Abstract
Objectives
Lung volume reduction surgery (LVRS) has proven an effective treatment for emphysema, by decreasing hyperinflation and improving lung function, activity level and reducing dyspnoea. However, postoperative air leak is an important complication, often leading to reoperation.
Our aim was to analyse reoperations after LVRS and identify potential predictors.
Methods
Consecutive single-centre unilateral VATS LVRS performed from 2017 to 2022 were included. Typically, 3–5 minor resections were made using vascular magazines without buttressing. Data were obtained from an institutional database and analysed. Multivariable logistic regression was used to identify predictors of reoperation. Number and location of injuries were registered.
Results
In total, 191 patients were included, 25 were reoperated (13%). In 21 patients, the indication for reoperation was substantial air leak, 3 patients bleeding and 1 patient empyema. Length of stay (LOS) was 21 (11–33) vs. 5 days (3–11), respectively. Only 3 injuries were in the stapler line, 13 within < 2cm and 15 injuries were in another site. Multivariable logistic regression analysis showed that decreasing DLCO increased risk of reoperation, OR 1.1 (1.03, 1.18, P = 0.005). Resections in only one lobe, compared to resections in multiple lobes, were also a risk factor OR 3.10 (1.17, 9.32, P = 0.03). Patients undergoing reoperation had significantly increased 30-day mortality, OR 5.52 (1.03, 26.69, P = 0.02).
Conclusions
Our incidence of reoperation after LVRS was 13% leading to prolonged LOS and increased 30-day mortality. Low DLCO and resections in a single lobe were significant predictors of reoperation. The air leak was usually not localized in the stapler line.
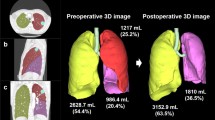
Graphical abstract
Key question: What characterizes reoperations after lung volume reduction surgeries?
Key findings: Lung injuries were predominantly located away from the original surgical site.
Take home message: Lung injuries remote from the stapler line is frequent during reoperation after lung volume reduction surgery.
Location of lung injuries found during reoperation after lung volume reduction surgery

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lung volume reduction surgery (LVRS) is an acknowledged treatment of severe emphysema. It increases walking distance and quality of life [1]. However, air leak continues to be a considerable challenge in the postoperative patient care. Prolonged air leak (PAL) increases length of hospital stay, readmission rate, intensive care unit (ICU) admission and postoperative pneumonia [2].
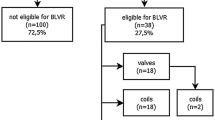
Since the National Emphysema Treatment Trial (NETT) [3] was carried out more than 20 years ago, LVRS has evolved. More LVRS centres focus on minimally invasive approaches introducing video-assisted thoracoscopic surgery (VATS) instead of median sternotomy or thoracotomy. The quality of paraclinical tools used in patient selection has improved, especially with the single-photon emission computed tomography (SPECT) scans and computed tomography (CT) software, providing a more accurate emphysema assessment in the lung tissue.
PAL is the primary challenge after LVRS, with prolonged PAL (> 7 days) incidence of 24–46% [4].
In NETT, an interim analysis identified a subgroup of patients with high mortality. These patients had Forced Expiratory Volume in 1s (FEV1) < 20% of predicted and either diffusing capacity for carbon monoxide (DLCO) < 20% of predicted or homogenous emphysema. As a consequence, patients with these characteristics have subsequently often been excluded from LVRS. In this fragile patient group, the 30-day mortality rate reported was 16% compared to 2.2% for patients not in the high-risk group. Predictors for PAL were low DLCO, predominant upper lobe disease and extensive pleural adhesions [2].
Our aim in this study was to identify predictors for reoperation and to characterize the intraoperative findings and surgical outcomes.
Patients and methods
Patient selection
The study was approved by the Institutional Review Board. Patient informed consent was not required. Conducted as a retrospective cohort study, we included a consecutive series of patients with moderate to severe emphysema eligible for unilateral LVRS from 2017 to 2022. Lung function and medical history were screened according to the inclusion criteria listed in Table 1 before preoperative workup.
Eligible patients were submitted to physical evaluation and additional testing at the department. This included medical and surgical history, comorbidity, symptoms, smoking status, cardiology evaluation including echocardiography, blood gas, 6-min-walking test (6MWT), lung function evaluation by spirometry, body plethysmography and DLCO.
