Abstract
Background
Recommendations on when to start enzyme replacement therapy (ERT) in children with Fabry disease (FD) differ between guidelines. In this study, kidney biopsies of a cohort of 14 untreated children and one treated child were analyzed for their morphologic changes to determine whether early initiation of ERT is indicated.
Methods
All pediatric FD patients (< 18 years old) diagnosed between 2003 and 2021 in our department who received a kidney biopsy were enrolled. Clinical symptoms; laboratory parameters regarding kidney function, such as eGFR, plasma urea, protein-creatinine, and albumin/creatinine ratio; and 14 kidney biopsies prior to ERT and one under treatment were retrospectively analyzed.
Results
A total of 14 patients were enrolled, including 9 male and 5 female children, aged 3–18 years (median age 11). Seven of the enrolled children were 10 years old or younger. Histological analysis of kidney biopsy samples revealed severe vacuolization and accumulation of inclusions in podocytes and renal tubules. The majority of cases had no FD-specific clinical or laboratory features independent of age, gender, or genotype. The youngest FD patient presenting with isolated abnormal kidney biopsy was 3 years old.
Conclusions
We demonstrate that histological lesions, typical for FD, can be observed in kidney biopsies at a very young age in patients without classical clinical symptoms or laboratory abnormalities. Thus, we recommend kidney biopsies as a possible tool for early diagnosis of renal involvement in FD. As a consequence of these early biopsy findings without a clinical correlate, an early initiation of ERT should be considered.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fabry disease (FD) is a chronic, progressive, multisystem, X-linked lysosomal disorder caused by pathogenic variants in the galactosidase alpha (GLA) gene leading to a reduced activity of the enzyme galactosidase A (GALA) [1,2,3]. This mainly leads to a globotriaosylceramide (Gb3) accumulation within lysosomes in different organs [1,2,3], and less commonly to an accumulation of lipids such as digalactosyl ceramide and blood group B, B1, and P1 glycolipids [1,2,3]. The accumulation of Gb3 which begins in utero in the kidney cells is observed in adults mainly in the kidneys, heart, and cerebrovascular system and leads to severe organ complications, typically during the third to fifth decade of life [4,5,6,7].
FD can be categorized into two major forms: the severe classical form, with little residual enzyme activity, and the milder nonclassical form, also called late-onset phenotype [4]. Both forms affect female and male patients. Men with classical FD have a much higher risk of presenting with an event, especially they have a poorer kidney function and a higher left ventricular mass than women with classical FD and both women and men with non-classical FD [4]. Women rather show fibrosis in the absence of cardiac hypertrophy. Late-onset patients are mostly free of clinical symptoms in childhood and adolescence. They show a more variable disease course and are less severely affected; often, only one organ is affected by the disease [4]. Women with non-classical FD show the mildest disease course. For classical FD, there is a wide spectrum of disease severity and age of onset. Data on pediatric patients with classical FD show characteristic clinical features in male and female children, such as neuropathic pain, acroparesthesia, gastrointestinal symptoms, hypohidrosis, angiokeratomas, and ocular abnormalities such as cornea verticillate [2, 5, 8]. According to the Fabry Registry, the median age of onset of clinical symptoms is 6 years in males and 9 years in females [5]. However, accumulation of disease-specific deposits, such as podocyte inclusions in the glomeruli, may appear long before the patients present with typical clinical symptoms and organ-specific laboratory abnormalities [1, 2, 8, 9]. Initial signs are typically unspecific and may result in a significant delay of diagnosis [5]. This is also reflected by the fact that the majority of pediatric FD patients are detected by genetic screening due to a positive family history for FD [5]. Only a minority of pediatric FD patients are diagnosed as index patients [5]. Timely treatment is often hampered by a diagnostic delay leading to progressive damage of the kidneys, heart, and central nervous system with associated complications and thereby contributes to an increased morbidity and early mortality [2, 3, 10].
Enzyme replacement therapy (ERT) for FD was approved by the European Medicines Agency (EMA) for agalsidase beta (Fabryzyme®) and agalsidase alfa (Replage®) and by the U. S. Food and Drug Administration (FDA) for agalsidase beta (Fabrazyme®) in 2001 [11,12,13]. Several studies in adults have shown the positive effects of ERT, including reduction of glycolipid storage in different organs, reduced pain, and improvement of peripheral nerve function and sweating, as well as a reduction of cardiac hypertrophy [1, 8]. Clinical trials addressing the efficacy were all conducted in adults and only a small number of reports have documented the effects in children and adolescents [8]. In general, the treatment leads to an improvement of disease-related symptoms whereby a non-significant decrease of gastrointestinal symptoms was seen in boys [8]. In addition, it is believed that both agalsidase beta and agalsidase alfa have better clinical benefits when treatment initiation is established before Gb3 accumulation has induced kidney damage [3, 5, 14,15,16,17].
