Abstract
Background
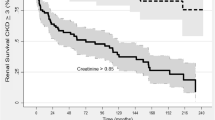
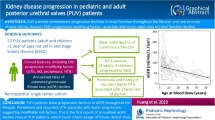
Posterior urethral valve (PUV) is a leading cause of chronic kidney failure in children. Studies have shown that a creatinine nadir above historical cutoff values of 0.8 or 1.0 mg/dL correlates with worse kidney outcomes. The ability to use nadir creatinine more discriminately as a test of kidney outcomes is otherwise limited.
Methods
We performed a retrospective review of 102 infants treated with primary valve ablation prior to 1 year of age. Patient factors including creatinine at presentation (Cr-P), nadir within 6 weeks after ablation (Cr-6 W), and nadir within 1 year after ablation (Cr-1Y) were assessed as predictors of final chronic kidney disease (CKD) severity. An optimal threshold for four CKD levels was defined in incremental fashion using binary outcome with receiver operating characteristic (ROC). Multivariable logistic regression models compared Cr-P, Cr-6 W, and Cr-1Y while adjusting for patient factors.
Results
Boys were ablated at mean age of 36.3 days and followed for 6.6 years (± 3.7). When compared to other demographics, only creatinine remained independently predictive of CKD outcomes on multivariable analysis. ROC analysis demonstrated excellent diagnostic accuracy for Cr-6 W and Cr-1Y (p < 0.001) and acceptable accuracy for Cr-P (p < 0.005). Using the Cr-6 W and Cr-1Y models, high sensitivity and specificity creatinine nadir cutoffs were determined to predict each CKD outcome.
Conclusions
The severity of childhood CKD can be predicted with high accuracy using the creatinine nadir within 6 weeks of ablation. The cutoff values described can be incorporated into a clinical setting for patient counseling and individual risk stratification.
Graphical abstract


Similar content being viewed by others
References
Brownlee E, Wragg R, Robb A, Chandran H, Knight M, McCarthy L, BAPS-CASS (2019) Current epidemiology and antenatal presentation of posterior urethral valves: outcome of BAPS CASS National Audit. J Pediatr Surg 54:318–321
Caione P, Nappo SG (2011) Posterior urethral valves: long-term outcome. Pediatr Surg Int 27:1027–1035
Coleman R, King T, Nicoara CD, Bader M, McCarthy L, Chandran H, Parashar K (2015) Nadir creatinine in posterior urethral valves: how high is low enough? J Pediatr Urol 11(356):e351-355
Sarhan OM, El-Ghoneimi AA, Helmy TE, Dawaba MS, Ghali AM, el Ibrahiem HI (2011) Posterior urethral valves: multivariate analysis of factors affecting the final renal outcome. J Urol 185:2491–2495
Bilgutay AN, Roth DR, Gonzales ET Jr, Janzen N, Zhang W, Koh CJ, Gargollo P, Seth A (2016) Posterior urethral valves: risk factors for progression to renal failure. J Pediatr Urol 12(179):e171-177
Coquillette M, Lee RS, Pagni SE, Cataltepe S, Stein DR (2020) Renal outcomes of neonates with early presentation of posterior urethral valves: a 10-year single center experience. J Perinatol 40:112–117
Warshaw BL, Hymes LC, Trulock TS, Woodard JR (1985) Prognostic features in infants with obstructive uropathy due to posterior urethral valves. J Urol 133:240–243
DeFoor W, Clark C, Jackson E, Reddy P, Minevich E, Sheldon C (2008) Risk factors for end stage renal disease in children with posterior urethral valves. J Urol 180:1705–1708; discussion 1708
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Ansari MS, Gulia A, Srivastava A, Kapoor R (2010) Risk factors for progression to end-stage renal disease in children with posterior urethral valves. J Pediatr Urol 6:261–264
Kousidis G, Thomas DF, Morgan H, Haider N, Subramaniam R, Feather S (2008) The long-term outcome of prenatally detected posterior urethral valves: a 10 to 23-year follow-up study. BJU Int 102:1020–1024
Hennus PM, van der Heijden GJ, Bosch JL, de Jong TP, de Kort LM (2012) A systematic review on renal and bladder dysfunction after endoscopic treatment of infravesical obstruction in boys. PLoS One 7:e44663
Duckett JW (1983) Management of posterior urethral valves. AUA Weekly Update Series 2
Hulbert WC, Duckett JW (1988) Current views on posterior urethral valves. Pediatr Ann 17:31–36
Rittenberg MH, Hulbert WC, Snyder HM 3rd, Duckett JW (1988) Protective factors in posterior urethral valves. J Urol 140:993–996
Lopez Pereira P, Espinosa L, Martinez Urrutina MJ, Lobato R, Navarro M, Jaureguizar E (2003) Posterior urethral valves: prognostic factors. BJU Int 91:687–690
Pohl M, Mentzel HJ, Vogt S, Walther M, Ronnefarth G, John U (2012) Risk factors for renal insufficiency in children with urethral valves. Pediatr Nephrol 27:443–450
Denes ED, Barthold JS, Gonzalez R (1997) Early prognostic value of serum creatinine levels in children with posterior urethral valves. J Urol 157:1441–1443
Demirkan H, Yesildal C (2020) Serum creatinine levels in cases of posterior urethral valve: 29 years experience of a pediatric urology reference center. Low Urin Tract Symptoms 12:274–277
Vasconcelos MA, Silva ACSE, Gomes IR, Carvalho RA, Pinheiro SV, Colosimo EA, Yorgin P, Mak RH, Oliveira EA (2019) A clinical predictive model of chronic kidney disease in children with posterior urethral valves. Pediatr Nephrol 34:283–294
Onuora VC, Mirza K, Koko AH, Al Turki M, Meabed AH, Al Jawini N (2000) Prognostic factors in Saudi children with posterior urethral valves. Pediatr Nephrol 14:221–223
Deshpande AV, Alsaywid BS, Smith GH (2011) Setting the speed limit: a pilot study of the rate of serum creatinine decrease after endoscopic valve ablation in neonates. J Urol 185:2497–2500
Churchill BM, Khoury AE, McLorie GA (1989) Posterior urethral valves. Acta Urol Belg 57:435–449
Sarhan O, El-Dahshan K, Sarhan M (2010) Prognostic value of serum creatinine levels in children with posterior urethral valves treated by primary valve ablation. J Pediatr Urol 6:11–14
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, C.Q., Blum, E.S., Patil, D. et al. Predicting childhood chronic kidney disease severity in infants with posterior urethral valve: a critical analysis of creatinine values in the first year of life. Pediatr Nephrol 37, 1339–1345 (2022). https://doi.org/10.1007/s00467-021-05271-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05271-w