Abstract
Background
Video-based assessment by experts may structurally measure surgical performance using procedure-specific competency assessment tools (CATs). A CAT for minimally invasive esophagectomy (MIE-CAT) was developed and validated previously. However, surgeon’s time is scarce and video assessment is time-consuming and labor intensive. This study investigated non-procedure-specific assessment of MIE video clips by MIE experts and crowdsourcing, collective surgical performance evaluation by anonymous and untrained laypeople, to assist procedure-specific expert review.
Methods
Two surgical performance scoring frameworks were used to assess eight MIE videos. First, global performance was assessed with the non-procedure-specific Global Operative Assessment of Laparoscopic Skills (GOALS) of 64 procedural phase-based video clips < 10 min. Each clip was assessed by two MIE experts and > 30 crowd workers. Second, the same experts assessed procedure-specific performance with the MIE-CAT of the corresponding full-length video. Reliability and convergent validity of GOALS for MIE were investigated using hypothesis testing with correlations (experience, blood loss, operative time, and MIE-CAT).
Results
Less than 75% of hypothesized correlations between GOALS scores and experience of the surgical team (r < 0.3), blood loss (r = − 0.82 to 0.02), operative time (r = − 0.42 to 0.07), and the MIE-CAT scores (r = − 0.04 to 0.76) were met for both crowd workers and experts. Interestingly, experts’ GOALS and MIE-CAT scores correlated strongly (r = 0.40 to 0.79), while crowd workers’ GOALS and experts’ MIE-CAT scores correlations were weak (r = − 0.04 to 0.49). Expert and crowd worker GOALS scores correlated poorly (ICC ≤ 0.42).
Conclusion
GOALS assessments by crowd workers lacked convergent validity and showed poor reliability. It is likely that MIE is technically too difficult to assess for laypeople. Convergent validity of GOALS assessments by experts could also not be established. GOALS might not be comprehensive enough to assess detailed MIE performance. However, expert’s GOALS and MIE-CAT scores strongly correlated indicating video clip (instead of full-length video) assessments could be useful to shorten assessment time.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Suboptimal surgical performance has been related to less favorable patient outcomes in complex minimally invasive surgical procedures [1,2,3,4,5]. Procedure-specific competency assessment tools (CATs) are an objective method to measure surgical performance with [2, 6, 7]. CATs are tools for structured (video-based) assessment used by experts to assess surgical performance and are currently viewed as the gold standard for measuring surgical performance for a given surgical procedure. A procedure-specific CAT for minimally invasive esophagectomy (MIE), the MIE-CAT, was developed and validated by our group previously [8]. However, an important limitation for using the MIE-CAT is that time of expert surgeons is scarce and video analysis is time-consuming and labor intensive, thereby limiting potential broad applicability [2].
A way to assist expert review for MIE might be using global performance assessment of video clips. Global performance assessment with Global Operative Assessment of Laparoscopic Skills (GOALS) [9] could provide an initial performance estimate, potentially followed by detailed feedback of the MIE-CAT if desired. In addition, using video clips instead of full-length videos might reduce assessment time without loss of relevant information, but could introduce bias [10]. Another way to assist expert review might be the use of crowdsourcing, in which large groups of anonymous and untrained workers evaluate surgical performance [11,12,13,14,15]. However, previous studies that investigated crowdsourcing for surgical performance video assessment have important limitations: (1) the outcomes of non-procedure-specific tools (e.g., GOALS or Global Evaluative Assessment of Robotic Skills (GEARS) [16]) were not compared to procedure-specific CATs; and (2) the studies were performed with videos of relatively simple tasks or procedures, often in dry-lab settings [15, 17,18,19,20,21,22]. Therefore, additional research is desired to explore both global performance assessment of video clips and crowdsourcing for video assessment of MIE.
There are two primary aims of this study: (1) to evaluate global performance assessment of MIE and (2) to evaluate the correlation between MIE experts and crowd workers assessments. We hypothesize that global performance assessment by both MIE experts and crowd workers can reliably be used to assist expert review, by providing rapid global feedback for MIE surgeons and reduce assessment time significantly.