Morphological changes in the kidneys result from Gb3 accumulation in nearly all kidney cell types, with particularly dense accumulations found in podocytes and distal tubular epithelial cells [18]. They trigger interstitial inflammation and fibrosis, which can lead to chronic kidney disease (CKD) in adults [16, 17]. In a study with 58 patients (age > 16 years), accumulation of Gb3 in kidney tissue varied strongly but could significantly be reduced after 11 months on ERT [18]. ERT efficacy is less pronounced when the disease has reached the stage of CKD [1, 18,19,20]. In contrast, patients without impaired kidney function (no proteinuria and/or decreased glomerular filtration rate) are reported to have a better response to ERT [19]. In consequence, the current treatment recommendations for adults propose an early initiation of ERT to stop disease progression or even reverse organ damage [7, 21]. Nevertheless, the debate on when to initiate ERT in children is still ongoing and various recommendations have been made including different criteria regarding when to start ERT [3, 20].
Consensus criteria based on expert opinions include clinical symptoms and kidney involvement, such as proteinuria and/or elevated serum creatinine. However, morphological changes in kidney biopsies may be observed preceding proteinuria and/or elevated serum creatinine [2, 19, 22]. Yet screening for morphological changes in the glomeruli, as a marker for disease progression, has not been implemented as a standard diagnostic tool for FD prior to ERT. The absence of proteinuria/albuminuria is currently erroneously considered a measure to determine whether the kidney is affected or not. Therefore, the decision to start a treatment could be delayed in children who might benefit from initiation of ERT at an earlier time point. Thus, the decision to start ERT should not be based solely on proteinuria as a marker of kidney involvement [3].
Current US [20], French [23], and international [24] guidelines suggest different ages to start ERT (ranging from age 8 to 16). According to the latest publication in 2019 by Germain et al. [3], initiation of ERT is recommended at an age of 7 years independent of clinical or laboratory manifestations.
However, only little is known about the natural history of glomerular disease progression in the early phases of the disease or the silent kidney involvement in FD and is reviewed in Levstek et al. [21]. The study of Tøndel et al. is of particular interest, since progressive glomerular and vascular involvement in kidney biopsies from children and adolescents (age range 7–17 years) with FD could be observed even in the absence of proteinuria. Podocyte foot process effacement was found to be an early marker of nephropathy [7, 14]. Subsequently, the same author proposed that kidney biopsies are not only essential in the early diagnosis of nephropathy but might also serve in the evaluation of the response to ERT of early Fabry nephropathy [7]. Early initiation of ERT in children was documented to prevent progression of nephropathy on sequential kidney biopsies [14].
The intention of our study was to further investigate the kidney pathology by analyzing the kidney biopsies from a cohort of 14 untreated and one treated child with FD, as well as to review the evidence for an early intervention with ERT based on findings. Our results indicate that ERT initiation should be generally considered at younger ages, especially in male classical FD patients, but also in females with glomerular phenotypes, before FD-associated morphological changes in the kidney have developed.
Methods
Patients
All pediatric FD patients (< 18 years old) followed at the University Children’s Hospital Zurich diagnosed between 2003 and 2021 who underwent kidney biopsies were enrolled. All children, except two, had either albuminuria or microhematuria which led to the decision of performing a kidney biopsy. In patient 3, the kidney biopsy was performed due to clinical symptoms and in patient 6 due to family history with known kidney involvement.
Routine clinical monitoring included clinical visits every 6 to 12 months, measurement of kidney markers every 6 months, ECG and echocardiography every 12 months, and cardiac MRI every 5 years. FD was either suspected due to typical clinical symptoms and/or positive family history and was confirmed by the measurement of GALA activity in leukocytes, dried blood spots and/or plasma, and/or molecular genetics of the GLA gene. LysoGb3 measurement was included since 2019.
All data was collected retrospectively from the patient files and summarized in an Excel file. Kidney biopsy results were compared with biochemical measurements in urine and blood samples performed within the last 2 months before the kidney biopsy. Descriptive statistics were used to summarize the data. Due to the small number of patients a statistical analysis was not possible. The study was reviewed and approved by the local IRB (University Zurich). All participants signed a general consent to be included in research projects.
Clinical symptoms
The clinical characteristics of the children, as shown in Table 1, were assessed using the Mainzer Severity Score Index [25]. Ophthalmologic and cardiac changes were evaluated by an ophthalmologist and a cardiologist, respectively. We included general characteristics like gender, age, and GLA sequence variant, and the most common clinical parameters: neurological involvement (acroparesthesia, tinnitus, dizziness, hypo- or anhidrosis), gastrointestinal symptoms (abdominal pain, diarrhea, constipation), ophthalmologic abnormalities (cornea verticillate), cardiovascular abnormalities, and angiokeratomas.
