Abstract
Background
Studies in adults have shown that persistent kidney dysfunction ≥7–90 days following acute kidney injury (AKI), termed acute kidney disease (AKD), increases chronic kidney disease (CKD) and mortality risk. Little is known about the factors associated with the transition of AKI to AKD and the impact of AKD on outcomes in children. The aim of this study is to evaluate risk factors for progression of AKI to AKD in hospitalized children and to determine if AKD is a risk factor for CKD.
Methods
Retrospective cohort study of children age ≤18 years admitted with AKI to all pediatric units at a single tertiary-care children’s hospital between 2015 and 2019. Exclusion criteria included insufficient serum creatinine values to evaluate for AKD, chronic dialysis, or previous kidney transplant.
Results
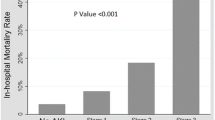
A total of 528 children with AKI were included in the study. There were 297 (56.3%) hospitalized AKI survivors who developed AKD. Among children with AKD, 45.5% developed CKD compared to 18.7% in the group without AKD (OR 4.0, 95% CI 2.1–7.4, p-value <0.001 using multivariable logistic regression analysis including other covariates). Multivariable logistic regression model identified age at AKI diagnosis, PCICU and NICU admission, prematurity, malignancy, bone marrow transplant, previous AKI, mechanical ventilation, AKI stage, duration of kidney injury, and need for kidney replacement therapy during day 1–7 as risk factors for AKD after AKI.
Conclusions
AKD is common among hospitalized children with AKI and multiple risk factors are associated with AKD. Children that progress from AKI to AKD are at higher risk of developing CKD.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
Data availability
All data are stored according to the Duke University Institutional Review Board approval and are available upon request.
References
McGregor TL, Jones DP, Wang L et al (2016) Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am J Kidney Dis 67:384–390. https://doi.org/10.1053/j.ajkd.2015.07.019
Kaddourah A, Basu RK, Bagshaw SM et al (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMoa1611391
Williams DM, Sreedhar SS, Mickell JJ, Chan JCM (2002) Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med 156:893–900. https://doi.org/10.1001/archpedi.156.9.893
Sutherland SM, Ji J, Sheikhi FH et al (2013) AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol 8:1661–1669. https://doi.org/10.2215/CJN.00270113
Alkandari O, Eddington KA, Hyder A et al (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 15:R146. https://doi.org/10.1186/cc10269
Mammen C, Al Abbas A, Skippen P et al (2012) Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis 59:523–530. https://doi.org/10.1053/j.ajkd.2011.10.048
Atkinson MA, Warady BA (2018) Anemia in chronic kidney disease. Pediatr Nephrol 33:227–238. https://doi.org/10.1007/s00467-017-3663-y
Hruska KA, Sugatani T, Agapova O, Fang Y (2017) The chronic kidney disease - Mineral bone disorder (CKD-MBD): Advances in pathophysiology. Bone 100:80–86. https://doi.org/10.1016/j.bone.2017.01.023
Drube J, Wan M, Bonthuis M et al (2019) Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol 15:577–589. https://doi.org/10.1038/s41581-019-0161-4
Chen K, Didsbury M, van Zwieten A et al (2018) Neurocognitive and Educational Outcomes in Children and Adolescents with CKD: A Systematic Review and Meta-Analysis. Clin J Am Soc Nephrol 13:387–397. https://doi.org/10.2215/CJN.09650917
Jankowski J, Floege J, Fliser D et al (2021) Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation 143:1157–1172. https://doi.org/10.1161/CIRCULATIONAHA.120.050686
Lameire NH, Levin A, Kellum JA et al (2021) Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int 100:516–526. https://doi.org/10.1016/j.kint.2021.06.028
Patel M, Heipertz A, Joyce E et al (2021) Acute kidney disease predicts chronic kidney disease in pediatric non-kidney solid organ transplant patients. Pediatr Transplant 26:e14172. https://doi.org/10.1111/petr.14172
