Abstract
Background
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease, especially in children. Owing to the short-term observational period and the small number of patients analyzed in previous reports, the long-term clinical and laboratory characteristics and renal prognosis of children with TINU syndrome remain unclear.
Methods
In this retrospective observational study, we enrolled 29 children with TINU syndrome from February 1990 to February 2019.
Results
During the median follow-up duration of 38 months, the kidney function, urinary β2 microglobulin-creatinine ratio (U-β2MG/Cr), and uveitis in the patients had significantly improved at 24, 6, and 36 months after diagnosis. Higher U-β2MG/Cr was associated with longer duration of kidney function normalization. Half of the patients required uveitis treatment for 5 years after the diagnosis.
Conclusions
Patients with severe low-molecular weight proteinuria at diagnosis needed a longer duration to achieve improvements in kidney function. Uveitis has a much longer treatment period than tubulointerstitial nephritis. This study demonstrates the good prognosis of children with TINU syndrome in terms of their long-term clinical and laboratory characteristics.
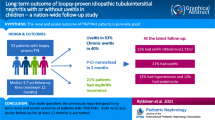
Graphical abstract




Similar content being viewed by others
References
Dobrin RS, Vernier RL, Fish AL (1975) Acute eosinophilic interstitial nephritis and renal failure with bone marrow-lymph node granulomas and anterior uveitis. A new syndrome. Am J Med 59:325–333. https://doi.org/10.1016/0002-9343(75)90390-3
Clive DM, Vanguri VK (2018) The syndrome of tubulointerstitial nephritis with uveitis (TINU). Am J Kidney Dis 72:118–128. https://doi.org/10.1053/j.ajkd.2017.11.013
Mandeville JT, Levinson RD, Holland GN (2001) The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol 46:195–208. https://doi.org/10.1016/s0039-6257(01)00261-2
Tan Y, Yu F, Qu Z, Su T, Xing GQ, Wu LH, Wang FM, Liu G, Yang L, Zhao MH (2011) Modified C-reactive protein might be a target autoantigen of TINU syndrome. Clin J Am Soc Nephrol 6:93–100. https://doi.org/10.2215/CJN.09051209
Saarela V, Nuutinen M, Ala-Houhala M, Arikoski P, Ronnholm K, Jahnukainen T (2013) Tubulointerstitial nephritis and uveitis syndrome in children: a prospective multicenter study. Ophthalmology 120:1476–1481. https://doi.org/10.1016/j.ophtha.2012.12.039
Jahnukainen T, Ala-Houhala M, Karikoski R, Kataja J, Saarela V, Nuutinen M (2011) Clinical outcome and occurrence of uveitis in children with idiopathic tubulointerstitial nephritis. Pediatr Nephrol 26:291–299. https://doi.org/10.1007/s00467-010-1698-4
Takemura T, Okada M, Hino S, Fukushima K, Yamamoto S, Miyazato H, Maruyama K, Yoshioka K (1999) Course and outcome of tubulointerstitial nephritis and uveitis syndrome. Am J Kidney Dis 34:1016–1021. https://doi.org/10.1016/S0272-6386(99)70006-5
Tanaka H, Suzuki K, Nakahata T, Tateyama T, Waga S, Ito E (2001) Repeat renal biopsy in a girl with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 16:885–887. https://doi.org/10.1007/s004670100697
Hibi Y, Uemura O, Nagai T, Yamakawa S, Yamasaki Y, Yamamoto M, Nakano M, Kasahara K (2015) The ratios of urinary beta2-microglobulin and NAG to creatinine vary with age in children. Pediatr Int 57:79–84. https://doi.org/10.1111/ped.12470
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Fisher DA (2000) The importance of early management in optimizing IQ in infants with congenital hypothyroidism. J Pediatr 136:273–274. https://doi.org/10.1067/mpd.2000.104286
Suzuki K, Tanaka H, Ito E, Waga S (2004) Repeat renal biopsy in children with severe idiopathic tubulointerstitial nephritis. Pediatr Nephrol 19:240–243. https://doi.org/10.1007/s00467-003-1362-3
Yanagihara T, Kitamura H, Aki K, Kuroda N, Fukunaga Y (2009) Serial renal biopsies in three girls with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 24:1159–1164. https://doi.org/10.1007/s00467-009-1142-9
Kanno H, Ishida K, Yamada W, Shiraki I, Murase H, Yamagishi Y, Mochizuki K (2018) Clinical and genetic features of tubulointerstitial nephritis and uveitis syndrome with long-term follow-Up. J Ophthalmol 2018:4586532. https://doi.org/10.1155/2018/4586532
Li C, Su T, Chu R, Li X, Yang L (2014) Tubulointerstitial nephritis with uveitis in Chinese adults. Clin J Am Soc Nephrol 9:21–28. https://doi.org/10.2215/CJN.02540313
Zeng X, Hossain D, Bostwick DG, Herrera GA, Zhang PL (2014) Urinary β2-microglobulin is a good indicator of proximal tubule injury: a correlative study with renal biopsies. J Biomark 2014:492838. https://doi.org/10.1155/2014/492838
Pakzad-Vaezi K, Pepple KL (2017) Tubulointerstitial nephritis and uveitis. Curr Opin Ophthalmol 28:629–635. https://doi.org/10.1097/ICU.0000000000000421
Kase S, Kitaichi N, Namba K, Miyazaki A, Yoshida K, Ishikura K, Ikeda M, Nakashima T, Ohno S (2006) Elevation of serum Krebs von den Lunge-6 levels in patients with tubulointerstitial nephritis and uveitis syndrome. Am J Kidney Dis 48:935–941. https://doi.org/10.1053/j.ajkd.2006.09.013
Goda C, Kotake S, Ichiishi A, Namba K, Kitaichi N, Ohno S (2005) Clinical features in tubulointerstitial nephritis and uveitis (TINU) syndrome. Am J Ophthalmol 140:637–641. https://doi.org/10.1016/j.ajo.2005.04.019
Acknowledgements
We are grateful for the work of the past and present members of our laboratory.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were reviewed and approved by the Institutional Review Board of Hokkaido University Hospital and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Table 1
Baseline clinical and laboratory characteristics of the 29 enrolled children with TINU syndrome. Diagnostic criteria of D; Definite and P; probable. Gender F; Female, Gender M; Male. ESR; erythrocyte sedimentation rate (normal male range, 2-10 mm/h; normal female range 3-15 mm/h), Hb; blood hemoglobin, KL-6; sialylated carbohydrate antigen KL-6 (normal range < 500 U/mL), Pyuria (in urinary sediment 5 white blood cells (WBCs), > 400 times field of vision), PRO; proteinuria (> 1+ by dipstick method),GLU; glucosuria (> 1 ± by dipstick). N/A; not available. (PPTX 55.5 kb).
Rights and permissions
About this article
Cite this article
Hayashi, A., Takahashi, T., Ueda, Y. et al. Long-term clinical characteristics and renal prognosis of children with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 36, 2319–2325 (2021). https://doi.org/10.1007/s00467-021-04956-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-04956-6