Kidney-associated laboratory features
The following kidney-specific parameters were included: estimated glomerular filtration rate (eGFR) was expressed in millimeters per minute per 1.73 m2 according to the Schwartz formula [26] using the local factor κ of 40 for all children based on the plasma creatinine, which was measured by an enzymatic method. Other kidney-related parameters include plasma urea, protein/creatinine, and albumin/creatinine ratio, which were calculated from spot urine by measuring protein and albumin content (by immunoturbidimetric assay). Impaired eGFR was defined as < 90 ml/min per 1.72 m2. Elevated plasma urea was defined at > 7 mmol/L, microalbuminuria with an albumin/creatinine ratio > 3.4 mg/mmol Crea, and proteinuria with a protein/creatinine ratio > 20 mg/mmol Crea. Nephrotic range proteinuria is defined as a protein/creatinine ratio > 200 mg/mmol Crea. Urine sediment was analyzed by the flow cytometric method.
Morphological characteristics of the kidney
Since 2011, the University Children’s Hospital Zurich routinely performed kidney biopsies in all pediatric FD patients to evaluate the degree of kidney damage and confirm the indication for ERT.
Based upon the studies of Tøndel et al. [2] and the American [20] and French [3] recommendation for diagnosis, management, and treatment of FD, we decided to perform a baseline kidney biopsy prior to ERT, to also confirm the diagnosis, at the age 4–6 for boys and 12–15 for girls; a second biopsy is usually planned after 5 years on ERT or as a follow-up after 5 years, when the patient was not started on ERT. Within the period investigated in this publication, only one patient had a follow-up biopsy. All kidney biopsies were performed by an experienced nephrologist. The morphological characteristics were analyzed on light and electron microscopy by a specialized pathologist. To compare our results with current studies, one nephropathologist (A.G.) scored the biopsy samples based on a modified scoring system from Tøndel et al. [14]. Global glomerular sclerosis, focal segmental glomerulosclerosis, glomerular hyaline, interstitial fibrosis and arteriopathy, with PAS-positive hyaline-like material in the media of arterioles or arteries, replacing smooth muscle cells, was defined as Fabry arteriopathy [27]. Podocyte and tubular vacuolization were assessed on hematoxylin and eosin-stained and periodic acid-Schiff-stained slides. Inclusions in podocytes, mesangial cells, and tubular epithelial cells were assessed on methylene blue-azure stained semi-thin sections and with electron microscopy. Podocyte foot process effacement was evaluated on electron microscopy images and scored as segmental if comprising less than 50% of the capillary loop circumference. Plus signs indicate a clear occurrence of the feature, plus signs in parentheses indicate a slight occurrence, and minus signs indicate the absence of scored feature [14].
Treatment with ERT
The EMA approved agalsidase alfa and beta for ERT in FD in 2001. Pediatric patients at the University Children’s Hospital Zurich are currently treated with agalsidase alfa or agalsidase beta. Depending on the age of the patient this treatment is stated as off label, specifically under the age of 7.
Results
Fabry cohort, clinical and laboratory findings
A total of 14 patients were enrolled, including 9 male and 5 female children. One individual (patient 5, Tables 1 and 2) had two consecutive kidney biopsies, one before (5a) and one on ERT (5b). A total of 15 kidney biopsies were investigated. All patients were identified based on family history, respectively family screening. FD was confirmed using biochemical and/or genetic testing. All individuals were classified as having classical FD. Kidney biopsies prior to ERT were performed in a total of 14 patients with a median age of 11. 7 of the enrolled children were 10 years old or younger. Multiple affected individuals from 5 families were included: patients 1 and 2 are first cousins, 5 and 6 s cousins, and 8 and 9 twins. Children 10 and 11 and 12 and 13 are siblings.
Kidney biopsy findings
The morphologic changes in the kidney biopsy specimens (light and electron microscopy) for all our patients are shown in Table 3. All morphological changes are typical for FD. Only chloroquine toxicity would show similar changes in kidney biopsies. However, there was no known chloroquine intake in our patients.
Light microscopy showed podocyte vacuolization in all patients. In 13 out of 15 samples, tubular vacuolization was observed. Glomerulosclerosis, focal minimal interstitial fibrosis, and arteriolopathy were rare findings. Global glomerulosclerosis was found in 3 out of 14 patients whereby patient 7 presented an increased number of globally sclerosed glomeruli (2/43) for his age. Focal minimal interstitial fibrosis was seen in one patient. Fabry arteriopathy in the form of arteriolar lesions with hyaline-like material replacing smooth muscle cells in arterioles occurred in 2 patients. Podocyte inclusions documented by electron microscopy were present in all patients.
