Abstract
Background
Cardiovascular disease is the leading cause of death in children with chronic kidney disease (CKD). Serum levels of gut-derived uremic toxins increase with deterioration of kidney function and are associated with cardiac comorbidities in adult CKD patients.
Methods
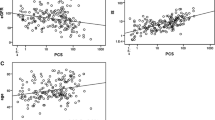
Indoxyl sulfate (IS) and p-cresyl sulfate (pCS) were measured by high-performance liquid chromatography in serum of children participating in the Cardiovascular Comorbidity in Children with CKD (4C) Study. Results were correlated with measurements of the carotid intima-media thickness (cIMT), central pulse wave velocity (PWV), and left ventricular mass index (LVMI) in children aged 6–17 years with initial eGFR of 10–60 ml/min per 1.73 m2.
Results
The median serum levels of total IS and of pCS, measured in 609 patients, were 5.3 μmol/l (8.7) and 17.0 μmol/l (21.6), respectively. In a multivariable regression model, IS and pCS showed significant positive associations with urea and negative associations with eGFR and uric acid. Furthermore, positive associations of pCS with age, serum albumin, and non-Mediterranean residency and a negative association with glomerular disease were observed. By multivariable regression analysis, only IS was significantly associated with a higher cIMT SDS at baseline and progression of PWV SDS within 12 months, independent of other risk factors.
Conclusions
Serum levels of gut-derived uremic toxins IS and pCS correlated inversely with eGFR in children. Only IS was significantly associated with surrogate markers of cardiovascular disease in this large pediatric CKD cohort.


Similar content being viewed by others
References
Barreto FC, Barreto DV, Liabeuf S, Meert N, Glorieux G, Temmar M, Choukroun G, Vanholder R, Massy ZA (2009) Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin J Am Soc Nephrol 4:1551–1558
Lin CJ, Wu V, Wu PC, Wu CJ (2015) Meta-analysis of the associations of p-cresyl sulfate (PCS) and indoxyl sulfate (IS) with cardiovascular events and all-cause mortality in patients with chronic renal failure. PLoS One 10:e0132589
Poesen R, Viaene L, Verbeke K, Claes K, Bammens B, Sprangers B, Naesens M, Vanrenterghem Y, Kuypers D, Evenepoel P, Meijers B (2013) Renal clearance and intestinal generation of p-cresyl sulfate and indoxyl sulfate in CKD. Clin J Am Soc Nephrol 8:1508–1514
van den Brand JA, Mutsaers HA, van Zuilen AD, Blankestijn PJ, van den Broek PH, Russel FG, Masereeuw R, Wetzels JF (2016) Uremic solutes in chronic kidney disease and their role in progression. PLoS One 11:e0168117
Grant CJ, Harrison LE, Hoad CL, Marciani L, Gowland PA, McIntyre CW (2016) Patients with CKD have abnormal upper gastro-intestinal tract digestive function: a study of uremic enteropathy. J Gastroenterol Hepatol
Ramezani A, Massy ZA, Meijers B, Evenepoel P, Vanholder R, Raj DS (2016) Role of the gut microbiome in uremia: a potential therapeutic target. Am J Kidney Dis 67:483–498
Vaziri ND, Zhao YY, Pahl MV (2016) Altered intestinal microbial flora and impaired epithelial barrier structure and function in CKD: the nature, mechanisms, consequences and potential treatment. Nephrol Dial Transplant 31:737–746
