Abstract
Background
Routine surgical video recording has multiple benefits. Video acts as an objective record of the operative record, allows video-based coaching and is integral to the development of digital technologies. Despite these benefits, adoption is not widespread. To date, only questionnaire studies have explored this failure in adoption. This study aims to determine the barriers and provide recommendations for the implementation of routine surgical video recording.
Materials and methods
A pre- and post-pilot questionnaire surrounding a real-world implementation of a C-SATS©, an educational recording and surgical analytics platform, was conducted in a university teaching hospital trust. Usage metrics from the pilot study and descriptive analyses of questionnaire responses were used with the non-adoption, abandonment, scale-up, spread, sustainability (NASSS) framework to create topic guides for semi-structured interviews. Transcripts of interviews were evaluated in an inductive thematic analysis.
Results
Engagement with the C-SATS© platform failed to reach consistent levels with only 57 videos uploaded. Three attending surgeons, four surgical residents, one scrub nurse, three patients, one lawyer, and one industry representative were interviewed, all of which perceived value in recording. Barriers of ‘change,’ ‘resource,’ and ‘governance,’ were identified as the main themes. Resistance was centred on patient misinterpretation of videos. Participants believed availability of infrastructure would facilitate adoption but integration into surgical workflow is required. Regulatory uncertainty was centred around anonymity and data ownership.
Conclusion
Barriers to the adoption of routine surgical video recording exist beyond technological barriers alone. Priorities for implementation include integration recording into the patient record, engaging all stakeholders to ensure buy-in, and formalising consent processes to establish patient trust.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Minimally invasive techniques are standard practice for many surgical procedures performed worldwide [1]. However, despite this widespread use, only a minority of surgeons routinely record video for use beyond the perioperative period. A recent nationwide study demonstrated significant variations in the practices of surgical video recording in the UK, estimating that just one fifth of surgeons routinely record their procedures [2]. This is surprising as the benefits of routine video recording are multiple. Surgical video acts as an objective documentation of the operative record [3,4,5], is an invaluable resource for training [6, 7], and is a substantial data resource forming the foundation for many digital surgical applications [8]. Lack of data has been consistently cited as a significant barrier to progression of digital surgery [8,9,10] and the scale of surgical video datasets [9] are minute when compared to those within conventional computer vision research [11].
The failure to routinely record surgical video has often been attributed to a lack of available infrastructure [12]. However, a range of recording and surgical analytics products are now available on the market, including C-SATS© (Johnson and Johnson) and TouchSurgery™ (Medtronic), suggesting that the reason for non-adoption extends beyond technological barriers alone. Some of these hypothesized wider barriers include challenges to privacy both for patients and surgeons [13, 14], concerns that recordings may result in an increase in medicolegal action against surgeons [5, 15], and fears that routine video recording may lead to a Hawthorne effect [16, 17].
To date, the current literature exploring these barriers have comprised of questionnaire studies which are restricted in their exploratory scope. This mixed-methods study aims to build on the existing literature by completing an in-depth qualitative assessment of the barriers to routine surgical video recording. We utilize usage data from a real-world surgical video recording platform pilot study and include participants to contextualize barriers in a real-world clinical setting. From these results, recommendations for wider implementation of routine surgical video recording are derived to facilitate other researchers and institutions.
Methods
This study consisted of two phases (Fig. 1). Phase 1 consisted of the deployment of C-SATS© in a UK university teaching hospital trust. Phase 2 consisted of semi-structured interviews to explore perceptions, perceived utility, and barriers to implementation for routine surgical video recording.
Phase 1: Deployment of a surgical video recording platform
C-SATS© pilot
Phase 1 of this study incorporated a 44-week pilot of C-SATS©, a recording and surgical analytics platform at a UK university teaching hospital trust. The platform included a video library of expert cases as well as the function to record, review and receive feedback on individual procedures. All surgical residents and attendings across all specialties were invited to participate. The C-SATS© device was installed into ten operating rooms across three hospitals for 31 weeks capturing the stream from the endoscopic camera once the device had been manually activated, and user details inputted. Users had access to a video library of expert cases and an AI-powered analytics dashboard for longitudinal performance tracking. Engagement with the platform was monitored throughout and interventions, such as email reminders, were utilized if engagement dropped at any point.