All patients, except for one 15-year-old girl (patient 3) with isolated podocyte vacuolization and inclusions without clinical or laboratory features of kidney involvement, presented mild segmental podocyte foot process effacement, comprising less than 50% of the capillary loop circumference. Our investigations revealed that morphological kidney changes are not always associated with clinical and laboratory findings. One child (patient 13), with 8 out of 12 positive light and electron microscopic criteria, solely complained about rare abdominal pain and showed no laboratory abnormalities. On the other hand, while patient 3 showed distinctive clinical features and angiokeratoma, the histology in this case only showed podocyte vacuolization and inclusions. In addition, children without any evident clinical symptoms can manifest severe morphological changes in their biopsies (patient 5a, 5b, and 6).
In one patient (patient 5b), on treatment with agalsidase alfa for 4 years, the follow-up kidney biopsy revealed a complete disappearance of glomerular endothelial cell inclusions. However, an onset of mild interstitial fibrosis and glomerulosclerosis was observed.
To summarize, there was severe vacuolization and accumulation of inclusions in podocytes in all patients, in renal tubules in 13 out of 14 patients, and a combination with segmental foot process effacement was seen in 13 out of 14 patients. Fabry arteriopathy was found in two patients.
Discussion
This study investigates the kidney morphological changes found through biopsies in 15 children with FD as young as 3 years to extend the current data, in particular with focus on the clinical phenotype and initiation of ERT. Earlier studies by Tøndel et al. [2] investigated kidney biopsy findings in children and adolescents with FD in a smaller cohort; all but one were older than 10 years old. Two additional studies analyzing kidney biopsy findings in pediatric FD focused either on foot process effacement [7] or on the correlation between clinical parameters, LysoGb3, podocyturia, and kidney biopsy findings [28].
ERT for FD has been approved by the FDA and the EMA in 2001. Previously published recommendations suggest a treatment initiation as soon as patients present with FD-specific symptoms regardless of age or sex [20]. However, clear guidelines for pediatric FD regarding the appropriate age at which to start ERT are vague. Data on kidney biopsies investigating response to ERT as well as histological evidence of Gb3 accumulation in asymptomatic boys with classical FD suggested to consider beginning ERT around the age of 8–10 years [20, 29]. For asymptomatic girls with FD-causing mutations, primary clinical follow-up is recommended [3, 20, 23, 24]. It is believed that ERT should only be initiated when organs, such as the kidneys, are involved; however, organ screening through kidney biopsies is rarely performed.
Our study evaluated the early diagnosis of Fabry nephropathy in biopsies in correlation to ERT start, applying a semiquantitative scoring, based on a slightly modified version of the scoring protocol published by Tøndel et al. [14]. In contrast to Najafian et al. [30], who applied unbiased stereological quantitative methods to electron microscopic changes of Fabry nephropathy to determine the relationship between parameters of glomerular structure and kidney function, we did not intend to correlate our findings with kidney function.
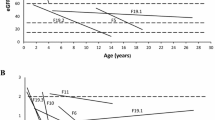
The main finding of our study was that vacuolization of podocytes and podocyte inclusions were found in all biopsy samples independent of genotype, clinical symptoms, age, or gender. Severe vacuolization and accumulation of inclusions in podocytes and renal tubules without laboratory abnormalities were seen in a 3-year-old, indicating that morphological changes of the kidney develop early in life and without organ-specific clinical or laboratory findings (Fig. 1). Interestingly, 80% of the patients did not have any abnormalities in their routine laboratory exams addressing kidney function, proteinuria, and albuminuria. Patients who had concurrent proteinuria or microalbuminuria showed a combination of severe vacuolization and accumulation of inclusions in podocytes, as well as segmental foot process effacement and inclusions in renal tubules in all but 3 patients. Our results rather suggest that the presence of albumin in the urine of patients with FD is a late marker, which might indicate that glomerular cells have already been irreversibly damaged. Similarly, Tøndel et al. [2] have recently demonstrated a broad spectrum of morphological changes including glomerular, tubulointerstitial, and/or vascular impairments. However, compared to the previously published results by Tøndel et al. [2], our results indicate that the kidney involvement begins even earlier.
