Abstract
Background
Laparoscopic repair of duodenal atresia (LRDA) remains a technically challenging procedure and its benefits ambiguous. To assess the safety and efficacy of LRDA, we performed a systematic review of techniques and material for LRDA and a meta-analysis comparing outcomes with open repair (OR).
Methods
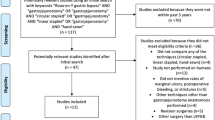
Comprehensive search of EMBASSE, PubMed and Cochrane was performed from 2000 to 2023. Studies comparing LRDA with OR were identified and outcomes extracted included operative time, time to enteral feeds, length of hospitalisation, anastomotic leaks and stricture and total complications. χ2 was used to assess associations between complications and conversions rates of different LRDA approaches (laparoscopic technique, suturing technique). Comprehensive meta-analysis was used for Meta-analysis.
Results
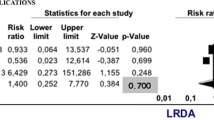
Twelve studies were identified and 1731 patients were enrolled in the study (398 [LRDA] and 1325 [OR]). Total rate of complications and conversion for LRDA was 15.58% and 18.84%, respectively. Complication rates were not significantly affected by operative technique and suturing technique. Conversion rates were not significantly affected operative technique; using a combination of interrupted and running suturing was significantly higher than using running or interrupted (χ2 = 7.45, p < 0.05). Anastomotic leaks, strictures and total complications were equivocal between LRDA and OR (OR 1.672, 95% CI 0.796–3.514; OR 2.010, 95% CI 0.758–5.333; OR 1.172, 95% CI 0.195–7.03). Operative time was significantly greater for LRDA (SDM 1.035, 95% CI 0.574–1.495, p < 0.001). Time to initial and full enteral feeds and length of hospitalisation were shorter in the LRDA group (SDM − 0.493, 95% CI − 2.166 to 1.752, p = 0.466; SDM − 0.207, 95% CI − 1.807 to 0.822, p = 0.019; SDM − 0.111, 95% CI − 1.101 to 0.880, p = 0.466, respectively).
Conclusions
LRDA showed equivalent complication rates compared to OR with an additional benefit of quicker establishment of feeds. There was no significant difference in complication and conversion rates between laparoscopic techniques. Despite a longer operative time, LRDA provides a safe minimal access approach for neonates after this consistent implementation of the technique in the past decade.






Similar content being viewed by others
References
Bethell GS, Long A-M, Knight M, Hall NJ (2020) Congenital duodenal obstruction in the UK: a population-based study. Arch Dis Child 105:178–183
Kimura K, Mukohara N, Nishijima E, Muraji T, Tsugawa C, Matsumoto Y (1990) Diamond-shaped anastomosis for duodenal atresia: an experience with 44 patients over 15 years. J Pediatr Surg 25:977–979
Gracie DJ, Lam JPH (2023) Laparoscopic duodenoduodenostomy: local experience, outcomes and points of practice. J Ped Endosc Surg 5:7–11
Bax NM, Ure BM, van der Zee DC, van Tuijl I (2001) Laparoscopic duodenoduodenostomy for duodenal atresia. Surg Endosc 15:217
van der Zee DC (2011) Laparoscopic repair of duodenal atresia: revisited. World J Surg 35:1781–1784
Zhang J, Xu X, Wang X, Zhao L, Lv Y, Chen K (2022) Laparoscopic versus open repair of congenital duodenal obstruction: a systematic review and meta-analysis. Pediatr Surg Int 38:1507–1515
Mentessidou A, Saxena AK (2017) Laparoscopic repair of duodenal atresia: systematic review and meta-analysis. World J Surg 41:2178–2184
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Spilde TL, St Peter SD, Keckler SJ, Holcomb GW, Snyder CL, Ostlie DJ (2008) Open vs laparoscopic repair of congenital duodenal obstructions: a concurrent series. J Pediatr Surg 43:1002–1005
Cruz-Centeno N, Stewart S, Marlor DR et al (2023) Duodenal atresia repair: a single-center comparative study. Am Surg 89:5911–5914
Weller JH, Engwall-Gill AJ, Westermann CR, Patel PP, Kunisaki SM, Rhee DS (2022) Laparoscopic versus open surgical repair of duodenal atresia: a NSQIP-pediatric analysis. J Surg Res 279:803–808
Williams SA, Nguyen ATH, Chang H, Danielson PD, Chandler NM (2022) Multicenter comparison of laparoscopic versus open repair of duodenal atresia in neonates. J Laparoendosc Adv Surg Tech A 32:226–230