LoBasso M, Schneider J, Sanchez-Pinto LN et al (2022) Acute kidney injury and kidney recovery after cardiopulmonary bypass in children. Pediatr Nephrol 37:659–665. https://doi.org/10.1007/s00467-021-05179-5
Namazzi R, Batte A, Opoka RO et al (2022) Acute kidney injury, persistent kidney disease, and post-discharge morbidity and mortality in severe malaria in children: a prospective cohort study. EClinicalMedicine 44:101292. https://doi.org/10.1016/j.eclinm.2022.101292
Deng Y-H, Yan P, Zhang N-Y et al (2022) Acute kidney disease in hospitalized pediatric patients with acute kidney injury in china. Front Pediatr 10:885055. https://doi.org/10.3389/fped.2022.885055
Daraskevicius J, Azukaitis K, Dziugeviciute-Tupko J et al (2020) Phenotypes and baseline risk factors of acute kidney injury in children after allogeneic hematopoietic stem cell transplantation. Front Pediatr 8:499. https://doi.org/10.3389/fped.2020.00499
Sigurjonsdottir VK, Chaturvedi S, Mammen C, Sutherland SM (2018) Pediatric acute kidney injury and the subsequent risk for chronic kidney disease: is there cause for alarm? Pediatr Nephrol 33:2047–2055. https://doi.org/10.1007/s00467-017-3870-6
Menon S, Kirkendall ES, Nguyen H, Goldstein SL (2014) Acute kidney injury associated with high nephrotoxic medication exposure leads to chronic kidney disease after 6 months. J Pediatr 165:522–527.e2. https://doi.org/10.1016/j.jpeds.2014.04.058
Schwartz GJ, Muñoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Zappitelli M, Parikh CR, Akcan-Arikan A et al (2008) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954. https://doi.org/10.2215/CJN.05431207
Carmody JB, Swanson JR, Rhone ET, Charlton JR (2014) Recognition and reporting of AKI in very low birth weight infants. Clin J Am Soc Nephrol 9:2036–2043. https://doi.org/10.2215/CJN.05190514
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120:c179–c184. https://doi.org/10.1159/000339789
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Workgroup (2013) KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 3:1–150
Basu RK, Zappitelli M, Brunner L et al (2014) Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int 85:659–667. https://doi.org/10.1038/ki.2013.349
Yaradilmiş RM, Öztürk B, Güngör A et al (2023) Success of the acute renal angina index in the early prediction of acute kidney injury in the emergency department. Acta Clin Belg 78:51–57. https://doi.org/10.1080/17843286.2022.2031667
Gist KM, SooHoo M, Mack E et al (2022) Modifying the renal angina index for predicting AKI and related adverse outcomes in pediatric heart surgery. World J Pediatr Congenit Heart Surg 13:196–202. https://doi.org/10.1177/21501351211073615
Menon S, Tarrago R, Carlin K et al (2021) Impact of integrated clinical decision support systems in the management of pediatric acute kidney injury: a pilot study. Pediatr Res 89:1164–1170. https://doi.org/10.1038/s41390-020-1046-8
Goldstein SL, Dahale D, Kirkendall ES et al (2020) A prospective multi-center quality improvement initiative (NINJA) indicates a reduction in nephrotoxic acute kidney injury in hospitalized children. Kidney Int 97:580–588. https://doi.org/10.1016/j.kint.2019.10.015
Funding
MP was supported by National Institutes of Health Nephrology Training Grant (5T32DK007731-24).
Author information
Authors and Affiliations
Contributions
MP, CH, CD, DS, and RG designed the study. MP gathered clinical data for the study. MP and CH carried out the data analysis. MP wrote the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Duke University Institutional Review Board.
Competing interests
CJD reports consultancy with UnitedHealth Group/Optum Labs. Other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, M., Hornik, C., Diamantidis, C. et al. Patient level factors increase risk of acute kidney disease in hospitalized children with acute kidney injury. Pediatr Nephrol 38, 3465–3474 (2023). https://doi.org/10.1007/s00467-023-05997-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05997-9