Kidney biopsy of the youngest patient (3 years old) with vacuolization of cells and glycosphingolipid deposition. A Glomerulus with prominent podocytes with mildly vacuolated cytoplasm (hematoxylin and eosin). B Glomerulus with deposits in the podocytes (methylene blue -azure). C Electron microscopic image of deposits in podocytes (original magnification × 700). D Tubules with vacuolated cells (hematoxylin and eosin). E Deposits in tubular cells (methylene blue -azure). F Electron microscopy of deposits in tubular cells (original magnification × 2000)
We show that in our pediatric cohort, merely the histological evidence of kidney involvement of FD detected through biopsies leads to the initiation of ERT. This suggests that early treatment with ERT should be considered before clinical symptoms, such as proteinuria, occur, in order to prevent possibly irreversible organ damage due to Gb3 accumulation. Risk factors for CKD include low eGFR and albuminuria [17]. It can be assumed that children with classical FD, especially young male patients, develop extensive intracellular Gb3 deposits in the kidneys which triggers a cascade of cellular processes resulting in irreversible kidney damage [16]. Our findings suggest that early diagnostic kidney biopsies should be implemented independent of biochemical findings to facilitate an early indication for ERT in children with FD, taking into consideration results of several studies, which had shown small or no impact of ERT in patients with FD who had moderate to severe kidney disease [15, 31,32,33]. However, the effect of ERT on existing kidney damage is purely understood. Tøndel et al. [14] presented complete clearance of mesangial and glomerular endothelial cell inclusions but only 1/3 of the patients showed substantial or complete clearance of podocytes. On the other hand, Thurberg et al. [18] demonstrated moderate to severe proteinuria or reduced eGFR prior to ERT start, to be negative predictors for efficacy of ERT. A similar result was observed in patient 5b. The biopsy revealed complete clearance of glomerular endothelial cell inclusions, which may be seen as the general treatment effect [2, 14, 18]. However, despite therapy with agalsidase alfa, minimal interstitial fibrosis and glomerulosclerosis developed over time. We postulate that early kidney morphological changes can be reversed with ERT, whereas more severe changes will most probably lead to an aggravation with progressive nephropathy including interstitial fibrosis, glomerulosclerosis, and arteriopathy. Pronounced proteinuria prior to ERT might activate interstitial inflammation and fibrosis resulting in irreversible damage of the kidneys [16, 17, 21, 34,35,36]. Early introduction of an antiproteinuric and antiproliferative treatment is recommended in CKD to reduce progression of kidney disease [37, 38]. A combination of ERT and renin–angiotensin–aldosterone system blockade, should be implemented in FD as soon as a kidney pathology is seen in the biopsy [37, 38].
Further studies are needed to investigate the reversibility of kidney pathology and efficacy of ERT in individual FD patients. Therefore, we will further analyze kidney biopsies in our cohort after 5 years on ERT. This ongoing study will shed light on these important questions. It is essential to investigate the full effect of ERT in kidney disease of children with FD without pathological laboratory findings; the invasiveness of the diagnostic method however must be kept in mind.
Based on our findings of early morphological damages, also supporting earlier studies by Tøndol et al. [2, 7, 14] and Fogo et al. [39], ERT initiation in male classical FD should be considered soon as possible after classical FD is diagnosed. In females and children with late-onset FD, we recommend a kidney biopsy prior to ERT initiation, due to the more variable disease course and different severity [4, 22]. Corresponding to Najafian et al. [22], we assume that pre-ERT and follow-up biopsies in female and late-onset FD patients could help in the assessment of the effectiveness of different ERT dosing schemes. Meanwhile, kidney function should be monitored through regular cystatin C and plasma creatinine measurement for a more precise estimation of the GFR as well as plasma LysoGb3.
Additionally, blood pressure measurements, urine analysis for albuminuria, and kidney biopsies could potentially be used to detect early kidney damage and in turn to prevent disease progression by (1) initiating ERT and/or (2) making ERT dose adjustments.
In conclusion, our results underline and strengthen previous reports that normal standard laboratory assessments of kidney function, as well as the lack of significant classical clinical symptoms, may not exclude glomerular kidney involvement in pediatric patients with FD. Additionally, our analysis showed that kidney histological features (such as vacuolization, inclusions in podocytes and renal tubules) might be prevalently observed also at a very young age. This highlights the necessity for early treatment with ERT, i.e., before histological changes in podocytes appear, to avoid non-reversible organ damage.
Nevertheless, our study has a few limitations. Due to the rarity of FD and the single center setup, the number of individuals included in our cohort is rather small; however, our cohort represents most of the pediatric FD patients treated within Switzerland.
When considering the informative value and significance of podocyte inclusions, in particular in female FD patients, local tissue mosaicism needs to be considered and should be further investigated in future studies. Mauer et al. [40] showed an increased percentage of podocytes without Gb3 inclusions with age, suggesting survival disadvantage for FD podocytes. These findings were confirmed by Najafian et al. [41] even though robust data for females < 10 years of age is still missing.
So far only one patient had a follow-up kidney biopsy on ERT, which is mainly caused by the short period of observation. However, further analysis including more patients and multicenter cohorts are of utmost importance to allow evidence-based treatment recommendations with regards to the best age to start ERT.
Kidney biopsies, especially follow-up biopsies can help in individual decision-making and to investigate the outcome of early kidney biopsy. Incorporating detailed data on kidney morphology before and on treatment regimens, and different dosing of ERT may show that male pediatric patients with FD show the most significant benefit of ERT when treated early in life.