Andersen K, Kesper MS, Marschner JA, Konrad L, Ryu M, Kumar Vr S, Kulkarni OP, Mulay SR, Romoli S, Demleitner J, Schiller P, Dietrich A, Muller S, Gross O, Ruscheweyh HJ, Huson DH, Stecher B, Anders HJ (2016) Intestinal dysbiosis, barrier dysfunction, and bacterial translocation account for CKD-related systemic inflammation. J Am Soc Nephrol
Vaziri ND, Yuan J, Norris K (2013) Role of urea in intestinal barrier dysfunction and disruption of epithelial tight junction in chronic kidney disease. Am J Nephrol 37:1–6
Khouzam N, Wesseling-Perry K (2017) Pathophysiology and treatment of cardiovascular disease in pediatric chronic kidney disease. Pediatr Nephrol
Mitsnefes MM (2012) Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23:578–585
Kracht D, Shroff R, Baig S, Doyon A, Jacobi C, Zeller R, Querfeld U, Schaefer F, Wuhl E, Schmidt BM, Melk A (2011) Validating a new oscillometric device for aortic pulse wave velocity measurements in children and adolescents. Am J Hypertens 24:1294–1299
Doyon A, Kracht D, Bayazit AK, Deveci M, Duzova A, Krmar RT, Litwin M, Niemirska A, Oguz B, Schmidt BM, Sozeri B, Querfeld U, Melk A, Schaefer F, Wuhl E (2013) Carotid artery intima-media thickness and distensibility in children and adolescents: reference values and role of body dimensions. Hypertension 62:550–556
Schaefer F, Doyon A, Azukaitis K, Bayazit A, Canpolat N, Duzova A, Niemirska A, Sozeri B, Thurn D, Anarat A, Ranchin B, Litwin M, Caliskan S, Candan C, Baskin E, Yilmaz E, Mir S, Kirchner M, Sander A, Haffner D, Melk A, Wuhl E, Shroff R, Querfeld U, Consortium CS (2017) Cardiovascular phenotypes in children with CKD: the 4C study. Clin J Am Soc Nephrol 12:19–28
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Doyon A, Fischer DC, Bayazit AK, Canpolat N, Duzova A, Sozeri B, Bacchetta J, Balat A, Buscher A, Candan C, Cakar N, Donmez O, Dusek J, Heckel M, Klaus G, Mir S, Ozcelik G, Sever L, Shroff R, Vidal E, Wuhl E, Gondan M, Melk A, Querfeld U, Haffner D, Schaefer F, Consortium CS (2015) Markers of bone metabolism are affected by renal function and growth hormone therapy in children with chronic kidney disease. PLoS One 10:e0113482
Querfeld U, Anarat A, Bayazit AK, Bakkaloglu AS, Bilginer Y, Caliskan S, Civilibal M, Doyon A, Duzova A, Kracht D, Litwin M, Melk A, Mir S, Sozeri B, Shroff R, Zeller R, Wuhl E, Schaefer F (2010) The cardiovascular comorbidity in children with chronic kidney disease (4C) study: objectives, design, and methodology. Clin J Am Soc Nephrol 5:1642–1648
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, Ebrahim S, Fatar M, Hernandez Hernandez R, Kownator S, Prati P, Rundek T, Taylor A, Bornstein N, Csiba L, Vicaut E, Woo KS, Zannad F (2004) Mannheim intima-media thickness consensus. Cerebrovasc Dis 18:346–349
Chinali M, Emma F, Esposito C, Rinelli G, Franceschini A, Doyon A, Raimondi F, Pongiglione G, Schaefer F, Matteucci MC (2016) Left ventricular mass indexing in infants, children, and adolescents: a simplified approach for the identification of left ventricular hypertrophy in clinical practice. J Pediatr 170:193–198
Thurn D, Doyon A, Sozeri B, Bayazit AK, Canpolat N, Duzova A, Querfeld U, Schmidt BM, Schaefer F, Wuhl E, Melk A (2015) Aortic pulse wave velocity in healthy children and adolescents: reference values for the Vicorder device and modifying factors. Am J Hypertens 28:1480–1488
Group KW (2009) KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. Executive summary. Am J Kidney Dis 53:S11–S104
