Abstract
Background
This study was performed to determine the clinical features and outcomes of childhood-onset anti-neutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV), particularly microscopic polyangiitis (MPA).
Methods
A retrospective Japanese multicenter study was performed in patients diagnosed with AAV before 16 years of age.
Results
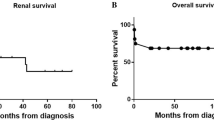
Of 49 patients with AAV, 36 were female. The diagnoses were as follows: MPA (n = 38, 78%), granulomatosis with polyangiitis (GPA; n = 9, 18%), eosinophilic granulomatosis with polyangiitis (EGPA; n = 1, 2%), and other (n = 1, 2%). The median age at onset was 10.7 years, and median time to diagnosis was 2.0 months. Twenty-seven (55%) patients were identified through a school urinary screening program. Initial symptoms included fever and fatigue (45%), and renal (71%), pulmonary (29%), ocular (20%), and mucocutaneous involvement (22%). Although 27 (55%) patients achieved remission and none had died at the last follow-up, at least one recurrence occurred in 13 (48%) patients after a median of 48 months and was more common in patients with GPA (P < 0.01). After a median follow-up of 43 months, seven (14%) patients (all with MPA) progressed to end-stage renal disease (ESRD).
Conclusions
Childhood-onset AAV has an estimated prevalence of 3.41–4.28 per million children and is characterized by female predominance and high frequency of detection in school urinary screening programs. More than 10% of patients with childhood-onset AAV still progress to ESRD without achieving remission. Histological chronicity is a factor associated with ESRD.



Similar content being viewed by others
References
Morishita KA, Moorthy LN, Lubieniecka JM, Twilt M, Yeung RS, Toth MB, Shenoi S, Ristic G, Nielsen SM, Luqmani RA, Li SC (2017) Early outcomes in children with antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheumatol 69:1470–1479
Sacri AS, Chambaraud T, Ranchin B, Florkin B, Sée H, Decramer S, Flodrops H, Ulinski T, Allain-Launay E, Boyer O, Dunand O (2015) Clinical characteristics and outcomes of childhood-onset ANCA-associated vasculitis: a French nationwide study. Nephrol Dial Transplant 30:i104–i112
Iudici M, Puéchal X, Pagnoux C, Quartier P, Agard C, Aouba A, Büchler M, Cevallos R, Cohen P, de Moreuil C, Guilpain P (2015) Brief report: childhood-onset systemic necrotizing vasculitides: long-term data from the french vasculitis study group registry. Arthritis Rheumatol 67:1959–1965
Cabral DA, Canter DL, Muscal E, Nanda K, Wahezi DM, Spalding SJ, Twilt M, Benseler SM, Campillo S, Charuvanij S, Dancey P, Eberhard BA, Elder ME, Hersh A, Higgins GC, Huber AM, Khubchandani R, Kim S, Klein-Gitelman M, Kostik MM, Lawson EF, Lee T, Lubieniecka JM, McCurdy D, Moorthy LN, Morishita KA, Nielsen SM, O'Neil KM, Reiff A, Ristic G, Robinson AB, Sarmiento A, Shenoi S, Toth MB, Van Mater HA, Wagner-Weiner L, Weiss JE, White AJ, Yeung RS, ARChiVe Investigators Network within the PedVas Initiative (2016) Comparing presenting clinical features in 48 children with microscopic polyangiitis to 183 children who have granulomatosis with polyangiitis (Wegener’s): an ARChiVe cohort study. Arthritis Rheumatol 68:2514–2526
Rottem M, Fauci AS, Hallahan CW, Kerr GS, Lebovics R, Leavitt RY, Hoffman GS (1993) Wegener granulomatosis in children and adolescents: clinical presentation and outcome. J Pediatr 122:26–31
Ellis EN, Wood EG, Berry P (1995) Spectrum of disease associated with anti-neutrophil cytoplasmic autoantibodies in pediatric patients. J Pediatr 126:40–43
Stegmayr BG, Gothefors L, Malmer B, Müller DE, Nilsson K, Sundelin B (2000) Wegener granulomatosis in children and young adults. A case study of ten patients. Pediatr Nephrol 14:208–213
