Abstract
Background
Optimal steroid treatment at onset of idiopathic nephrotic syndrome is still debated. The aim of this study was to analyze the clinical outcome at 24 months of follow-up in patients admitted to our unit for the first episode of steroid-sensitive nephrotic syndrome comparing two different steroid regimens.
Methods
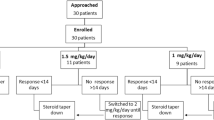
We collected data on patients treated from 1992 to 2007 with prednisone according to the International Study on Kidney Diseases in Children 8-week regimen and since 2008 according to the Arbeitsgemeinschaft fur Padiatrische Nephrologie 12-week regimen. The primary outcome was to evaluate cumulative prednisone dosage at 12 and 24 months of follow-up in the two groups. As secondary outcomes, we considered mean relapse rate per patient; number of children without relapses at 6, 12, and 24 months; and number of patients who developed frequent relapses and steroid-dependent disease.
Results
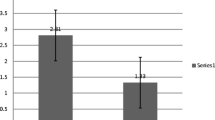
Data were collected on 127 patients. Sixty-one subjects received the 8-week regimen and 66 the 12-week regimen. The mean cumulative prednisone dose at 12 and 24 months was not different, and the rate of patients without relapses was lower at 6 and 12 months in patients treated with the 8-week course, while no difference was observed at 24 months.
Conclusions
Despite the limitations of a retrospective study with limited follow-up, our data indicate that switching treatment from a shorter to a longer scheme did not improve the clinical outcome at 24 months of observation.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Abbreviations
- INS:
-
Idiopathic nephrotic syndrome
- SSNS:
-
Steroid-sensitive nephrotic syndrome
- FRNS:
-
Frequently relapsing nephrotic syndrome
- SDNS:
-
Steroid-dependent nephrotic syndrome
- ISKDC:
-
International Study on Kidney Diseases in Children
- PDN:
-
Prednisone
- APN:
-
Arbeitsgemeinschaft fur Padiatrische Nephrologie
- 8W:
-
8 Weeks
- 12W:
-
12 Weeks
- MMF:
-
Mycophenolate mofetil
- RCTs:
-
Randomized controlled studies
References
Dossier C, Delbet JD, Boyer O, Daoud P, Mesples B, Pellegrino B, See H, Benoist G, Chace A, Larakeb A, Hogan J, Deschênes G (2019) Five-year outcome of children with idiopathic nephrotic syndrome: the NEPHROVIR population-based cohort study. Pediatr Nephrol 34:671–678. https://doi.org/10.1007/s00467-018-4149-2
Noone DG, Iijima K, Parekh R (2018) Idiopathic nephrotic syndrome in children. Lancet 392:61–74. https://doi.org/10.1016/S0140-6736(18)31608-8
Koskimies O, Vilska J, Rapola J, Hallman N (1982) Long-term outcome of primary nephrotic syndrome. Arch Dis Child 57:544–548. https://doi.org/10.1136/adc.57.7.544
Webb NJA, Woolley RL, Lambe T, Frew E, Brettell EA, Barsoum EN, Trompeter RS, Cummins C, Deeks JJ, Wheatley K, Ives NJ; PREDNOS Collaborative Group (2019) Long term tapering versus standard prednisolone treatment for first episode of childhood nephrotic syndrome: phase III randomised controlled trial and economic evaluation. BMJ 365:l1800. https://doi.org/10.1136/bmj.l1800
Vivarelli M, Massella L, Ruggiero B, Emma F (2017) Minimal change disease. Clin J Am Soc Nephrol 12:332–345. https://doi.org/10.2215/CJN.05000516
Carter SA, Mistry S, Fitzpatrick J, Banh T, Hebert D, Langlois V, Pearl RJ, Chanchlani R, Licht CPB, Radhakrishnan S, Brooke J, Reddon J, Levin L, Aitken-Menezes K, Noone D, Parekh RS (2020) Prediction of short- and long-term outcomes in childhood nephrotic syndrome. Kidney Int Rep 5:426–434. https://doi.org/10.1016/j.ekir.2019.12.015
Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776. https://doi.org/10.1681/ASN.V85769
Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF, Landais P, Lesavre P, Chauveau D, Knebelmann B, Broyer M, Grünfeld JP, Niaudet P (2003) Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis 41:550–557. https://doi.org/10.1053/ajkd.2003.50116
(1981) Primary nephrotic syndrome in children: clinical significance of histopathologic variants of minimal change and of diffuse mesangial hypercellularity. A Report of the International Study of Kidney Disease in Children. Kidney Int 20:765–771. https://doi.org/10.1038/ki.1981.209
Ehrich JH, Brodehl J (1993) Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Eur J Pediatr 152:357–361. https://doi.org/10.1007/BF01956754
Sinha A, Saha A, Kumar M, Sharma S, Afzal K, Mehta A, Kalaivani M, Hari P, Bagga A (2015) Extending initial prednisolone treatment in a randomized control trial from 3 to 6 months did not significantly influence the course of illness in children with steroid-sensitive nephrotic syndrome. Kidney Int 87:214–224. https://doi.org/10.1038/ki.2014.240
Yoshikawa N, Nakanishi K, Sako M, Oba MS, Mori R, Ota E, Ishikura K, Hataya H, Honda M, Ito S, Shima Y, Kaito H, Nozu K, Nakamura H, Igarashi T, Ohashi Y, Iijima K; Japanese Study Group of Kidney Disease in Children (2015) A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment. Kidney Int 87:225–232. https://doi.org/10.1038/ki.2014.260
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group (2012) KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2:139–274
Schijvens AM, Teeninga N, Dorresteijn EM, Teerenstra S, Webb NJ, Schreuder MF (2021) Steroid treatment for the first episode of childhood nephrotic syndrome: comparison of the 8 and 12 weeks regimen using an individual patient data meta-analysis. Eur J Pediatr 180:2849–2859. https://doi.org/10.1007/s00431-021-04035-w
Williams AE, Gbadegesin RA (2021) Steroid regimen for children with nephrotic syndrome relapse. Clin J Am Soc Nephrol 16:179–181. https://doi.org/10.2215/CJN.19201220
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int 100:S1–S276. https://doi.org/10.1016/j.kint.2021.05.021
Hahn D, Samuel SM, Willis NS, Craig JC, Hodson EM (2020) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev 2020:CD001533. https://doi.org/10.1002/14651858.CD001533.pub6
Hiraoka M, Tsukahara H, Matsubara K, Tsurusawa M, Takeda N, Haruki S, Hayashi S, Ohta K, Momoi T, Ohshima Y, Suganuma N, Mayumi M; West Japan Cooperative Study Group of Kidney Disease in Children (2003) A randomized study of two long course prednisolone regimens for nephrotic syndrome in children. Am J Kidney Dis 41:1155–1162. https://doi.org/10.1016/s0272-6386(03)00346-9
Andersen RF, Thrane N, Noergaard K, Rytter L, Jespersen B, Rittig S (2010) Early age at debut is a predictor of steroid-dependent and frequent relapsing nephrotic syndrome. Pediatr Nephrol 25:1299–1304. https://doi.org/10.1007/s00467-010-1537-7
Sato M, Ishikura K, Ando T, Kikunaga K, Terano C, Hamada R, Ishimori S, Hamasaki Y, Araki Y, Gotoh Y, Nakanishi K, Nakazato H, Matsuyama T, Iijima K, Yoshikawa N, Ito S, Honda M (2019) Prognosis and acute complications at the first onset of idiopathic nephrotic syndrome in children: a nationwide survey in Japan (JP-SHINE study). Nephrol Dial Transplant 36:475–481. https://doi.org/10.1093/ndt/gfz185.gfz185
Hoyer PF (2015) New lessons from randomized trials in steroid-sensitive nephrotic syndrome: clear evidence against long steroid therapy. Kidney Int 87:17–19. https://doi.org/10.1038/ki.2014.354
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lucchetti, L., Gatto, A., Gianviti, A. et al. Treatment of idiopathic nephrotic syndrome at onset: a comparison between 8- and 12-week regimens in everyday clinical practice. Pediatr Nephrol 38, 2101–2106 (2023). https://doi.org/10.1007/s00467-022-05824-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05824-7