and treatment of catheter-related infections and peritonitis in pediatric patients receiving peritoneal dialysis: 2012 update. Perit Dial Int 32:S32–S86. https://doi.org/10.3747/pdi.2011.00091
Gadallah MF, Pervez A, El-Shahawy MA, Sorrells D, Zibari G, McDonald J, Work J (1999) Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: a prospective randomized study on outcome. Am J Kidney Dis 33:118–122. https://doi.org/10.1016/S0272-6386(99)70266-0
Wright MJ, Bel’eed K, Johnson BF, Eadington DW, Sellars L, Farr MJ (1999) Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int 19:372–375. https://doi.org/10.1177/089686089901900415
van Laanen JHH, Cornelis T, Mees BM, Litjens EJ, van Loon MM, Tordoir JHM, Peppelenbosch AG (2018) Randomized controlled trial comparing open versus laparoscopic placement of a peritoneal dialysis catheter and outcomes: the capd i trial. Perit Dial Int 38:104–112. https://doi.org/10.3747/pdi.2017.00023
Stringel G, McBride W, Weiss R (2008) Laparoscopic placement of peritoneal dialysis catheters in children. J Pediatr Surg 43:857–860. https://doi.org/10.1016/j.jpedsurg.2007.12.026
Carpenter JL, Fallon SC, Swartz SJ, Minifee PK, Cass DL, Nuchtern JG, Pimpalwar AP, Brandt ML (2016) Outcomes after peritoneal dialysis catheter placement. J Pediatr Surg 51:730–733. https://doi.org/10.1016/j.jpedsurg.2016.02.011
Ramage IJ, Geary DF, Harvey E, Secker DJ, Balfe JA, Balfe JW (1999) Efficacy of gastrostomy feeding in infants and older children receiving chronic peritoneal dialysis. Perit Dial Int 19:231–236. https://doi.org/10.1177/089686089901900308
Ledermann SE, Spitz L, Moloney J, Rees L, Trompeter RS (2002) Gastrostomy feeding in infants and children on peritoneal dialysis. Pediatr Nephrol 17:246–250. https://doi.org/10.1007/s00467-002-0846-x
Warady BA, Feneberg R, Donmez O, Sever L, Sirin A, Alexander SR, Schaefer F, Verrina E, Flynn JT, Muller-Wiefel DE, Besbas N, Zurowska A, Aksu N, Fischbach M, Sojo E (2007) Peritonitis in children who receive long-term peritoneal dialysis: a prospective evaluation of therapeutic guidelines. J Am Soc Nephrol 18:2172–2179. https://doi.org/10.1681/ASN.2006101158
von Schnakenburg C, Feneberg R, Plank C, Zimmering M, Arbeiter K, Bald M, Fehrenbach H, Griebel M, Licht C, Konrad M, Timmermann K, Kemper MJ (2006) Percutaneous endoscopic gastrostomy in children on peritoneal dialysis. Perit Dial Int 26:69–77. https://doi.org/10.1177/089686080602600111
Dorman RM, Benedict LA, Sujka J, Sobrino J, Dekonenko C, Andrews W, Warady B, Oyetunji TA, Hendrickson RJ (2019) Safety of laparoscopic gastrostomy in children receiving peritoneal dialysis. J Surg Res 244:460–467. https://doi.org/10.1016/j.jss.2019.06.090
Kempf C, Holle J, Berns S, Henning S, Bufler P, Müller D (2022) Feasibility of percutaneous endoscopic gastrostomy insertion in children receiving peritoneal dialysis. Perit Dial Int 42:482–488. https://doi.org/10.1177/08968608211057651
Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK (2008) Bacteremia associated with toothbrushing and dental extraction. Circulation 117:3118–3125. https://doi.org/10.1161/CIRCULATIONAHA.107.758524
Kiddy K, Brown PP, Michael J, Adu D (1985) Peritonitis due to streptococcus viridans in patients receiving continuous ambulatory peritoneal dialysis. BMJ 290:969–970. https://doi.org/10.1136/bmj.290.6473.969-a
Yip T, Tse KC, Lam MF, Cheng SW, Lui SL, Tang S, Ng M, Chan TM, Lai KN, Lo WK (2007) Risks and outcomes of peritonitis after flexible colonoscopy in capd patients. Perit Dial Int 27:560–564. https://doi.org/10.1177/089686080702700517
Gweon T, Jung SH, Kim SW, Lee K, Cheung DY, Lee B, Choi H (2019) Risk factors for peritonitis in patients on continuous ambulatory peritoneal dialysis who undergo colonoscopy: a retrospective multicentre study. BMC Gastroenterol 19:175. https://doi.org/10.1186/s12876-019-1081-2
Fan P, Chan M, Lin S, Wu H, Chang M, Tian Y, Kuo G (2019) Prophylactic antibiotic reduces the risk of peritonitis after invasive gynecologic procedures. Perit Dial Int 39:356–361. https://doi.org/10.3747/pdi.2018.00218
Acknowledgements
Participating centers that contributed data to the SCOPE Collaborative:
Children’s of Alabama, Phoenix Children’s Hospital, Arkansas Children’s Hospital, Children’s Hospital Los Angeles, Lucile Packard Children’s Hospital Stanford, UCLA Mattel Children’s Hospital, UCSF Benioff Children’s Hospital San Francisco, University of California Davis Children’s Hospital, Children’s Hospital Colorado, Connecticut Children’s Medical Center, Yale-New Haven Children’s Hospital, Nemours/Alfred I. duPont Hospital for Children, Children’s National Hospital , Arnold Palmer Hospital for Children, Nicklaus Children’s Hospital, Children’s Healthcare of Atlanta, Ann & Robert H. Lurie Children’s Hospital of Chicago, University of Iowa Stead Family Children’s Hospital, Children’s Hospital of New Orleans, Johns Hopkins Children’s Center, Boston Children’s Hospital, C.S. Mott Children’s Hospital, Helen DeVos Children’s Hospital, Masonic Children’s Hospital—University of Minnesota, Children’s Mercy Kansas City, SSM Health Cardinal Glennon Children’s Hospital, St. Louis Children’s Hospital, Children’s Hospital & Medical Center, Cohen Children’s Medical Center, Golisano Children’s Hospital at The University of Rochester Medical Center, New York-Presbyterian Morgan Stanley Children’s Hospital, The Children’s Hospital at Montefiore, The Mount Sinai Kravis Children’s Hospital, Upstate Golisano Children’s Hospital, Levine Children’s Hospital, Akron Children’s Hospital, Cincinnati Children’s Hospital Medical Center, Cleveland Clinic Children’s Hospital, Nationwide Children’s Hospital, UH Rainbow Babies & Children’s Hospital, Oklahoma Children’s Hospital, Doernbecher Children’s Hospital at Oregon Health & Science University, Children’s Hospital of Philadelphia, St. Christopher’s Hospital for Children, UPMC Children’s Hospital of Pittsburgh, MUSC Shawn Jenkins Children’s Hospital, Children’s Health Dallas, Cook Children’s Medical Center, Dell Children’s Medical Center of Central Texas, Driscoll Children’s Hospital, Texas Children’s Hospital, Primary Children’s Hospital, UVA Children’s Hospital, Seattle Children’s, American Family Children’s Hospital, Children’s Wisconsin
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wasik, H.L., Keswani, M., Munshi, R. et al. Assessment of potential peritonitis risk factors in pediatric patients receiving maintenance peritoneal dialysis. Pediatr Nephrol 38, 4119–4125 (2023). https://doi.org/10.1007/s00467-023-06076-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06076-9