Analysis
Pre- and post-pilot questionnaires were distributed to participants (Appendix 1–3). Questions focussed on satisfaction with current feedback from training procedures, opinion of video-based review, and AI methodologies for training. Questionnaire responses were used to extract themes to design topic guides for semi-structured interviews. Metrics regarding engagement and video uploads to the C-SATS© platform were also analyzed.
Phase 2: Semi-structured interviews
Topic guides
Topic guides were created by two authors (KL and CS), with separate guides for professional and patient participants. Themes identified from the questionnaire and the current literature were used to inform the questions. Topic guides were structured around the NASSS framework, which is defined as ‘an overarching theory of complex adaptive systems’ [18] (Appendix 4–6). The framework considers multiple domains within a system, and further stratifies by the assumed difficulty when implementing in this area. Thus, it allows for the thorough identification and weighting of barriers highlighted. This framework was chosen due to the identification of the complexity in introducing routine recording in the literature.
Study participants
Members of the extended surgical team were recruited using snowball sampling. All surgeons participating in the C-SATS© pilot were invited to participate, but pilot involvement was not a requirement. Industry, information governance, legal representatives, and patients were also invited to participate as key stakeholders. Patient participants were eligible if on a waiting list for surgery or had previously undergone surgery in the last 3 years.
Data collection
A grounded theory approach using a constructivist research paradigm was chosen to allow ideas to emerge from the data. Interview findings were reported using the Standards for Reporting Qualitative Research (SRQR) (Appendix 7). All interviews were conducted over Microsoft Teams (Microsoft, Redmond, WA, USA) or telephone call (CS). All interviews were recorded with informed consent. Transcripts were manually checked and anonymized for analysis.
Data analysis
An inductive thematic analysis was conducted (CS). Transcripts were studied intently to identify recurrent themes and ideas. Data were then coded with related codes being grouped into themes and sub-themes. Repeated reflection of the codes and themes continued until all themes were clearly defined. Refinement of the definitions was completed through discussion with a second researcher (KL). The codebook can be found in Table 1.
Ethical approval
A full ethical review was undertaken, and ethical approval was obtained through the NHS Research Ethics Service (Ref—22/SC/0259). Informed consent was obtained from all participants prior to interviews.
Results
Pre- and post-pilot questionnaire
The pre-pilot questionnaire was distributed to 46 residents and 26 attendings with response rates of 21.7 and 26.9%, respectively. The total number of users was reduced to 30 during the pilot. The post-pilot questionnaire was distributed to 19 residents and 11 attendings, with response rates of 42.1 and 27.2%, respectively. All respondents in the post-pilot questionnaire were keen to adopt C-SATS©, and 90.9% believed C-SATS© had a positive impact on training. 36.4% reported using the platform weekly, and 54.5% monthly. Full results from the questionnaires can be found in the Appendix 1–3.
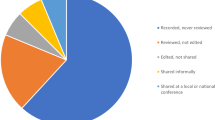
C-SATS© engagement metrics
Usage metrics were available from May 2022 to February 2023 (Fig. 2). Of the final 30 users, 26 accessed their accounts, and 16 uploaded videos to the platform. A total of 57 videos were uploaded in 24 of the 31 weeks in which the C-SATS© device was installed in operating rooms. A consistent level of uploads failed to be achieved.
a Number of case uploads per week to the C-SATS© platform. A total of 57 videos were uploaded by 16 users in 24 of the 31 weeks of the pilot when the recording device was installed in operating rooms. Source: Ethicon, (Johnson and Johnson). b Number of users engaging with the C-SATS© platform by week. Engagement is defined as logging into the C-SATS. © platform for any purpose (n = 26). Purposes include accessing the video library, expert index and profile, dashboard, community dashboard, case page, academy index and video, and other page types. Source: Ethicon, (Johnson and Johnson)
Semi-structured interviews
Demographics
A total of 13 participants were interviewed: three attending surgeons, four surgical residents, three patients, one scrub nurse, one lawyer, and one industry representative. Participants were 53.8% female, and 46.2% male. Of the seven surgeons, four were involved in the C-SATS© pilot (two residents and two attendings). One patient participant had previously undergone a laparoscopic procedure, with the others awaiting surgery. Thematic saturation was achieved, with no further codes created after the ninth interview.