Subsequently, all patients were discussed at a multidisciplinary team meeting (MDT), which included a pulmonologist, thoracic surgeon, cardiothoracic radiologist and clinical physiology specialist present. Patient history was presented, high-resolution computed tomography (HRCT) and ventilation perfusion scintigraphy including SPECT/CT imaging were evaluated, and treatment strategy for the patient was planned, including resections on a sublobar level.
Surgical approach
In 2017, the standardized surgical protocol for LVRS was reformed after a clinical immersion at the Department of Thoracic Surgery, University Hospital Zürich, Switzerland. Depending on suitable target areas on SPECT, several minor wedge resections were preferred in order to diminish tissue stress [5]. With this approach, target areas could be located in more than one lobe, though the traditional horseshoe-shaped resection across the upper lobe was still applied if indicated.
Surgeries were performed using a “standard anterior approach” [6] and only by experienced surgeons. Atraumatic techniques were applied, including only use of peanuts to gently retract the lung. One to six minor resections were made by stapling with vascular tan Tri-Staple™ Technology cartilages without buttressing, followed by water test to visualize possible air leaks. Lastly, two Ch 20 chest drains were inserted and connected to a digital drainage system (Topaz Plus) using 2 cmH20 suction. [7]. If postoperative subcutaneous emphysema developed, an additional third chest drain was considered as an alternative to increasing suction pressure. This was done to prevent enlarging of the fistula or creating further lung injury. Pain management was administered in line with our standard protocol [8].
When the patient was ready for extubation, the double lumen tube was replaced with a laryngeal mask, to prevent coughing and adjoining development of air leaks.
From the first postoperative day, patients were encouraged to physical activity within the physical limitations and with the assistance of a physiotherapist.
The final drain was removed when air leak was < 20 ml/min and fluid loss < 500 ml both for 12 continuous hours, and the patient had been sufficiently mobilized. Two hours after drain removal a chest x-ray was performed.
The indication for reoperation was set by the operating surgeon and established on the basis of a clinical evaluation including appearance of considerable subcutaneous emphysema and the severity of either haemorrhage or air leak. The latter with an approximate cut-off of 1500 ml/min or increasing. For this patient group, reoperation was preferred. Patients with minor air leak for several days were offered blood pleurodesis.
Statistics
Our primary aim of this study was to review the reoperations performed on this patient group and determine the location of the air leaks. We then compared the surgical outcomes for the reoperated group and the not reoperated group to investigate, whether reoperation constituted a risk. Lastly, we conducted a multivariable logistic regression to isolate predictors for reoperation.
Summary data are presented as mean including standard deviation for parametric data and median including interquartile range for nonparametric data, using appropriate statistical tests.
The categorical postoperative variables were compared individually using the X2-test to stratify the surgical outcomes for the two groups. Preoperative variables listed in Table 2 were tested with univariable logistic regression with the outcome “reoperation”. Variables with P < 0.1 at univariable analysis were included in the multivariable logistic regression. Overall, P values < 0.05 were accepted as statistically significant.
All statistical calculations were carried out using R Studio 2022.07.2 (The R Foundation for Statistical Computing, Vienna, Austria) and performed by the authors alone.
Results
A total of 191 unilateral LVRS procedures were performed, whereas 21 of these procedures were subsequent contralateral resections. The median age was 65 years (IQR: 59.0–70.5) and 59% were female. Additional preoperative characteristics are listed in Table 2.
Collectively, 25 patients were reoperated within 30 days of the primary procedure (13%). In 21 patients (84%), the indication was substantial air leak. Three patients (12%) were reoperated for bleeding and one patient (4%) for an empyema.
In one patient reoperated for massive air leak, we were not able to localize any lung injuries at all.
In total 33 lung injuries were revealed. Eight patients had more than one injury. The location of injuries is depicted in Fig. 1 and Table 3.
The reoperated patients had significantly longer LOS 21 vs. 5 days, more days with chest drain OR 1.11 (95% confidence interval, CI 1.07, 1.17, P < 0.001), and PAL OR 5.9 (CI 2.35, 16.94, P < 0.001).
The 30-day mortality was significantly increased for the reoperated patients. The risk of ICU admission for the two groups did not differ (Table 4).
