Abstract
Background
There is increasing evidence that maternal obesity is associated with several structural birth defects. Congenital abnormalities of the kidney and urinary tract (CAKUT) account for 30 to 50% of children starting kidney replacement therapy (KRT). We conducted a systematic review, meta-analysis and ecological study to explore the relationship between maternal obesity and CAKUT.
Methods
A systematic literature search was conducted in EMBASE, MEDLINE, Global Health, The Cochrane Library, Scopus and Web of Science. Study quality was assessed for bias and confounding. A meta-analysis using a random effect model was carried out to obtain a summary odds ratio (OR) and 95% confidence interval (CI). In the ecological study, country-level data were used to examine the correlation of secular trends in female obesity, CAKUT incidence and incidence of KRT.
Results
Eight epidemiological studies were included in the review—4 cohort studies and 4 case-control studies—7 of which were included in the meta-analysis. There was evidence of a positive association between obesity during pregnancy and the risk of CAKUT, with a summary OR = 1.14 (1.02–1.27). No association was seen with overweight, nor a dose response with increasing obesity. There was an increasing trend in countries’ proportion of female obesity and an increasing trend in reported CAKUT incidence with specific rises seen in congenital hydronephrosis (CH) and multicystic kidney dysplasia (MCKD).
Conclusions
Our findings suggest that pre-pregnancy obesity may be associated with increased risk of CAKUT at population level.

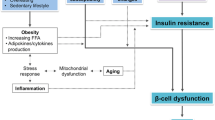
Graphical abstract




Similar content being viewed by others
References
WHO Obesity and Overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 26/02/2020 2020
Stothard KJ, Tennant PW, Bell R, Rankin J (2009) Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA 301:636–650. https://doi.org/10.1001/jama.2009.113
Huang HY, Chen HL, Feng LP (2017) Maternal obesity and the risk of neural tube defects in offspring: a meta-analysis. Obes Res Clin Pract 11:188–197. https://doi.org/10.1016/j.orcp.2016.04.005
Zhu Y, Chen Y, Feng Y, Yu D, Mo X (2018) Association between maternal body mass index and congenital heart defects in infants: a meta-analysis. Congenit Heart Dis 13:271–281. https://doi.org/10.1111/chd.12567
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373. https://doi.org/10.1007/s00467-011-1939-1
Andres-Jensen L, Jørgensen FS, Thorup J, Flachs J, Madsen JL, Maroun LL, Pernille Nørgaard P, Vinicoff PG, Olsen BH, Cortes D (2016) The outcome of antenatal ultrasound diagnosed anomalies of the kidney and urinary tract in a large Danish birth cohort. Arch Dis Child 101:819–824. https://doi.org/10.1136/archdischild-2015-309784
Tain Y-L, Luh H, Lin C-Y, Hsu C-N (2016) Incidence and risks of congenital anomalies of kidney and urinary tract in newborns: a population-based case-control study in Taiwan. Medicine 95:e2659–e2659. https://doi.org/10.1097/MD.0000000000002659
Nef S, Neuhaus TJ, Sparta G, Weitz M, Buder K, Wisser J, Gobet R, Willi U, Laube GF (2016) Outcome after prenatal diagnosis of congenital anomalies of the kidney and urinary tract. Eur J Pediatr 175:667–676. https://doi.org/10.1007/s00431-015-2687-1
Nicolaou N, Renkema KY, Bongers EM, Giles RH, Knoers NV (2015) Genetic, environmental, and epigenetic factors involved in CAKUT. Nat Rev Nephrol 11:720–731. https://doi.org/10.1038/nrneph.2015.140