Main findings
Three major sections were identified—value, barriers, and artificial intelligence. Within the ‘Barriers’ section, three major themes were identified, with nine sub-themes (Fig. 3).
Themes and sub-themes identified in the thematic analysis relating to the barriers to the implementation of routine surgical video recording with example quotations. Each sub-theme is matched to its corresponding NASSS framework domain(s). NASSS Domains: 2A—What are the key features of the technology? 3B—What is the desirability, efficacy, safety, and cost-effectiveness (demand-side value)? 4A—What changes in staff roles, practices, and identities are implied? 5A—What is the organization’s capacity to innovate? 5B—How ready is the organization for this technology-supported change? 5C—How easy will the adoption and funding decision be? 5D—What changes will be needed in team interactions and routines? 5E—What work is involved in implementation and who will do it? 6A—What is the political, economic, regulatory, professional, and sociocultural context for program rollout? 7A—How much scope is there for adapting and coevolving the technology and the service over time? 7B—How resilient is the organization to handling critical events and adapting to unforeseen circumstances?
Experience of recording
All professional participants had encountered surgical video recording. One attending recorded all cases. All patient participants were aware that procedures could be recorded. Of the participants involved in the C-SATS© pilot, all had utilized the platform at least once. 3/7 medical professional participants had experience of consenting patients for video recording during surgery. All participants felt it was important that patients were consented explicitly for recording.
Value of video recording
Educational and quality improvement
All participants saw videos as having an educational value to the surgeons, regardless of training stage. Most participants felt the value of recording was in the ability to reflect on performance outside of the operating room where the focus can be solely on education.
As a record
Several participants believed video is a better form of documentation than current methods. Most saw the video as a medicolegal record, believing video to be objective and factual evidence of the procedure. However, one attending disagreed, citing a perceived inability to establish culpability from a video. One patient stated they would have been interested in accessing the video to understand the events of their procedure, in which a serious complication had occurred.
Commercial
Most participants agreed that videos are a valuable commercial asset, which could contribute to improvements in surgical outcomes through analysis of surgical data. A commonly suggested idea was analysis of instrument data, leading to improvements in device functionality. However, some believed industry involvement was driven by financial motivation and may lose sight of patient outcomes. There was also an awareness of a general public hesitancy towards third party involvement in handling sensitive healthcare data.
Barriers
Change
Resistance
All medical professional participants expected there would be resistance around the introduction of routine surgical video recording. These concerns included exposure of performance at a lower competency than expected or fear of judgement from peers. Resident participants stated that recording may negatively impact performance due to the perception of being observed. However, it was acknowledged that this would be overcome if recording became standard.
System adaptability
All medical professionals anticipated systemic issues with adoption. Three medical professional participants believed hospitals may be limited in their abilities to adopt new technologies. Resident surgeons felt it may be challenging to demonstrate the benefit of investing in recording technology.
Integration into routine
All medical professional participants believed that a key challenge lies in embedding recording into the preoperative routine. This was particularly evident amongst the C-SATS© pilot participants who reported that use of the device was often overlooked despite availability. Participants stated that recording should simple to employ and requires engagement from the wider surgical team. All medical professional participants suggested that inclusion of recording within the preoperative checklist would enhance implementation.
Resource
Digital infrastructure
Storage of recordings was cited as a major barrier to implementation of routine recording by all professional participants. Concerns were centered around the need for extensive storage capacity if every procedure was recorded. Several medical professional participants felt that whilst cloud-based storage is the most viable option, this creates further questions around compliance with GDPR.
Financial
Cost was also discussed as a major barrier, with 75% of participants believing that storage would be the biggest cost. Other identified costs included training requirements and energy-related costs. Attending participants stated hospitals may not be willing to fund recording devices due to the challenges of demonstrating a discernable and immediate benefit to the patient.
Security
All participants expressed the need for highly secure software systems to store surgical videos. Patients highlighted the concern felt towards the prospect of their highly sensitive surgical data being released. The legal representative also raised the issue of the vulnerability of hospitals to cyberattacks, as well as the increased risk of major data breaches if large, centralized databases are used to store surgical video.
Governance
Regulatory uncertainty
Unclear regulations with reference to anonymity in a surgical procedure recording were highlighted by both the legal and industry representative. The uncertainty was focussed on the risk of reidentification of a patient through additional data linked to the video footage, such as hospital location, or the date and time of the procedure. All patient and surgeon participants, however, perceived intraabdominal footage as anonymous.