Duranton F, Cohen G, De Smet R, Rodriguez M, Jankowski J, Vanholder R, Argiles A (2012) Normal and pathologic concentrations of uremic toxins. J Am Soc Nephrol 23:1258–1270
Rossi M, Campbell K, Johnson D, Stanton T, Pascoe E, Hawley C, Dimeski G, McWhinney B, Ungerer J, Isbel N (2014) Uraemic toxins and cardiovascular disease across the chronic kidney disease spectrum: an observational study. Nutr Metab Cardiovasc Dis 24:1035–1042
Vanholder R, Schepers E, Pletinck A, Nagler EV, Glorieux G (2014) The uremic toxicity of indoxyl sulfate and p-cresyl sulfate: a systematic review. J Am Soc Nephrol 25:1897–1907
Lau WL, Savoj J, Nakata MB, Vaziri ND (2018) Altered microbiome in chronic kidney disease: systemic effects of gut-derived uremic toxins. Clin Sci (Lond) 132:509–522
Ryu JH, Park H, Kim SJ (2017) The effects of indoxyl sulfate-induced endothelial microparticles on neointimal hyperplasia formation in an ex vivo model. Ann Surg Treat Res 93:11–17
Carmona A, Aguera ML, Luna-Ruiz C, Buendia P, Calleros L, Garcia-Jerez A, Rodriguez-Puyol M, Arias M, Arias-Guillen M, de Arriba G, Ballarin J, Bernis C, Fernandez E, Garcia-Rebollo S, Mancha J, Del Peso G, Perez E, Poch E, Portoles JM, Rodriguez-Puyol D, Sanchez-Villanueva R, Sarro F, Torres A, Martin-Malo A, Aljama P, Ramirez R, Carracedo J (2017) Markers of endothelial damage in patients with chronic kidney disease on hemodialysis. Am J Physiol Renal Physiol 312:F673–f681
Pletinck A, Glorieux G, Schepers E, Cohen G, Gondouin B, Van Landschoot M, Eloot S, Rops A, Van de Voorde J, De Vriese A, van der Vlag J, Brunet P, Van Biesen W, Vanholder R (2013) Protein-bound uremic toxins stimulate crosstalk between leukocytes and vessel wall. J Am Soc Nephrol 24:1981–1994
Wakamatsu T, Yamamoto S, Ito T, Sato Y, Matsuo K, Takahashi Y, Kaneko Y, Goto S, Kazama JJ, Gejyo F, Narita I (2018) Indoxyl sulfate promotes macrophage IL-1beta production by activating aryl hydrocarbon receptor/NF-kappa/MAPK cascades, but the NLRP3 inflammasome was not activated. Toxins (Basel) 10
Dou L, Poitevin S, Sallee M, Addi T, Gondouin B, McKay N, Denison MS, Jourde-Chiche N, Duval-Sabatier A, Cerini C, Brunet P, Dignat-George F, Burtey S (2018) Aryl hydrocarbon receptor is activated in patients and mice with chronic kidney disease. Kidney Int 93:986–999
Drueke TB, Massy ZA (2016) Changing bone patterns with progression of chronic kidney disease. Kidney Int 89:289–302
Yamamoto S, Fukagawa M (2017) Uremic toxicity and bone in CKD. J Nephrol 30:623–627
Shafi T, Meyer TW, Hostetter TH, Melamed ML, Parekh RS, Hwang S, Banerjee T, Coresh J, Powe NR (2015) Free levels of selected organic solutes and cardiovascular morbidity and mortality in hemodialysis patients: results from the retained organic solutes and clinical outcomes (ROSCO) investigators. PLoS One 10:e0126048
Shafi T, Sirich TL, Meyer TW, Hostetter TH, Plummer NS, Hwang S, Melamed ML, Banerjee T, Coresh J, Powe NR (2017) Results of the HEMO study suggest that p-cresol sulfate and indoxyl sulfate are not associated with cardiovascular outcomes. Kidney Int 92:1484–1492
Kortman GAM, Reijnders D, Swinkels DW (2017) Oral iron supplementation: potential implications for the gut microbiome and metabolome in patients with CKD. Hemodial Int 21(Suppl 1):S28–S36