Limwongse C (2009) Syndromes and malformations of the urinary tract. In: Editors: Avner EDHW HW, Niaudet P, Yoshikawa N (ed) Pediatric nephrology, 6th Edition, vol 1. Springer, Berlin, pp 122–138
Kanwar YS, Nayak B, Lin S, Akagi S, Xie P, Wada J, Chugh SS, Danesh FR (2005) Hyperglycemia: its imminent effects on mammalian nephrogenesis. Pediatr Nephrol 20:858–866. https://doi.org/10.1007/s00467-005-1888-7
Glastras SJ, Chen H, McGrath RT, Zaky AA, Gill AJ, Pollock CA, Saad S (2016) Effect of GLP-1 receptor activation on offspring kidney health in a rat model of maternal obesity. Sci Rep 6:23525–23525. https://doi.org/10.1038/srep23525
Zhao E, Zhang Y, Zeng X, Liu B (2015) Association between maternal diabetes mellitus and the risk of congenital malformations: a meta-analysis of cohort studies. Drug Discov Ther 9:274–281. https://doi.org/10.5582/ddt.2015.01044
Balsells M, Garcia-Patterson A, Gich I, Corcoy R (2009) Maternal and fetal outcome in women with type 2 versus type 1 diabetes mellitus: a systematic review and metaanalysis. J Clin Endocrinol Metab 94:4284–4291. https://doi.org/10.1210/jc.2009-1231
Parimi M, Nitsch D (2020) A systematic review and meta-analysis of diabetes during pregnancy and congenital genitourinary abnormalities. Kidney Int Rep 5:678–693. https://doi.org/10.1016/j.ekir.2020.02.1027
Slickers JE, Olshan AF, Siega-Riz AM, Honein MA, Aylsworth AS (2008) Maternal body mass index and lifestyle exposures and the risk of bilateral renal agenesis or hypoplasia: the National Birth Defects Prevention Study. Am J Epidemiol 168:1259–1267. https://doi.org/10.1093/aje/kwn248
Block SR, Watkins SM, Salemi JL, Rutkowski R, Tanner JP, Correia JA, Kirby RS (2013) Maternal pre-pregnancy body mass index and risk of selected birth defects: evidence of a dose-response relationship. Paediatr Perinat Epidemiol 27:521–531. https://doi.org/10.1111/ppe.12084
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Higgins JPT G, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Chapter 10. The Cochrane Collaboration; 2011. https://training.cochrane.org/handbook/current/chapter-10
EUROCAT European network of population-based registries for the epidemiological surveillance of congenital anomalies. European Commission. https://eu-rd-platform.jrc.ec.europa.eu/eurocat. 2019
Blomberg MI, Kallen B (2010) Maternal obesity and morbid obesity: the risk for birth defects in the offspring. Birth Defects Res A Clin Mol Teratol 88:35–40. https://doi.org/10.1002/bdra.20620
Garcia-Patterson A, Erdozain L, Ginovart G, Adelantado JM, Cubero JM, Gallo G, de Leiva A, Corcoy R (2004) In human gestational diabetes mellitus congenital malformations are related to pre-pregnancy body mass index and to severity of diabetes. Diabetologia 47:509–514. https://doi.org/10.1007/s00125-004-1337-3
Persson M, Cnattingius S, Villamor E, Soderling J, Pasternak B, Stephansson O, Neovius M (2017) Risk of major congenital malformations in relation to maternal overweight and obesity severity: cohort study of 1.2 million singletons. BMJ 357:j2563. https://doi.org/10.1136/bmj.j2563
Honein MA, Moore CA, Watkins ML (2003) Subfertility and prepregnancy overweight/obesity: possible interaction between these risk factors in the etiology of congenital renal anomalies. Birth Defects Res A Clin Mol Teratol 67:572–577. https://doi.org/10.1002/bdra.10077
Oddy WH, De Klerk NH, Miller M, Payne J, Bower C (2009) Association of maternal pre-pregnancy weight with birth defects: evidence from a case-control study in Western Australia. Aust N Z J Obstet Gynaecol 49:11–15. https://doi.org/10.1111/j.1479-828X.2008.00934.x