Another identified challenge was the global variation in data protection regulations, notably between the USA and UK. Both the legal and industry representative considered the obligations in the USA to be less significant than in the UK, such that the label of anonymity is given with less weight in the USA compared to the UK. Both felt it was important to have a global framework for the labelling and handling of procedure videos, due to the global nature of the technology.
Ownership
Data ownership was a less eminent issue, often requiring prompting to extract views. 12/13 participants supported a hospital ownership model. One attending believed ownership should belong to the patient. However, all patients believed there was little use owning the rights to the video. All residents believed recordings should fall under the same ownership principles as other healthcare data, like imaging.
Patient access
Patient access to their own procedure recordings proved to be an area of uncertainty. All but one participant was in favour of patient access to recordings. One commonly cited reason for patient access was the use of video to assist in patient understanding of their condition. All medical professional participants felt there was some danger of misinterpretation of intraoperative events which could lead to increased rates of litigation.
Artificial intelligence
Role of artificial intelligence
All participants were unopposed to the use of videos for algorithm generation and believed AI has a role in the future of surgery. The belief that it would reduce surgeon workload was a recurrent theme amongst all participants.
Challenges
Some participants were not confident in the ability to AI to assess technical skills, whereas others felt extensive validation would be needed before its use as an assessment tool. Resident participants felt there could be challenges with the inability of AI to appreciate the intricacies of a surgical procedure, and the need to deviate from the set course, resulting in poor performance scores. All attending participants perceived a resistance amongst colleagues to the use of decision-making or intraoperative navigation tools, which may be perceived as questioning their own decision-making.
Discussion
This study is the first to include data from a real-world recording platform, as well as utilize interviews to investigate attitudes towards routine surgical video recording and identify barriers to its adoption [12, 19, 20]. All medical professional participants in this study believed that provision of recording technology would facilitate adoption. However, only 16/30 within the C-SATS© pilot used the recording device demonstrating implementation extends beyond technological availability alone. Resistance from surgeons was identified as a significant barrier in this study in line with existing evidence [8, 20]. Many believed this to be centered on concerns that recording may alter their practice, formally known as the Hawthorne effect. However, it may be argued that this is likely to be a positive change. Video provides an objective measure of various quality control measures, such as achieving the Critical View of Safety in laparoscopic cholecystectomies, definitively showing this stage has been achieved. It is not unlikely that the resistance is linked to litigation concerns. Two participants were concerned that an increase in medicolegal action would occur due to misinterpretation of events in the video by patients although this was viewed by these participants as an area to address rather than a barrier to this technology [21]. There is a fear that use of routine recording will lead to an onslaught of litigation cases [19] despite little evidence to support these claims. Participants in fact viewed videos as a positive factor in the case of litigation as they provide a better form of medicolegal evidence than the operative note.
A key theme emerging from this study was the need for recording to be integrated into the surgical workflow. However, integrating new steps within a well-established workflow is not without difficulty and lessons can be learnt with the establishment of the World Health Organization Surgical Safety Checklist [22,23,24]. Successful implementation will require structured education and detailed explanation of the rationale. Surgical video recording may ultimately fall under the responsibility of the wider surgical team and unless buy-in is ensured by the entire team, recording may be viewed as an unnecessary task with little immediate benefit.
The most frequently identified barrier in this study was developing the required infrastructure and its associated costs. In an ecosystem where multiple digital surgical technologies are on the market, hospital managers are under pressure to justify the costs associated with implementing surgical video recording. Current commercially available recording platforms are largely focussed on education and therefore business cases will require a growing evidence base that video-based review improves surgical performance and ultimately patient outcomes [6, 7]. A potential method for hospitals to mitigate these costs is working in conjunction with industry. This study identified the importance of videos to members of the surgical technology industry. While all participants were willing to share video data with industry, this may not be representative of the entire population. Historically, the public has been resistant to third-party involvement in healthcare with a multinational survey highlighting an aversion to the sharing of public health data with private companies [25]. Clear guidelines surrounding secondary data sharing agreements and video ownership must therefore be established to ensure responsible use of personal data for commercial purposes.