Abbreviations
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- EMA:
-
European Medicines Agency
- ERT:
-
Enzyme replacement therapy
- FD:
-
Fabry disease
- FDA:
-
Food and Drug Administration
- GALA:
-
Alpha-galactosidase A
- Gb3:
-
Globotriaosylceramide
- GLA :
-
Galactosidase alpha gene
References
Ries M, Gupta S, Moore DF, Sachdev V, Quirk JM, Murray GJ, Rosing DR, Robinson C, Schaefer E, Gal A, Dambrosia JM, Garman SC, Brady RO, Schiffmann R (2005) Pediatric Fabry disease. Pediatrics 115:e344-355. https://doi.org/10.1542/peds.2004-1678
Tøndel C, Bostad L, Hirth A, Svarstad E (2008) Renal biopsy findings in children and adolescents with Fabry disease and minimal albuminuria. Am J Kidney Dis 51:767–776. https://doi.org/10.1053/j.ajkd.2007.12.032
Germain DP, Fouilhoux A, Decramer S, Tardieu M, Pillet P, Fila M, Rivera S, Deschênes G, Lacombe D (2019) Consensus recommendations for diagnosis, management and treatment of Fabry disease in paediatric patients. Clin Genet 96:107–117. https://doi.org/10.1111/cge.13546
Arends M, Wanner C, Hughes D, Mehta A, Oder D, Watkinson OT, Elliott PM, Linthorst GE, Wijburg FA, Biegstraaten M, Hollak CE (2017) Characterization of classical and nonclassical Fabry disease: a multicenter study. J Am Soc Nephrol 28:1631–1641. https://doi.org/10.1681/asn.2016090964
Hopkin RJ, Bissler J, Banikazemi M, Clarke L, Eng CM, Germain DP, Lemay R, Tylki-Szymanska A, Wilcox WR (2008) Characterization of Fabry disease in 352 pediatric patients in the Fabry Registry. Pediatr Res 64:550–555. https://doi.org/10.1203/PDR.0b013e318183f132
Eng CM, Fletcher J, Wilcox WR, Waldek S, Scott CR, Sillence DO, Breunig F, Charrow J, Germain DP, Nicholls K, Banikazemi M (2007) Fabry disease: baseline medical characteristics of a cohort of 1765 males and females in the Fabry Registry. J Inherit Metab Dis 30:184–192. https://doi.org/10.1007/s10545-007-0521-2
Tøndel C, Kanai T, Larsen KK, Ito S, Politei JM, Warnock DG, Svarstad E (2015) Foot process effacement is an early marker of nephropathy in young classic Fabry patients without albuminuria. Nephron 129:16–21. https://doi.org/10.1159/000369309
Ramaswami U, Parini R, Pintos-Morell G, Kalkum G, Kampmann C, Beck M, Investigators F (2012) Fabry disease in children and response to enzyme replacement therapy: results from the Fabry Outcome Survey. Clin Genet 81:485–490. https://doi.org/10.1111/j.1399-0004.2011.01671.x
Vedder AC, Strijland A, Weerman MV, Florquin S, Aerts JM, Hollak CE (2006) Manifestations of Fabry disease in placental tissue. J Inherit Metab Dis 29:106–111. https://doi.org/10.1007/s10545-006-0196-0
Ries M, Clarke JT, Whybra C, Mehta A, Loveday KS, Brady RO, Beck M, Schiffmann R (2007) Enzyme replacement in Fabry disease: pharmacokinetics and pharmacodynamics of agalsidase alpha in children and adolescents. J Clin Pharmacol 47:1222–1230. https://doi.org/10.1177/0091270007305299
Ratko TA, Marbella A, Godfrey S, Aronson N (2013) Enzyme-replacement therapies for lysosomal storage diseases. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Jan. Report No.: 12(13)-EHC154-EF. www.effectivehealthcare.ahrq.gov/reports/final.cfm
Juan P, Hernan A, Beatriz SA, Gustavo C, Antonio M, Eduardo T, Raul D, Margarita L, Mariana B, Daniela G, Marina S (2014) Fabry disease: multidisciplinary evaluation after 10 years of treatment with agalsidase Beta. JIMD Rep 16:7–14. https://doi.org/10.1007/8904_2014_310
Desnick RJ (2004) Enzyme replacement therapy for Fabry disease: lessons from two alpha-galactosidase A orphan products and one FDA approval. Expert Opin Biol Ther 4:1167–1176. https://doi.org/10.1517/14712598.4.7.1167
Tøndel C, Bostad L, Larsen KK, Hirth A, Vikse BE, Houge G, Svarstad E (2013) Agalsidase benefits renal histology in young patients with Fabry disease. J Am Soc Nephrol 24:137–148. https://doi.org/10.1681/asn.2012030316
Germain DP, Waldek S, Banikazemi M, Bushinsky DA, Charrow J, Desnick RJ, Lee P, Loew T, Vedder AC, Abichandani R, Wilcox WR, Guffon N (2007) Sustained, long-term renal stabilization after 54 months of agalsidase beta therapy in patients with Fabry disease. J Am Soc Nephrol 18:1547–1557. https://doi.org/10.1681/asn.2006080816