Drueke T, Witko-Sarsat V, Massy Z, Descamps-Latscha B, Guerin AP, Marchais SJ, Gausson V, London GM (2002) Iron therapy, advanced oxidation protein products, and carotid artery intima-media thickness in end-stage renal disease. Circulation 106:2212–2217
Kshirsagar AV, Freburger JK, Ellis AR, Wang L, Winkelmayer WC, Brookhart MA (2013) Intravenous iron supplementation practices and short-term risk of cardiovascular events in hemodialysis patients. PLoS One 8:e78930
Snauwaert E, Van Biesen W, Raes A, Glorieux G, Van Bogaert V, Van Hoeck K, Coppens M, Roels S, Vande Walle J, Eloot S (2017) Concentrations of representative uraemic toxins in a healthy versus non-dialysis chronic kidney disease paediatric population. Nephrol Dial Transplant
Hyun HS, Paik KH, Cho HY (2013) p-Cresyl sulfate and indoxyl sulfate in pediatric patients on chronic dialysis. Kor J Pediatr 56:159–164
Wyczalkowska-Tomasik A, Czarkowska-Paczek B, Giebultowicz J, Wroczynski P, Paczek L (2017) Age-dependent increase in serum levels of indoxyl sulphate and p-cresol sulphate is not related to their precursors: tryptophan and tyrosine. Geriatr Gerontol Int 17:1022–1026
Viaene L, Thijs L, Jin Y, Liu Y, Gu Y, Meijers B, Claes K, Staessen J, Evenepoel P (2014) Heritability and clinical determinants of serum indoxyl sulfate and p-cresyl sulfate, candidate biomarkers of the human microbiome enterotype. PLoS One 9:e79682
Deguchi T, Kusuhara H, Takadate A, Endou H, Otagiri M, Sugiyama Y (2004) Characterization of uremic toxin transport by organic anion transporters in the kidney. Kidney Int 65:162–174
Meijers BK, De Loor H, Bammens B, Verbeke K, Vanrenterghem Y, Evenepoel P (2009) p-Cresyl sulfate and indoxyl sulfate in hemodialysis patients. Clin J Am Soc Nephrol 4:1932–1938
Rossi M, Johnson DW, Xu H, Carrero JJ, Pascoe E, French C, Campbell KL (2015) Dietary protein-fiber ratio associates with circulating levels of indoxyl sulfate and p-cresyl sulfate in chronic kidney disease patients. Nutr Metab Cardiovasc Dis 25:860–865
Poesen R, Mutsaers HA, Windey K, van den Broek PH, Verweij V, Augustijns P, Kuypers D, Jansen J, Evenepoel P, Verbeke K, Meijers B, Masereeuw R (2015) The influence of dietary protein intake on mammalian tryptophan and phenolic metabolites. PLoS One 10:e0140820
Black AP, Anjos JS, Cardozo L, Carmo FL, Dolenga CJ, Nakao LS, de Carvalho FD, Rosado A, Carraro Eduardo JC, Mafra D (2018) Does low-protein diet influence the uremic toxin serum levels from the gut microbiota in nondialysis chronic kidney disease patients? J Ren Nutr
Nigam SK, Bush KT, Martovetsky G, Ahn SY, Liu HC, Richard E, Bhatnagar V, Wu W (2015) The organic anion transporter (OAT) family: a systems biology perspective. Physiol Rev 95:83–123
Bush KT, Wu W, Lun C, Nigam SK (2017) The drug transporter OAT3 (SLC22A8) and endogenous metabolite communication via the gut-liver-kidney axis. J Biol Chem 292:15789–15803
Nigam SK, Wu W, Bush KT, Hoenig MP, Blantz RC, Bhatnagar V (2015) Handling of drugs, metabolites, and uremic toxins by kidney proximal tubule drug transporters. Clin J Am Soc Nephrol 10:2039–2049
Borghi C, Rosei EA, Bardin T, Dawson J, Dominiczak A, Kielstein JT, Manolis AJ, Perez-Ruiz F, Mancia G (2015) Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens 33:1729–1741 discussion 1741
Gryp T, Vanholder R, Vaneechoutte M, Glorieux G (2017) p-Cresyl sulfate. Toxins (Basel) 9