Materials and methods
Two frameworks for scoring surgical performance of MIE were used in this study: (1) global performance assessment (GOALS) and (2) procedure-specific performance (MIE-CAT) (Fig. 1). GOALS was assessed by both crowd workers and MIE experts, while the MIE-CAT was only assessed by MIE experts. The use of the MIE-CAT for crowd workers was considered unfeasible given the technical complexity of the MIE-CAT. Reliability and convergent validity of the surgical performance assessments were analyzed as constructed by the COSMIN panel [23]. This study was carried out in accordance with applicable legislation and reviewed by the ethical committee of the Radboud university medical center.
Video database and pre-processing
Full-length intraoperative MIE videos, performed thoraco-laparoscopically between 2011 and 2020, from the database of the Esophageal Center East Netherlands in Nijmegen were used. Eight transthoracic MIE with intrathoracic anastomosis videos for esophageal cancer were randomly included. Each included procedure was performed by two consultant surgeons from one surgical team with four consultant surgeons in total. Procedures assisted by surgeons in training were excluded. Videos were divided into four experience groups, based on the consecutive case date and the learning curve of 119 cases found by van Workum et al. [24]. These four groups include (1) novice (0 to 25 MIEs performed), (2) intermediate (26 to 119 MIEs performed), (3) advanced (120 to 200 MIEs performed), and (4) expert (> 200 MIEs performed) (Online Appendix A). Two randomly selected videos per experience group were included after written informed patient consent and were stripped from any patient or surgeon identifiers.
Video clips of maximum 10 min were used for the global performance assessment with GOALS. Every video was cut into eight video clips, with every clip representative to one of the eight phases of the MIE-CAT [8] (Table 1) based on procedural-phase landmarks (Online Appendix A), resulting in 64 video clips total. The eight full-length MIE videos (average 3.5 h per video) were used for the procedure-specific assessments with the MIE-CAT.
Reviewers
Crowd workers were recruited by Crowd-Sourced Assessment of Technical Skills® (C-SATS, Seattle, WA, USA) via Amazon Mechanical Turk (MTurk, https://mturk.com), an online marketplace that facilitates hiring crowd workers [25]. Crowd workers were eligible if they were 18 years or older, had more than 95% approval on previous evaluations and lived in the USA. All crowd workers received a training video prior to the assessment, including a skill comparison test with dry-lab videos of a high- and low-performing surgeon. Crowd workers were invited on a ‘first come, first served’ basis.
MIE experts, identified through a literature search in the field of MIE and previous research collaborations [8, 26,27,28], were contacted to participate in this study. In total, 9 MIE experts who performed at least 120 MIEs [24] and currently perform at least 50 MIEs annually from Europe (6), the USA (2), and Asia (1) were included. The average experience in esophageal surgery was 18 years (SD 8.3). All experts were trained in online video assessment using the MIE-CAT [8] during interactive online workshops of 1.5 h with two to five experts.
Performance assessment tools
All video assessments were conducted via the online C-SATS platform. First, global performance assessment was conducted by both crowd workers and experts with the non-procedure-specific validated GOALS tool [9] of the 64 video clips. Intraoperative laparoscopic performance of every video clip was assessed using four domains: (1) depth perception, (2) bimanual dexterity, (3) efficiency, and (4) tissue handling. GOALS’ autonomy domain was excluded because of the absence of sound. Each domain was scored with a 1–5 Likert scale. One GOALS assessment included all eight procedural phase-based video clips from one MIE procedure. To obtain a 95% confidence interval to be ± 1 point on the grading scale, at least 30 crowd workers per video clip assessment were deemed necessary based on previous research [17, 18, 29, 30]. In addition, two MIE experts were randomly appointed per GOALS assessment. An average GOALS score for each surgical phase video clip and for the full-length videos were analyzed. The average GOALS score was calculated as mean of all crowd workers or expert assessments.