All three patients in the reoperated group died from respiratory failure within few days from the surgery. One was complicated by an empyema. In the not reoperated group, one patient suffered mesenterial ischaemia and respiratory failure and died subsequently. One died from a pressure pneumothorax and the remaining two patients died from respiratory failure.
Multivariable logistic regression analysis showed that decreasing DLCO significantly increased the risk of reoperation by OR 1.1 (CI 1.03, 1.18, P = 0.005). Furthermore, resections in only one lobe compared to resections in multiple lobes were a risk factor with OR 3.10 (CI 1.17, 9.32, P = 0.03). Number of staplers or resections did not affect the risk of reoperation (Table 5). Risk of reoperation for patients resected in the upper lobe compared to patients resected in non-upper lobes was not significant. Charlson Comorbidity Index (CCI) and COPD Assessment Test (CAT) were significant in the simple logistic regression, however not in the multiple regression model.
Discussion
The incidence of reoperation after LVRS in this population was 13%, which is higher than in comparable studies. In the NETT reoperation for air leak was 3.3% [9]. Reoperation rates are reported up to 13% [10].
The criteria for reoperation vary among centres. In this study, the operating surgeon decided the indication for reoperation, often resulting in reoperation few days after the primary operation. Other reports have not scheduled reoperations for massive air leak before 15 days if not resolved prior [11].
Hospital LOS was six days in total, with five days and 21 days for the not reoperated and reoperated patients, respectively. This is in line with other studies, where overall LOS was 10–14 days collectively [9]. Expectedly, the reoperated group had significantly longer LOS.
The 30-day mortality rate was 4% in total, which is similar to other studies (2.4%–4%) [12]. However, 30-day mortality was significantly higher in the reoperated group compared to the non-reoperated group (12% vs. 2%).
In this study, PAL > 7days was at 30% and 72% in the non-reoperated and reoperated group, respectively. PAL for LVRS is reported at 46–80% for PAL > 7 days [13]. With these high numbers, PAL is the most common complication after LVRS, causing morbidity and mortality, and increasing medical costs. Reducing PAL presents the most significant challenge in improving the surgical course for LVRS [14]. In this study, we focus on findings during reoperations in an attempt to characterize the air leaks further. We found that only few patients had an air leak in the stapler line (9%) or adjacent to a pleural adhesion (6%). More than 80% of the lung injuries were located away from the surgical site, which indicates that the general pathology of emphysematic lung tissue presents the actual challenge.
Standard approach is to test for air leak before the end of the procedure, and therefore, it is speculated that some of the air leaks might not be present until after the primary surgery, and therefore caused by the physiologic changes in the lung tissue rather than by a specific surgical trauma [11].
Pneumothorax is the primary complication to bronchial lung volume reduction with endobronchial valves (EBV). Recently published data from the CELEB trial showed an incidence of pneumothorax as high as 30.4% [15]. Another study found that 43% of cases were complicated by pneumothorax needing additional treatment for persistent air leak besides chest drain [16].
Peripheral injury occurring after central intervention coincides with our theory, that the underlying lung disease is the problem rather than iatrogenic injuries.
An earlier study concluded that air leak occurred primarily in the proximal stapler line and buttressed staplers with bovine pericardium effectively minimized these leaks [17]. Also, buttressed staplers have proved effectively decreasing days with chest drain; however, LOS and rate of reoperation were unaffected [18]. Furthermore, buttressed staplers have been reported to induce serious complications such as haemoptysis, metalloptysis and interstitial pneumonia [19].
In this study, we found very few lung injuries in the stapler lines. It is hypothesized in other studies, that the staplers redistribute forces across the tissue, creating subsequent tears and air leaks remote from the resection site [20]. In that case, buttressing will not provide additional effect. Our use of Tri staple technology originates from the intention of distributing the tension on the tissue evenly. The choice of vascular staplers originates in the presumption that it will minimize the injuries in this very thin and vulnerable emphysematous tissue. However, scientific verification of this is absent. Mainly because of the intraoperative findings in this study, we do not suspect buttressed stapler will solve the challenge of postoperative airleaks in this patient group. However, in light of the steep reoperation rate and high mortality rate in the reoperated group, we continuously consider all improvements in our procedures to bring down the rate of complications.