Another major theme identified surrounded experiences of consenting patients for surgical video recording. While participants found patients were generally happy to allow video recording, it is unclear where additional clauses detailing sharing with third parties would be met with similar approval. Asking patients to donate their personal health information to a company who may utilize this data for commercial gain raises potential ethical questions [26]. Standardization of processes by which patients are consented for surgical video recording and the possible downstream uses will be central to maintaining transparency with patients and retaining their trust.
Finally, anonymization of video was a common theme. Whilst surgeon and patient participants considered endoscopic recordings to be fully anonymous, both the legal and industry representatives believed the risk of identification was too high to class intracorporeal videos as anonymous. Of note, Rocher et al., described an algorithm which identified 99.98% of Americans from deidentified, incomplete databases [27]. Whilst anonymity may be important to industry in terms of allowing access, it is questionable whether detaching the video from the patient’s medical record, and thus preventing linkage of video data with clinical outcomes is useful. AI tools for decision support and risk prediction will likely require full access to the entire patient profile to reach maximum analytic potential [28,29,30] and therefore efforts may be better guided to improving pseudonymization of surgical procedure recordings and ensuring adequate data protection measures are in place [31].
Through the analysis of the themes derived from these interviews, we have produced a set of recommendations for the successful implementation of routine surgical video recording (Fig. 4). These recommendations have been designed to facilitate the broad spectrum of stakeholders across surgical video recording.
This study is ultimately limited by the range of participants included within the study. Inclusion of a larger number of industry representatives would likely improve the breadth of views within our study and broader exploration through a focussed study on patient views alone around routine surgical video recording will likely enhance our understanding around failure in adoption. Furthermore, an international sample of participants would provide greater insights into the global applicability of the identified barriers. Future work may therefore consist of further semi-structured interviews or a consensus technique, such as a Delphi Consensus. It can also be argued that participants taking part in the study were more likely to be in favour of surgical video recording potentially biasing the results obtained.
Conclusions
Barriers to implementation of routine surgical video recording exist beyond the technological level alone. This study is the first thorough exploration of these barriers utilizing semi-structured interviews. We provide recommendations for improved implementation of routine surgical video recording through the synthesis of themes derived from these interviews. Integration of video recording within the surgical workflow will be a priority and will require buy-in from the wider surgical team. Furthermore, all stakeholders must be consulted including patients, who must be engaged and educated in how their data is being used.
References
St John A, Caturegli I, Kubicki NS et al (2020) The rise of minimally invasive surgery: 16 year analysis of the progressive replacement of open surgery with laparoscopy. Jsls 24(4). https://doi.org/10.4293/jsls.2020.00076
Yiu A, Lam K, Simister C et al (2024) Adoption of routine surgical video recording: a nationwide freedom of information act request across England and Wales. Eclinicalmedicine, p 70
Wauben L, Van Grevenstein W, Goossens R et al (2011) Operative notes do not reflect reality in laparoscopic cholecystectomy. J Br Surg 98(10):1431–1436
Gambadauro P, Magos A (2012) Surgical videos for accident analysis, performance improvement, and complication prevention: time for a surgical black box? Surg Innovat 19(1):76–80
Jesudason E (2023) Surgery should be routinely videoed. J Med Ethics 49(4):235–239
Augestad KM, Butt K, Ignjatovic D et al (2020) Video-based coaching in surgical education: a systematic review and meta-analysis. Surg Endosc 34:521–535
Soucisse ML, Boulva K, Sideris L et al (2017) Video coaching as an efficient teaching method for surgical residents—a randomized controlled trial. J Surg Educ 74(2):365–371
Lam K, Abràmoff MD, Balibrea JM et al (2022) A Delphi consensus statement for digital surgery. NPJ Digital Med 5(1):100
Maier-Hein L, Eisenmann M, Sarikaya D et al (2022) Surgical data science—from concepts toward clinical translation. Med Image Anal 76:102306. https://doi.org/10.1016/j.media.2021.102306[publishedOnlineFirst:2021/12/09]
Hashimoto DA, Rosman G, Rus D et al (2018) Artificial intelligence in surgery: promises and perils. Ann Surg 268(1):70–76. https://doi.org/10.1097/sla.0000000000002693[publishedOnlineFirst:2018/02/02]
Emam Z, Kondrich A, Harrison S et al (2021) On the state of data in computer vision: human annotations remain indispensable for developing deep learning models. https://ui.adsabs.harvard.edu/abs/2021arXiv210800114E. Accessed July 01, 2021.