Deshpande PV, Gilbert R, Alton H, Milford DV (2000) Microscopic polyarteritis with renal and cerebral involvement. Pediatr Nephrol 15:134–135
Belostotsky VM, Shah V, Dillon MJ (2002) Clinical features in 17 paediatric patients with Wegener granulomatosis. Pediatr Nephrol 17:754–761
Yu F, Huang JP, Zou WZ, Zhao MH (2006) The clinical features of anti-neutrophil cytoplasmic antibody-associated systemic vasculitis in Chinese children. Pediatr Nephrol 21:497–502
Peco-Antic A, Bonaci-Nikolic B, Basta-Jovanovic G, Kostic M, Markovic-Lipkovski J, Nikolic M, Spasojevic B (2006) Childhood microscopic polyangiitis associated with MPO-ANCA. Pediatr Nephrol 21:46–53
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS (2013) 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
Ozen S, Ruperto N, Dillon MJ, Bagga A, Barron K, Davin JC, Kawasaki T, Lindsley C, Petty RE, Prieur AM, Ravelli A (2006) EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Ann Rheum Dis 65:936–941
Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, Buoncompagni A, Lazar C, Bilge I, Uziel Y, Rigante D (2010) EULAR/PRINTO/PRES criteria for Henoch- Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: final classification criteria. Ann Rheum Dis 69:798–806
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, Jones R (2009) Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis 68:1827–1832
Dolezalova P, Price-Kuehne FE, Özen S, Benseler SM, Cabral DA, Anton J, Brunner J, Cimaz R, O'Neil KM, Wallace CA, Wilkinson N, Eleftheriou D, Demirkaya E, Böhm M, Krol P, Luqmani RA, Brogan PA (2013) Disease activity assessment in childhood vasculitis: development and preliminary validation of the Paediatric Vasculitis Activity Score (PVAS). Ann Rheum Dis 72:1628–1633
Hashimoto S, Fukutomi K, Nagai M, Nakamura Y, Yanagawa H, Sasaki R, Ohno Y (1990) A note on methods for estimating the number of patients in the nationwide epidemiological survey on intractable diseases. Nihon Koshu Eisei Zasshi 37:768–774 (in Japanese)
Little RJ, Vartivarian S (2003) On weighting the rates in non-response weights. Stat Med 22:1589–1599
The Statistics Bureau of the Ministry of Internal Affairs and Communications of Japan http://www.stat.go.jp/english/index.html. Accessed 12 May 2018
Savage CO, Winearls CG, Evans DJ, Rees AJ, Lockwood CM (1985) Microscopic polyarteritis: presentation, pathology and prognosis. Q J Med 56:467–483
Siomou E, Tramma D, Bowen C, Milford DV (2012) ANCA-associated glomerulonephritis/systemic vasculitis in childhood: clinical features-outcome. Pediatr Nephrol 27:1911–1920
Hattori M, Kurayama H, Koitabashi Y (2001) Antineutrophil cytoplasmic autoantibody- associated glomerulonephritis in children. J Am Soc Nephrol 12:1493–1500
Sun L, Wang H, Jiang X, Mo Y, Yue Z, Huang L, Liu T (2014) Clinical and pathological features of microscopic polyangiitis in 20 children. J Rheumatol 41:1712–1719
Yamato K, Ishii T, Kawamura T (2012) Microscopic polyangiitis in a girl with severe anemia and no respiratory symptoms. Pediatr Int 54:541–543
Chen M, Yu F, Zhang Y, Zhao MH (2005) Clinical [corrected] and pathological characteristics of Chinese patients with antineutrophil cytoplasmic autoantibody associated systemic vasculitides: a study of 426 patients from a single centre. Postgrad Med J 81:723–727
Vanoni F, Bettinelli A, Keller F, Bianchetti MG, Simonetti GD (2010) Vasculitides associated with IgG antineutrophil cytoplasmic autoantibodies in childhood. Pediatr Nephrol 25:205–212
Geetha D, Specks U, Stone JH, Merkel PA, Seo P, Spiera R, Langford CA, Hoffman GS, Kallenberg CG, Clair EW, Fessler BJ (2015) Rituximab versus cyclophosphamide for ANCA-associated vasculitis with renal involvement. J Am Soc Nephrol 26:976–985