Rozenfeld P, Feriozzi S (2017) Contribution of inflammatory pathways to Fabry disease pathogenesis. Mol Genet Metab 122:19–27. https://doi.org/10.1016/j.ymgme.2017.09.004
Gansevoort RT, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Chronic Kidney Disease Prognosis Consortium (2011) Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int 80:93–104. https://doi.org/10.1038/ki.2010.531
Thurberg BL, Rennke H, Colvin RB, Dikman S, Gordon RE, Collins AB, Desnick RJ, O’Callaghan M (2002) Globotriaosylceramide accumulation in the Fabry kidney is cleared from multiple cell types after enzyme replacement therapy. Kidney Int 62:1933–1946. https://doi.org/10.1046/j.1523-1755.2002.00675.x
Gubler MC, Lenoir G, Grünfeld JP, Ulmann A, Droz D, Habib R (1978) Early renal changes in hemizygous and heterozygous patients with Fabry’s disease. Kidney Int 13:223–235. https://doi.org/10.1038/ki.1978.32
Hopkin RJ, Jefferies JL, Laney DA, Lawson VH, Mauer M, Taylor MR, Wilcox WR, Fabry Pediatric Expert Panel (2016) The management and treatment of children with Fabry disease: a United States-based perspective. Mol Genet Metab 117:104–113. https://doi.org/10.1016/j.ymgme.2015.10.007
Levstek T, Vujkovac B, Trebusak Podkrajsek K (2020) Biomarkers of Fabry nephropathy: review and future perspective. Genes (Basel) 11:1091. https://doi.org/10.3390/genes11091091
Najafian B, Mauer M, Hopkin RJ, Svarstad E (2013) Renal complications of Fabry disease in children. Pediatr Nephrol 28:679–687. https://doi.org/10.1007/s00467-012-2222-9
Germain DP, Hughes DA, Nicholls K, Bichet DG, Giugliani R, Wilcox WR, Feliciani C, Shankar SP, Ezgu F, Amartino H, Bratkovic D, Feldt-Rasmussen U, Nedd K, Sharaf El Din U, Lourenco CM, Banikazemi M, Charrow J, Dasouki M, Finegold D, Giraldo P, Goker-Alpan O, Longo N, Scott CR, Torra R, Tuffaha A, Jovanovic A, Waldek S, Packman S, Ludington E, Viereck C, Kirk J, Yu J, Benjamin ER, Johnson F, Lockhart DJ, Skuban N, Castelli J, Barth J, Barlow C, Schiffmann R (2016) Treatment of Fabry’s disease with the pharmacologic chaperone Migalastat. N Engl J Med 375:545–555. https://doi.org/10.1056/NEJMoa1510198
Germain DP, Giugliani R, Hughes DA, Mehta A, Nicholls K, Barisoni L, Jennette CJ, Bragat A, Castelli J, Sitaraman S, Lockhart DJ, Boudes PF (2012) Safety and pharmacodynamic effects of a pharmacological chaperone on α-galactosidase A activity and globotriaosylceramide clearance in Fabry disease: report from two phase 2 clinical studies. Orphanet J Rare Dis 7:91. https://doi.org/10.1186/1750-1172-7-91
Beck M (2006) The Mainz Severity Score Index (MSSI): development and validation of a system for scoring the signs and symptoms of Fabry disease. Acta Paediatr Suppl 95:43–46. https://doi.org/10.1080/08035320600618825
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/asn.2008030287
Ramaswami U, Bichet DG, Clarke LA, Dostalova G, Fainboim A, Fellgiebel A, Forcelini CM, An Haack K, Hopkin RJ, Mauer M, Najafian B, Scott CR, Shankar SP, Thurberg BL, Tøndel C, Tylki-Szymanska A, Bénichou B, Wijburg FA (2019) Low-dose agalsidase beta treatment in male pediatric patients with Fabry disease: a 5-year randomized controlled trial. Mol Genet Metab 127:86–94. https://doi.org/10.1016/j.ymgme.2019.03.010
Politei J, Alberton V, Amoreo O, Antongiovanni N, Arán MN, Barán M, Cabrera G, Di Pietrantonio S, Durand C, Fainboim A, Frabasil J, Pizarro FG, Iotti R, Liern M, Perretta F, Ripeau D, Toniolo F, Trimarchi H, Rivas DV, Wallace E, Schenone AB (2018) Clinical parameters, LysoGb3, podocyturia, and kidney biopsy in children with Fabry disease: is a correlation possible? Pediatr Nephrol 33:2095–2101. https://doi.org/10.1007/s00467-018-4006-3
Wijburg FA, Bénichou B, Bichet DG, Clarke LA, Dostalova G, Fainboim A, Fellgiebel A, Forcelini C, An Haack K, Hopkin RJ, Mauer M, Najafian B, Scott CR, Shankar SP, Thurberg BL, Tøndel C, Tylki-Szymańska A, Ramaswami U (2015) Characterization of early disease status in treatment-naive male paediatric patients with Fabry disease enrolled in a randomized clinical trial. PLoS One 10:e0124987. https://doi.org/10.1371/journal.pone.0124987