Mazer L, Varban O, Montgomery JR et al (2022) Video is better: why aren’t we using it? A mixed-methods study of the barriers to routine procedural video recording and case review. Surg Endosc, pp 1–8.
Silas MR, Grassia P, Langerman A (2015) Video recording of the operating room–is anonymity possible? J Surg Res 197(2):272–276. https://doi.org/10.1016/j.jss.2015.03.097[publishedOnlineFirst:20150409]
Strandbygaard J, Dose N, Moeller KE et al (2022) Healthcare professionals' perception of safety culture and the Operating Room (OR) Black Box technology before clinical implementation: a cross-sectional survey. BMJ Open Qual 11(4). https://doi.org/10.1136/bmjoq-2022-001819
Makary MA (2013) The power of video recording: taking quality to the next level. JAMA 309(15):1591–1592. https://doi.org/10.1001/jama.2013.595
Rex DK, Hewett DG, Raghavendra M et al (2010) The impact of videorecording on the quality of colonoscopy performance: a pilot study. Official J Am College Gastroenterol| ACG 105(11):2312–2317.
Bergström H, Larsson L-G, Stenberg E (2018) Audio-video recording during laparoscopic surgery reduces irrelevant conversation between surgeons: a cohort study. BMC Surg 18(1):1–5
Greenhalgh T, Wherton J, Papoutsi C et al (2017) Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 19(11):e367. https://doi.org/10.2196/jmir.8775[publishedOnlineFirst:20171101]
Peled-Raz M, Willner N, Shteinberg D et al (2019) Digital recording and documentation of endoscopic procedures: physicians’ practice and perspectives. Israel J Health Policy Res 8:1–12
van de Graaf FW, Eryigit Ö, Lange JF (2021) Current perspectives on video and audio recording inside the surgical operating room: results of a cross-disciplinary survey. Updat Surg 73:2001–2007
Willner N, Peled-Raz M, Shteinberg D, Shteinberg M, Keren D, Rainis T (2016) Digital recording and documentation of endoscopic procedures: do patients and doctors think alike? Can J Gastroenterol Hepatol 2016:2493470. https://doi.org/10.1155/2016/2493470
Treadwell JR, Lucas S, Tsou AY (2014) Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf 23(4):299–318
Conley DM, Singer SJ, Edmondson L et al (2011) Effective surgical safety checklist implementation. J Am Coll Surg 212(5):873–879
Kasatpibal N, Senaratana W, Chitreecheur J et al (2012) Implementation of the World Health Organization surgical safety checklist at a university hospital in Thailand. Surg Infect 13(1):50–56
Patil S, Patruni B, Potoglou D et al (2016) Public preference for data privacy—a pan-European study on metro/train surveillance. Transportation Res A Policy Pract 92:145–161
Prigoff JG, Sherwin M, Divino CM (2016) Ethical recommendations for video recording in the operating room. Ann Surg 264(1):34–35. https://doi.org/10.1097/sla.0000000000001652[publishedOnlineFirst:2016/04/29]
Rocher L, Hendrickx JM, De Montjoye Y-A (2019) Estimating the success of re-identifications in incomplete datasets using generative models. Nat Commun 10(1):1–9
Cheikh Youssef S, Haram K, Noël J et al (2023) Evolution of the digital operating room: the place of video technology in surgery. Langenbecks Arch Surg 408(1):95
Loftus TJ, Altieri MS, Balch JA et al (2023) Artificial intelligence–enabled decision support in surgery: state-of-the-art and future directions. Ann Surg 278(1):51–58
Byerly S, Maurer LR, Mantero A et al (2021) Machine learning and artificial intelligence for surgical decision making. Surg Infect 22(6):626–634
El Emam K, Rodgers S, Malin B (2015) Anonymising and sharing individual patient data. BMJ, p 350
Acknowledgements
Dr Lam is supported by a NIHR Academic Clinical Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr James Kinross is a share holder in Surgease Ltd and Medical iSight Ltd. Dr Lam, Miss Simister, and Dr Yiu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lam, K., Simister, C., Yiu, A. et al. Barriers to the adoption of routine surgical video recording: a mixed-methods qualitative study of a real-world implementation of a video recording platform. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11174-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-11174-2