Untraditional surgical techniques have been explored to reduce or solve the issue of air leak. Tacconi et al. introduced plication on awake patients using epidural analgesia and had PAL in only 18% of the cases [11]. Results being ambiguous on this subject and pointing to air leaks away from the stapler line, it should be thoroughly considered whether the extra cost of applying buttressed staplers is reasonable.
Our results indicate that resections in only one lobe increase the risk of reoperation. It is hypothesized that spreading the resection to several lobes would minimize the tension on the lung tissue and therefore protect against air leak [4]. But the exact mechanism has yet to be uncovered. It has been suggested by Cooper et al [21]. that a surgical approach, where one continuous line of excision is preferred, over several wedge excisions, prevents air leak. This approach has later in general been changed towards performing several minor resections [5]. We believe our data contribute to this knowledge, with reduction of airleak by distributing resections on multiple lobes.
Only two of the 33 injuries found during reoperation were coinciding with a pleural adherence. As clinical experience indicates that pleural adherences increase risk of postoperative air leak, we expected a substantially greater incidence. Furthermore, pleural adhesions have been found to increase the risk and duration of air leak in the NETT [2]. For endobronchial lung volume reduction, pleural adherences have been identified as a predictor of pneumothorax [22].
Pleural adhesions could possibly still be a risk factor for the patients who were not reoperated. These data from the primary surgery are not available.
Some surgeons prefer a surgical technique where a pleural tent is performed during the primary surgery, to prevent postoperative air leak [23]. A meta-analysis confirmed similar findings for lobectomies [24]. Adversely, the pleural tent procedure has also been tried on patients with primary or secondary pneumothorax, with increasing LOS and days with chest drain as a result [25].
At our centre, pleural tent is not standard of care, merely intermittently used as additional measure against air leak during reoperation.
During the 5-year period of data collection, the indication for pleural tent has gradually changed and is now used more frequently during reoperation, as a method of diminishing air leak. One of the obvious benefits of this procedure is the lack of foreign body involvement.
EBV as treatment for PAL have been evaluated in a review from 2015 [26]. The review included air leak of all causes including surgical complication; however, most air leaks seized within 24 h. These results point to EBV being a possible way of handling PAL in cases, where reoperation is contraindicated or a non-favourable option. The issue of collateral ventilation and bronchoscopic location of the air leak does constitute a challenge [27].
Sealants are often applied as a supplement to staplers in order to prevent air leak after lung surgery. A systematic Cochrane review on effect of sealants in lung surgery uncovered reduced air leak in 12 out of 16 trials; however, it did not translate into reduced LOS [28].
Autologous fibrin sealants could reduce the incidence of PAL and duration of chest drainage after LVRS [29, 30]. However, from a cost/benefit perspective, postoperative autologous blood patch pleurodesis could be a more sensible choice.
A review from 2021 showed effectiveness of postoperative autologous blood pleurodesis on treating air leak within 48 h for 85.7% of patients with postoperative air leak [31], however not focussing solely on LVRS patients. It has not been explored whether this treatment is effective and safe in a LVRS population. We do not find the scientific evidence for the effect of chemical pleurodesis sufficient [32], and furthermore, we are reluctant to use chemical because the concomitant pleural adherences can cause surgical challenges related to potential later lung transplantation.
We found that low DLCO and resections in only one lobe instead of several lobes were predictors of reoperation. Isolated upper lobe resection showed no effect on reoperation rate in our study.
In the NETT, PAL was associated with low DLCO, pleural adhesions, predominantly upper lobe disease, steroid usage and Caucasian race. Mortality did not differ for the PAL group; however, rate of postoperative pneumonia and admission to the intensive care unit were increased [2, 3].
The NETT group did specify a high-risk patient group with DLCO < 20% or FEV1 < 20% with increased mortality risk [3]. As a consequence, several centres have incorporated a DLCO < 20% as an exclusion criterion for surgery. However, improvement of lung function following LVRS has even been proved beyond the NETT criteria for DLCO down to 15% without increased mortality [3, 33]. Pursuing to minimize the risk of reoperation in our centre, increasing the DLCO cut-off is a possibility.