Tromp L, de Walle HEK (2012) Pre-pregnant maternal obesity increases risk of several congenital anomalies, in particular neural tune defects in the offspring. UMCG EUROCAT Northern Netherlands http://scripties.umcg.eldoc.ub.rug.nl/FILES/root/geneeskunde/2012/TrompL/TrompL.pdf
Organization WH Body Mass Index. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
(1998) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res 6 Suppl 2:51S–209S
WHO: World health statistics 2009. Geneva: World Health Organization 2009
WHO (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i-xii, 1–253
Catalano PM, Shankar K (2017) Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ 356:j1. https://doi.org/10.1136/bmj.j1
Tudur Smith C, Marcucci M, Nolan SJ, Iorio A, Sudell M, Riley R, Rovers MM, Williamson PR (2016) Individual participant data meta-analyses compared with meta-analyses based on aggregate data. Cochrane Database Syst Rev 9:Mr000007. https://doi.org/10.1002/14651858.MR000007.pub3
Tierney JF, Fisher DJ, Burdett S, Stewart LA, Parmar MKB (2020) Comparison of aggregate and individual participant data approaches to meta-analysis of randomised trials: an observational study. PLoS Med 17:e1003019. https://doi.org/10.1371/journal.pmed.1003019
Neild GH (2009) What do we know about chronic renal failure in young adults? I. primary renal disease. Pediatr Nephrol 24:1913–1919. https://doi.org/10.1007/s00467-008-1108-3
Gaillard R, Steegers EA, Duijts L, Felix JF, Hofman A, Franco OH, Jaddoe VWV (2014) Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the generation R study. Hypertension 63:683–691. https://doi.org/10.1161/hypertensionaha.113.02671
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, Bergström A, Charles MA, Chatzi L, Chevrier C, Chrousos GP, Corpeleijn E, Costet N, Crozier S, Devereux G, Eggesbø M, Ekström S, Fantini MP, Farchi S, Forastiere F, Georgiu V, Godfrey KM, Gori D, Grote V, Hanke W, Hertz-Picciotto I, Heude B, Hryhorczuk D, Huang RC, Inskip H, Iszatt N, Karvonen AM, Kenny LC, Koletzko B, Küpers LK, Lagström H, Lehmann I, Magnus P, Majewska R, Mäkelä J, Manios Y, McAuliffe FM, McDonald SW, Mehegan J, Mommers M, Morgen CS, Mori TA, Moschonis G, Murray D, Chaoimh CN, Nohr EA, Nybo Andersen AM, Oken E, Oostvogels AJJM, Pac A, Papadopoulou E, Pekkanen J, Pizzi C, Polanska K, Porta D, Richiardi L, Rifas-Shiman SL, Ronfani L, Santos AC, Standl M, Stoltenberg C, Thiering E, Thijs C, Torrent M, Tough SC, Trnovec T, Turner S, van Rossem L, von Berg A, Vrijheid M, Vrijkotte TGM, West J, Wijga A, Wright J, Zvinchuk O, Sørensen TIA, Lawlor DA, Gaillard R, Jaddoe VWV (2019) Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med 16:e1002744. https://doi.org/10.1371/journal.pmed.1002744
Acknowledgements
We are grateful to Dr. Poongkodi Nagappan, Consultant Urologist, Kuala Lumpur Hospital, Malaysia for having read and commented.
Availability of data
Data are already in the public domain. Not Applicable.
Funding
This study used aggregate data already in the public domain and did not required ethical approval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lyda Jadresić and Howard Au Joint first authors
Rights and permissions
About this article
Cite this article
Jadresić, L., Au, H., Woodhouse, C. et al. Pre-pregnancy obesity and risk of congenital abnormalities of the kidney and urinary tract (CAKUT)—systematic review, meta-analysis and ecological study. Pediatr Nephrol 36, 119–132 (2021). https://doi.org/10.1007/s00467-020-04679-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04679-0