Sidler M, Djendov F, Curry JI, Blackburn S, Giuliani S, Eaton S, Mullassery D, Cross KM, De Coppi P (2020) Potential benefits of laparoscopic repair of duodenal atresia: insights from a retrospective comparative study. Eur J Pediatr Surg 30:33–38
Holler A-S, Muensterer OJ, Martynov I, Gianicolo EA, Lacher M, Zimmermann P (2019) Duodenal atresia repair using a miniature stapler compared to laparoscopic hand-sewn and open technique. J Laparoendosc Adv Surg Tech 29:1216–1222
Gfroerer S, Theilen T-M, Fiegel HC, Rolle U (2018) Laparoscopic versus open surgery for the repair of congenital duodenal obstructions in infants and children. Surg Endosc 32:3909–3917
Cho MJ, Kim DY, Kim SC, Namgoong JM (2017) Transition from laparotomy to laparoscopic repair of congenital duodenal obstruction in neonates: our early experience. Front Pediatr 5:203
Son TN, Kien HH (2017) Laparoscopic versus open surgery in management of congenital duodenal obstruction in neonates: a single-center experience with 112 cases. J Pediatr Surg 52:1949–1951
Parmentier B, Peycelon M, Muller C-O, El Ghoneimi A, Bonnard A (2015) Laparoscopic management of congenital duodenal atresia or stenosis: a single-center early experience. J Pediatr Surg 50:1833–1836
Jensen AR, Short SS, Anselmo DM, Torres MB, Frykman PK, Shin CE, Wang K, Nguyen NX (2013) Laparoscopic versus open treatment of congenital duodenal obstruction: multicenter short-term outcomes analysis. J Laparoendosc Adv Surg Tech 23:876–880
Hill S, Koontz CS, Langness SM, Wulkan ML (2011) Laparoscopic versus open repair of congenital duodenal obstruction in infants. J Laparoendosc Adv Surg Tech A 21:961–963
Miscia ME, Lauriti G, Lelli Chiesa P, Zani A (2019) Duodenal atresia and associated intestinal atresia: a cohort study and review of the literature. Pediatr Surg Int 35:151–157
Hasegawa T, Takano S, Masuda K, Fujiwara Y, Miyahara A, Miura M (2023) Retrospective analysis of neonatal surgery at Tottori University over the past ten years. Yonago Acta Med 66:413–421
Liang Z, Lan M, Xu X, Liu F, Tao B, Zeng J (2023) Diamond-shaped versus side-to-side anastomotic duodenoduodenostomy in laparoscopic management of annular pancreas in children: a single-center retrospective comparative study. Transl Pediatr 12(10):1791–1799. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10644016/. Accessed 2 Dec 2023
Oh C, Lee S, Lee S-K, Seo J-M (2017) Laparoscopic duodenoduodenostomy with parallel anastomosis for duodenal atresia. Surg Endosc 31:2406–2410
Valusek PA, Spilde TL, Tsao K, St Peter SD, Holcomb GW, Ostlie DJ (2007) Laparoscopic duodenal atresia repair using surgical U-clips: a novel technique. Surg Endosc 21:1023–1024
Fujii T, Tanaka A, Katami H, Shimono R (2021) Stapled versus hand-sewn intestinal anastomosis in pediatric patients: a systematic review and meta-analysis. BMC Pediatr 21:435
Westwood E, Saxena AK (2022) Pitfalls in laparoscopic duodenal atresia repair requiring modifications in approach based on literature review. J Ped Endosc Surg 4:13–16
Etlinger P, Barroso C, Miranda A et al (2022) Characterization of technical skill progress in a standardized rabbit model for training in laparoscopic duodenal atresia repair. Surg Endosc 36:2456–2465
Guelfand M, Harding C (2021) Laparoscopic management of congenital intestinal obstruction: duodenal atresia and small bowel atresia. J Laparoendosc Adv Surg Tech A 31:1185–1194
Marcadis AR, Romain CV, Alkhoury F (2019) Robotic duodeno-duodenostomy creation in a pediatric patient with idiopathic duodenal stricture. J Robotic Surg 13:695–698
Sanders RD, Davidson A (2009) Anesthetic-induced neurotoxicity of the neonate: time for clinical guidelines? Paediatr Anaesth 19:1141–1146
Hall NJ, Kitteringham L, Ron O, Stedman F, Stanton M, Wheeler R, Jones C, Smyth R, Keys C (2023) A minimally interventional approach to oesophageal atresia repair with early enteral feeding is safe, optimises neonatal outcomes, and reduces resource use. J Pediatr Surg S0022–3468(23):00563–00568
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Laura Martou and Amulya Kumar Saxena have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martou, L., Saxena, A.K. Laparoscopic repair of duodenal atresia: systematic review and meta-analysis after consistent implementation of the technique in the past decade. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10828-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10828-5