The retrospective nature of this study presents an obvious limitation. The small sample size and the indication for reoperation set by the individual surgeon also present a limitation, though we have no evidence to support expectations of a different outcome with a more conservative or aggressive approach. Not many manuscripts have been published on complications after LVRS despite the massive challenge of PAL. The data presented in this manuscript provide insights into this challenge.
Conclusion
Air leak is the predominant reason for reoperation in LVRS and is associated with increased LOS and mortality. Minimizing air leak therefore remains the main challenge in LVRS.
During reoperations, we found injuries predominantly occurred away from the stapler line. This contributes to current knowledge of understanding the pathology of postoperative air leak.
Predictors for reoperation were low DLCO and resections in only one lobe, suggesting that multiple minor resections in several lobes are preferred. Indication for LVRS should be carefully evaluated in patients with low DLCO.
Abbreviations
- A1AD:
-
Alpha 1 anti-trypsin deficiency
- BMI:
-
Body Mass Index
- BLVR:
-
Bronchial lung volume reduction
- CAT:
-
COPD assessment test
- CCI:
-
Charlson comorbidity index
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- DLCO:
-
Diffusion capacity of the lung for carbon monoxide
- EBV:
-
Endobronchial valves
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- HRCT:
-
High-resolution computed tomography
- LOS:
-
Length of stay
- LTOT:
-
Long-term oxygen treatment
- LVEF:
-
Left ventricle ejection fraction
- LVRS:
-
Lung volume reduction surgery
- MRC:
-
Medical research council dyspnoea score
- NETT:
-
Nation emphysema treatment trial
- PAL:
-
Prolonged air leak
- RV:
-
Residual volume
- SPECT:
-
Single-photon emission computed tomography
- TLC:
-
Total lung capacity
- RV:
-
Residual volume
- VATS:
-
Video-assisted thoracoscopic surgery
- 6MWT:
-
Six-minute walking test
References
Huang W, Wang WR, Deng B, Tan YQ, Jiang GY, Zhou HJ, He Y (2011) Several clinical interests regarding lung volume reduction surgery for severe emphysema: meta-analysis and systematic review of randomized controlled trials. J Cardiothorac Surg. https://doi.org/10.1186/1749-8090-6-148
DeCamp MM, Blackstone EH, Naunheim KS, Krasna MJ, Wood DE, Meli YM, McKenna RJ (2006) Patient and surgical factors influencing air leak after lung volume reduction surgery: lessons learned from the National Emphysema Treatment Trial. Ann Thorac Surg 82:197–207. https://doi.org/10.1016/J.ATHORACSUR.2006.02.050
National Emphysema Treatment Trial Research Group (2001) Patients at high risk of death after lung-volume-reduction surgery. N Engl J Med 345:1075–1083. https://doi.org/10.1056/NEJMOA11798
Dugan KC, Laxmanan B, Murgu S, Hogarth DK (2017) Management of Persistent Air Leaks. Chest 152:417–423. https://doi.org/10.1016/J.CHEST.2017.02.020
Weder W, Tutic M, Bloch KE (2009) Lung volume reduction surgery in nonheterogeneous emphysema. Thorac Surg Clin 19:193–199. https://doi.org/10.1016/J.THORSURG.2009.03.002
Hansen HJ, Petersen RH, Christensen M (2011) Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 25:1263–1269. https://doi.org/10.1007/S00464-010-1355-9
Holbek BL, Christensen M, Hansen HJ, Kehlet H, Petersen RH (2019) The effects of low suction on digital drainage devices after lobectomy using video-assisted thoracoscopic surgery: a randomized controlled trial†. Eur J Cardiothorac Surg 55:673–681. https://doi.org/10.1093/EJCTS/EZY361
Wildgaard K, Petersen RH, Hansen HJ, Sørensen HM, Ringsted TK, Kehlet H (2012) Multimodal analgesic treatment in video-assisted thoracic surgery lobectomy using an intraoperative intercostal catheter. Eur J Cardiothorac Surg 41:1072–1077. https://doi.org/10.1093/EJCTS/EZR151