Najafian B, Svarstad E, Bostad L, Gubler MC, Tøndel C, Whitley C, Mauer M (2011) Progressive podocyte injury and globotriaosylceramide (GL-3) accumulation in young patients with Fabry disease. Kidney Int 79:663–670. https://doi.org/10.1038/ki.2010.484
Banikazemi M, Bultas J, Waldek S, Wilcox WR, Whitley CB, McDonald M, Finkel R, Packman S, Bichet DG, Warnock DG, Desnick RJ; Fabry Disease Clinical Trial Study Group (2007) Agalsidase-beta therapy for advanced Fabry disease: a randomized trial. Ann Intern Med 146:77–86. https://doi.org/10.7326/0003-4819-146-2-200701160-00148
West M, Nicholls K, Mehta A, Clarke JT, Steiner R, Beck M, Barshop BA, Rhead W, Mensah R, Ries M, Schiffmann R (2009) Agalsidase alfa and kidney dysfunction in Fabry disease. J Am Soc Nephrol 20:1132–1139. https://doi.org/10.1681/asn.2008080870
Breunig F, Weidemann F, Strotmann J, Knoll A, Wanner C (2006) Clinical benefit of enzyme replacement therapy in Fabry disease. Kidney Int 69:1216–1221. https://doi.org/10.1038/sj.ki.5000208
Waldek S, Feriozzi S (2014) Fabry nephropathy: a review - how can we optimize the management of Fabry nephropathy? BMC Nephrol 15:72. https://doi.org/10.1186/1471-2369-15-72
Ortiz A, Oliveira JP, Waldek S, Warnock DG, Cianciaruso B, Wanner C, Registry F (2008) Nephropathy in males and females with Fabry disease: cross-sectional description of patients before treatment with enzyme replacement therapy. Nephrol Dial Transplant 23:1600–1607. https://doi.org/10.1093/ndt/gfm848
Ortiz A, Oliveira JP, Wanner C, Brenner BM, Waldek S, Warnock DG (2008) Recommendations and guidelines for the diagnosis and treatment of Fabry nephropathy in adults. Nat Clin Pract Nephrol 4:327–336. https://doi.org/10.1038/ncpneph0806
Brewster UC, Perazella MA (2004) The renin-angiotensin-aldosterone system and the kidney: effects on kidney disease. Am J Med 116:263–272. https://doi.org/10.1016/j.amjmed.2003.09.034
Tahir H, Jackson LL, Warnock DG (2007) Antiproteinuric therapy and fabry nephropathy: sustained reduction of proteinuria in patients receiving enzyme replacement therapy with agalsidase-beta. J Am Soc Nephrol 18:2609–2617. https://doi.org/10.1681/asn.2006121400
Fogo AB, Bostad L, Svarstad E, Cook WJ, Moll S, Barbey F, Geldenhuys L, West M, Ferluga D, Vujkovac B, Howie AJ, Burns A, Reeve R, Waldek S, Noël LH, Grünfeld JP, Valbuena C, Oliveira JP, Müller J, Breunig F, Zhang X, Warnock DG, all members of the International Study Group of Fabry Nephropathy (ISGFN) (2010) Scoring system for renal pathology in Fabry disease: report of the International Study Group of Fabry Nephropathy (ISGFN). Nephrol Dial Transplant 25:2168–2177. https://doi.org/10.1093/ndt/gfp528
Mauer M, Glynn E, Svarstad E, Tøndel C, Gubler MC, West M, Sokolovskiy A, Whitley C, Najafian B (2014) Mosaicism of podocyte involvement is related to podocyte injury in females with Fabry disease. PLoS One 9:e112188. https://doi.org/10.1371/journal.pone.0112188
Najafian B, Silvestroni A, Sokolovskiy A, Tøndel C, Svarstad E, Obrisca B, Ismail G, Holida MD, Mauer M (2022) A novel unbiased method reveals progressive podocyte globotriaosylceramide accumulation and loss with age in females with Fabry disease. Kidney Int 102:173–182. https://doi.org/10.1016/j.kint.2022.03.023
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Contributions
Jenny Avarappattu, Marianne Rohrbach, and Giuseppina Spartà contributed to the study conception and design. Jenny Avarappattu analyzed the data and made the tables. Ariana Gaspert analyzed the kidney biopsies and made the figures. Marianne Rohrbach and Giuseppina Spartà contributed equally to the paper. The first draft of the manuscript was written by Jenny Avarappattu and all authors commented on previous versions of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Avarappattu, J., Gaspert, A., Spartà, G. et al. Impact of kidney biopsy on deciding when to initiate enzyme replacement therapy in children with Fabry disease. Pediatr Nephrol 39, 131–140 (2024). https://doi.org/10.1007/s00467-023-06050-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06050-5