Basu B, Mahapatra TK, Mondal N (2015) Favourable renal survival in paediatric microscopic polyangiitis: efficacy of a novel treatment algorithm. Nephrol Dial Transplant 30:i113–i118
Sinico RA, Di Toma L, Radice A (2013) Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. Autoimmun Rev 4:477–482
Noone DG, Twilt M, Hayes WN, Thorner PS, Benseler S, Laxer RM, Parekh RS, Hebert D (2014) The new histopathologic classification of ANCA-associated GN and its association with renal outcomes in childhood. Clin J Am Soc Nephrol 7:1684–1691
Lee T, Gasim A, Derebail VK, Chung Y, McGregor JG, Lionaki S, Poulton CJ, Hogan SL, Jennette JC, Falk RJ, Nachman PH (2014) Predictors of treatment outcomes in ANCA-associated vasculitis with severe kidney failure. Clin J Am Soc Nephrol 7:905–913
Chen Y, Bao H, Liu Z, Liu X, Gao E, Zeng C, Zhang H, Liu Z, Hu W (2017) Risk factors for renal survival in Chinese patients with myeloperoxidase-ANCA-associated GN. Clin J Am Soc Nephrol 12:417–425
Vega LE, Espinoza LR (2016) Predictors of poor outcome in ANCA-associated vasculitis (AAV). Curr Rheumatol Rep 18:70
Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, Neumann I, Noël LH, Pusey CD, Waldherr R, Bruijn JA (2010) Histopathologic classification of ANCA- associated glomerulonephritis. J Am Soc Nephrol 21:1628–1636
Hilhorst M, Wilde B, van Breda Vriesman P, van Paassen P, Tervaert JW (2013) Estimating renal survival using the ANCA-associated GN classification. J Am Soc Nephrol 24:1371–1375
Chang DY, Wu LH, Liu G, Chen M, Kallenberg CG, Zhao MH (2012) Re-evaluation of the histopathologic classification of ANCA-associated glomerulonephritis: a study of 121 patients in a single center. Nephrol Dial Transplant 27:2343–2349
Tanna A, Guarino L, Tam FW, Rodriquez-Cubillo B, Levy JB, Cairns TD, Griffith M, Tarzi RM, Caplin B, Salama AD, Cook T (2015) Long-term outcome of anti-neutrophil cytoplasm antibody-associated glomerulonephritis: evaluation of the international histological classification and other prognostic factors. Nephrol Dial Transplant 30:1185–1192
Ford SL, Polkinghorne KR, Longano A, Dowling J, Dayan S, Kerr PG, Holdsworth SR, Kitching AR, Summers SA (2014) Histopathologic and clinical predictors of kidney outcomes in ANCA-associated vasculitis. Am J Kidney Dis 63:227–235
Iwakiri T, Fujimoto S, Kitagawa K, Furuichi K, Yamahana J, Matsuura Y, Yamashita A, Uezono S, Shimao Y, Hisanaga S, Tokura T (2013) Validation of a newly proposed histopathological classification in Japanese patients with anti-neutrophil cytoplasmic antibody-associated glomerulonephritis. BMC Nephrol 17:125
Togashi M, Komatsuda A, Nara M, Omokawa A, Okuyama S, Sawada K, Wakui H (2014) Validation of the 2010 histopathological classification of ANCA-associated glomerulonephritis in a Japanese single-center cohort. Mod Rheumatol 24:300–303
Muso E, Endo T, Itabashi M, Kakita H, Iwasaki Y, Tateishi Y, Komiya T, Ihara T, Yumura W, Sugiyama T, Joh K, Suzuki K (2013) Evaluation of the newly proposed simplified histological classification in Japanese cohorts of myeloperoxidase-anti- neutrophil cytoplasmic antibody-associated glomerulonephritis in comparison with other Asian and European cohorts. Clin Exp Nephrol 17:659–662
Ormerod AS, Cook MC (2008) Epidemiology of primary systemic vasculitis in the Australian Capital Territory and South-Eastern New South Wales. Intern Med J 38:816–823
Reinhold-Keller E, Zeidler A, Gutfleisch J, Peter HH, Raspe HH, Gross WL (2000) Giant cell arteritis is more prevalent in urban than in rural populations: results of an epidemiological study of primary systemic vasculitides in Germany. Rheumatology 39:1396–1402
Acknowledgments