DeCamp MM, McKenna RJ, Deschamps CC, Krasna MJ (2008) Lung volume reduction surgery: technique, operative mortality, and morbidity. Proc Am Thorac Soc 5:442. https://doi.org/10.1513/PATS.200803-023ET
Date H, Goto K, Souda R, Nagashima H, Togami I, Endou S, Aoe M, Yamashita M, Andou A, Shimizu N (1998) Bilateral lung volume reduction surgery via median sternotomy for severe pulmonary emphysema. Ann Thorac Surg 65:939–942. https://doi.org/10.1016/S0003-4975(98)00115-5
Tacconi F, Pompeo E, Mineo TC (2009) Duration of air leak is reduced after awake nonresectional lung volume reduction surgery. Eur J Cardiothorac Surg 35:822–828. https://doi.org/10.1016/J.EJCTS.2009.01.010
Weder W, Tutic M, Lardinois D, Jungraithmayr W, Hillinger S, Russi EW, Bloch KE (2009) Persistent benefit from lung volume reduction surgery in patients with homogeneous emphysema. Ann Thorac Surg 87:229–237. https://doi.org/10.1016/j.athoracsur.2008.10.012
Ciccone AM, Meyers BF, Guthrie TJ, Davis GE, Yusen RD, Lefrak SS, Patterson GA, Cooper JD, Kaiser LR, Rice TW (2003) Long-term outcome of bilateral lung volume reduction in 250 consecutive patients with emphysema. J Thorac Cardiovasc Surg 125:513–525. https://doi.org/10.1067/mtc.2003.147
Varela G, Jiménez MF, Novoa N, Aranda JL (2005) Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg 27:329–333. https://doi.org/10.1016/J.EJCTS.2004.11.005
Buttery SC, Banya W, Bilancia R, Boyd E, Buckley J, Greening NJ, Housely K, Jordan S, Kemp SV, Kirk AJB, Latimer L, Lau K, Lawson R, Lewis A, Moxham J, Rathinam S, Steiner MC, Tenconi S, Waller D, Shah PL, Hopkinson NS (2023) Lung volume reduction surgery versus endobronchial valves: a randomised controlled trial. Eur Respir J. https://doi.org/10.1183/13993003.02063-2022
Low SW, Swanson KL, Lee JZ, Tan MC, Cartin-Ceba R, Sakata KK, Maldonado F (2022) Complications of endobronchial valve placement for bronchoscopic lung volume reduction: insights from the food and drug administration manufacturer and user facility device experience (MAUDE). J Bronchology Interv Pulmonol 29:206–212. https://doi.org/10.1097/LBR.0000000000000859
Whitlark JD, Hsu HK (1994) Technique to reduce air leaks after the resection of emphysematous lung. Ann Thorac Surg 58:1560. https://doi.org/10.1016/0003-4975(94)91966-6
Stammberger U, Klepetko W, Stamatis G, Hamacher J, Schmid RA, Wisser W, Hillerjan L, Weder W (2000) Buttressing the staple line in lung volume reduction surgery: a randomized three-center study. Ann Thorac Surg 70:1820–1825. https://doi.org/10.1016/S0003-4975(00)01903-2
Provencher S, Deslauriers J (2003) Late complication of bovine pericardium patches used for lung volume reduction surgery. Eur J Cardiothorac Surg 23:1059–1061. https://doi.org/10.1016/S1010-7940(03)00155-6
Fischel RJ, McKenna RJ (1998) Bovine pericardium versus bovine collagen to buttress staples for lung reduction operations. Ann Thorac Surg 65:217–219. https://doi.org/10.1016/S0003-4975(97)01189-2
Cooper JD, Patterson GA, Sundaresan RS, Trulock EP, Yusen RD, Pohl MS, Lefrak SS, Benfield JR, Vaughn CC (1996) Results of 150 consecutive bilateral lung volume reduction procedures in patients with severe emphysema. J Thorac Cardiovasc Surg 112:1319–1330. https://doi.org/10.1016/S0022-5223(96)70147-2
Van Geffen WH, Klooster K, Hartman JE, Ten Hacken NHT, Kerstjens HAM, Wolf RFE, Slebos DJ (2017) Pleural adhesion assessment as a predictor for pneumothorax after endobronchial valve treatment. Respiration 94:224–231. https://doi.org/10.1159/000477258
Venuta F, De Giacomo T, Rendina EA, Ricci C, Coloni GF (1998) Thoracoscopic pleural tent. Ann Thorac Surg 66:1833–1834. https://doi.org/10.1016/S0003-4975(98)00921-7