Eloot S, Van Biesen W, Roels S, Delrue W, Schepers E, Dhondt A, Vanholder R, Glorieux G (2017) Spontaneous variability of pre-dialysis concentrations of uremic toxins over time in stable hemodialysis patients. PLoS One 12:e0186010
Sekula P, Goek ON, Quaye L, Barrios C, Levey AS, Romisch-Margl W, Menni C, Yet I, Gieger C, Inker LA, Adamski J, Gronwald W, Illig T, Dettmer K, Krumsiek J, Oefner PJ, Valdes AM, Meisinger C, Coresh J, Spector TD, Mohney RP, Suhre K, Kastenmuller G, Kottgen A (2016) A metabolome-wide association study of kidney function and disease in the general population. J Am Soc Nephrol 27:1175–1188
Goek ON, Prehn C, Sekula P, Romisch-Margl W, Doring A, Gieger C, Heier M, Koenig W, Wang-Sattler R, Illig T, Suhre K, Adamski J, Kottgen A, Meisinger C (2013) Metabolites associate with kidney function decline and incident chronic kidney disease in the general population. Nephrol Dial Transplant 28:2131–2138
Rhee EP, Clish CB, Ghorbani A, Larson MG, Elmariah S, McCabe E, Yang Q, Cheng S, Pierce K, Deik A, Souza AL, Farrell L, Domos C, Yeh RW, Palacios I, Rosenfield K, Vasan RS, Florez JC, Wang TJ, Fox CS, Gerszten RE (2013) A combined epidemiologic and metabolomic approach improves CKD prediction. J Am Soc Nephrol 24:1330–1338
Rhee EP, Clish CB, Wenger J, Roy J, Elmariah S, Pierce KA, Bullock K, Anderson AH, Gerszten RE, Feldman HI (2016) Metabolomics of chronic kidney disease progression: a case-control analysis in the chronic renal insufficiency cohort study. Am J Nephrol 43:366–374
Atherton JG, Hains DS, Bissler JJ, Pendley BD, Lindner E (2018) Generation, clearance, toxicity and monitoring possibilities of unaccounted uremic toxins for improved dialysis prescriptions. Am J Physiol Renal Physiol
Deltombe O, Van Biesen W, Glorieux G, Massy Z, Dhondt A, Eloot S (2015) Exploring protein binding of uremic toxins in patients with different stages of chronic kidney disease and during hemodialysis. Toxins (Basel) 7:3933–3946
Borges NA, Carmo FL, Stockler-Pinto MB, de Brito JS, Dolenga CJ, Ferreira DC, Nakao LS, Rosado A, Fouque D, Mafra D (2017) Probiotic supplementation in chronic kidney disease: a double-blind, randomized, placebo-controlled trial. J Ren Nutr
Funding
This study was made possible by grants from the European Renal Association-European Dialysis and Transplant Association (www.era-edta.org), the Kuratorium für Dialyse und Nierentransplantation (KfH) Foundation for Preventive Medicine, the German Federal Ministry of Education and Research (reference no. 01EO0802), and Pfizer Deutschland GmbH. The entire study was solely initiated and performed by the investigators of the 4C study group. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was partly funded by Pfizer Deutschland GmbH. There are no patents, products in development, or marketed products to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
(DOCX 161 kb)
Online Resource 2
(DOCX 24 kb)
Online Resource 3
(DOCX 24 kb)
Online Resource 4
(DOCX 121 kb)
Online Resource 5
(DOCX 25 kb)
Online Resource 6
(DOCX 23 kb)
Online Resource 7
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Holle, J., Querfeld, U., Kirchner, M. et al. Indoxyl sulfate associates with cardiovascular phenotype in children with chronic kidney disease. Pediatr Nephrol 34, 2571–2582 (2019). https://doi.org/10.1007/s00467-019-04331-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04331-6