The authors would like to thank all the institutions that participated in the surveys and Takayuki Okamoto (Hokkaido University Graduate School of Medicine), Kazushi Tsuruga (Hirosaki University), Naonori Kumagai (Tohoku University School of Medicine), Shigeo Suzuki (Ohara General Hospital), Kazuhide Suyama (Fukushima Medical University Hospital), Yasuo Oyake (Hitachi General Hospital), Yoko Ohwada (Dokkyo Medical University), Isamu Kamimaki (National Hospital Organization Saitama National Hospital), Koji Sakuraya (Saitama Children’s Medical Center), Yoshihiro Aoki (Asahi Hospital), Shosuke Sunami (Japanese Red Cross Narita Hospital), Shinsuke Matsumoto (Matsudo City General Hospital), Takashi Sato (Funabashi Futawa Hospital), Mamiko Suehiro (Chiba Children’s Hospital), Yuji Tomii (Tokyo Women’s Medical University Hospital), Tae Omori (Tokyo Metropolitan Bokutoh Hospital), Shojiro Okamoto (Tokai University Hachioji Hospital), Riku Hamada (Tokyo Metropolitan Children’s Medical Center), Takeshi Yanagihara (Nippon Medical School Musashi Kosugi Hospital), Hisashi Kaneda (Toyama City Hospital), Shoko Iwata (Ogaki Municipal Hospital), Masayoshi Yamada (Shizuoka Children’s Hospital), Naoya Fujita (Aichi Children’s Health and Medical Center), Nami Okamoto (Osaka Medical College Hospital), Kosuke Shabana (Osaka Medical College Hospital), Rika Fujimaru (Osaka City General Hospital), Takahisa Kimata (Kansai Medical University Hospital), Takeshi Ninchoji (Kobe University Graduate School of Medicine), Shingo Ishimori (Kakogawa City Hospital), Toshiyuki Ohta (Hiroshima Prefectural Hospital), Masafumi Teramachi (Fukuoka University Hospital), Kei Nishiyama (Kyushu University Hospital), Toshihiko Shirakawa (Nagasaki University Hospital), Hitoshi Nakazato (Kumamoto University Hospital), Akio Furuse (Japanese Red Cross Kumamoto Hospital), Hideaki Imamura (Faculty of Medicine, University of Miyazaki Hospital), and Tomoo Kise (Nanbu Medical Center/Nanbu Child Medical Center) for their contributions to the study. The authors would also like to thank Mr. Masanori Nimura of Yamate Information Processing Center Ltd. (Tokyo, Japan) for his participation in data management.
Funding
This work was supported by a Health and Labour Sciences Research Grant for Research in Rare and Intractable Diseases from the Ministry of Health, Labour, and Welfare, Japan (H26-nanchitou(nan)-ippan-036).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and with the ethical guidelines for epidemiological studies issued by the Ministry of Health, Labour and Welfare, Japan. The study was approved by the Ethics Review Committee of Graduate School of Medicine, Yokohama City University (institution of the principal investigator, SI, ID: B151201009) before commencement. Informed consent was not deemed necessary because the data were obtained retrospectively from the patient charts.
Conflict of interest
S.I. has received consulting fees from Novartis Pharma and Loche. S.I. has also received research grants from Asahi Kasei Pharma, Astellas Pharma, and Chugai Pharmaceutical. T.S. has received consulting fees from Takeda Pharmaceutical Company Limited. T.S. has also received lecture fees from Takeda Pharmaceutical Company Limited and Statcom Company Limited.
Additional information
The results presented in this paper have not been published previously in whole or part, except in abstract form.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirano, D., Ishikawa, T., Inaba, A. et al. Epidemiology and clinical features of childhood-onset anti-neutrophil cytoplasmic antibody–associated vasculitis: a clinicopathological analysis. Pediatr Nephrol 34, 1425–1433 (2019). https://doi.org/10.1007/s00467-019-04228-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04228-4