Uzzaman MM, Daniel Robb J, Mhandu PCE, Khan H, Baig K, Chaubey S, Whitaker DC (2014) A meta-analysis assessing the benefits of concomitant pleural tent procedure after upper lobectomy. Ann Thorac Surg 97:365–372. https://doi.org/10.1016/J.ATHORACSUR.2013.08.013
Kawachi R, Matsuwaki R, Tachibana K, Karita S, Nakazato Y, Tanaka R, Nagashima Y, Takei H, Kondo H (2016) Thoracoscopic modified pleural tent for spontaneous pneumothorax. Interact Cardiovasc Thorac Surg 23:190–194. https://doi.org/10.1093/ICVTS/IVW107
Gkegkes ID, Mourtarakos S, Gakidis I (2015) Endobronchial valves in treatment of persistent air leaks: a systematic review of clinical evidence. Med Sci Monit 21:432. https://doi.org/10.12659/MSM.891320
Majid A, Kheir F, Sierra-Ruiz M, Ghattas C, Parikh M, Channick C, Keyes C, Chee A, Fernandez-Bussy S, Gangadharan S, Folch E (2019) Assessment of fissure integrity in patients with intrabronchial valves for treatment of prolonged air leak. Ann Thorac Surg 107:407–411. https://doi.org/10.1016/j.athoracsur.2018.08.046
Belda-Sanchís J, Serra-Mitjans M, Iglesias Sentis M, Rami R (2010) Surgical sealant for preventing air leaks after pulmonary resections in patients with lung cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd003051.pub3
Moser C, Opitz I, Zhai W, Rousson V, Russi EW, Weder W, Lardinois D (2008) Autologous fibrin sealant reduces the incidence of prolonged air leak and duration of chest tube drainage after lung volume reduction surgery: a prospective randomized blinded study. J Thorac Cardiovasc Surg 136:843–849. https://doi.org/10.1016/J.JTCVS.2008.02.079
Shackcloth MJ, Poullis M, Jackson M, Soorae A, Page RD (2006) Intrapleural instillation of autologous blood in the treatment of prolonged air leak after lobectomy: a prospective randomized controlled trial. Ann Thorac Surg 82:1052–1056. https://doi.org/10.1016/J.ATHORACSUR.2006.04.015
Karampinis I, Galata C, Arani A, Grilli M, Hetjens S, Shackcloth M, Buderi S, Stamenovic D, Roessner ED (2021) Autologous blood pleurodesis for the treatment of postoperative air leaks. A systematic review and meta-analysis. Thorac Cancer 12:2648–2654. https://doi.org/10.1111/1759-7714.14138
Singhal S, Ferraris VA, Bridges CR, Clough ER, Mitchell JD, Fernando HC, Shrager JB (2010) Management of alveolar air leaks after pulmonary resection. Ann Thorac Surg 89:1327–1335. https://doi.org/10.1016/J.ATHORACSUR.2009.09.020
Caviezel C, Schneiter D, Opitz I, Weder W (2018) Lung volume reduction surgery beyond the NETT selection criteria. J Thorac Dis 10:S2748–S2753. https://doi.org/10.21037/JTD.2018.08.93
Funding
Open access funding provided by Royal Library, Copenhagen University Library. This study was supported with a research grant from Medtronic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Alberte Lund: Research grant received from Medtronic, Patrick Soldath: None, Erika Helena Nodin: None, Henrik Jessen Hansen: Speaker fee from BD and Medtronic. Kristine Jensen: Speakers honorary from PulmonX, Anna Kalhauge: None, Kåre Hornbech: None, Michael Perch: received speakers honorary from Astra-Zeneca, Chiesi, Novartis, PulmonX, Takeda and Therakos. Institutional research grant from Roche and PulmonX. Boeringer-Ingelheim supported congress participation. Jann Mortensen: None, René Horsleben Petersen: Research grant received from Medtronic. Speaker fee from Medtronic, AMBU, AstraZeneca, Medela. Advisory board for AstraZeneca, MSD, Roche, Bristol Myers Squibb.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The following abstract was presented at the 31st ESTS meeting in June 2023.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lund, A., Soldath, P., Nodin, E. et al. Predictors of reoperation after lung volume reduction surgery. Surg Endosc 38, 679–687 (2024). https://doi.org/10.1007/s00464-023-10559-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10559-z