Second, procedure-specific performance assessment of the eight corresponding full-length MIE videos were assessed with the MIE-CAT by the same two MIE experts. Performance was assessed using the eight procedural phases of the MIE-CAT (Table 1) [8]. Each procedural phase was scored with four quality components (exposure, execution, adverse events, and end-product quality) on a 1–4 Likert scale [8]. Crowd workers were excluded from procedure-specific assessments, since these assessments require procedure-specific expertise. Procedure-specific assessments resulted in one average MIE-CAT score per phase and per full-length video.
Global performance assessment of MIE
Convergent validity verifies whether the GOALS scores of MIE performance correlates with similar constructs to the degree that one would expect via hypotheses testing [31, 32]. If at least 75% of the hypotheses are correct, convergent validity is considered to be sufficient for GOALS assessment of MIE performance [31]. GOALS components scores that were investigated included the domain scores (4), phase scores (1), and total GOALS score (1) per video. For hypothesis testing the following related construct correlations with GOALS (components) were studied using Pearson’s correlations coefficients:
-
1.
Experience: Correlations between the GOALS (components) scores and experience of the surgical team, defined by consecutive case date. With the six GOALS components in total six hypotheses were tested for each group (crowd workers and experts separately).
-
2.
Clinical parameters: Correlations between the GOALS (components) scores and two clinical parameters: blood loss (in milliliters) and operative time (in minutes). With the six GOALS components in total 12 hypotheses (6 × 2 hypotheses) were tested for each group (crowd workers and experts separately).
-
3.
Procedure-specific performance: Correlations between the GOALS (components) scores, assessed by crowd workers and experts, and the MIE-CAT (components) scores assessed by experts. Components scores were investigated in relation each other: GOALS domain versus MIE-CAT quality component (4), GOALS phase versus MIE-CAT phase (1), and total GOALS versus total MIE-CAT (1). Therefore, in total six hypotheses were tested for each group (crowd workers and experts separately).
First, positive correlations between 0.3 and 0.7 (‘moderate’) were considered acceptable for the hypothesized correlations between GOALS and experience [32]. Second, negative correlations between − 0.3 and − 0.7 (‘moderate’) were considered acceptable for the hypothesized correlations between GOALS and the two clinical parameters. Both the experience of the surgical team and the two clinical parameters were expected to be indicators for global performance of MIE, and this was also confirmed in our previous study for procedure-specific performance for MIE [8]. In addition, Vassiliou et al. [9] showed increased GOALS score with increased experience for laparoscopic cholecystectomy. Smaller correlations than (−)0.3 would indicate inadequate global performance assessment and a higher correlation than (−)0.7 would indicate GOALS only correlates with experience or clinical outcome, while it is expected that global surgical performance embodies both. Third, a strong but not perfect positive correlation between 0.5 and 0.8 between global performance assessment (GOALS) and procedure-specific performance assessment (MIE-CAT) was considered acceptable. Both scoring frameworks are expected to assess surgical performance of MIE and therefore correlate at least moderately, > 0.5. However, the GOALS scores were not expected to correlate more than strong, > 0.8. The MIE-CAT assesses more detailed performance and thus the two tools assess the construct of quality performance in different ways. See Online Appendix B for an overview of the hypotheses for convergent validity. Reliability and validity of the MIE-CAT were established in a previous study [8].
Correlation MIE experts and crowd workers
The average GOALS scores of both experts and the average GOALS scores of all crowd workers from the corresponding video clip were used to determine inter-rater reliability. This inter-rater reliability was calculated using a one-way intraclass correlation coefficient (ICC) with a mean rating and consistency agreement. An ICC above 0.7 was considered acceptable and ≥ 0.8 good. In addition, a rank order of the lowest to highest scoring video (clip) and Bland–Altman plot was made to display the inter-rater agreement. The data analysis was performed using IBM SPSS Statistics for Windows version 27.0 (IBM Corp., Orchard Road Armonk, New York, US).
Results
MIE videos
Patients from the eight randomly included videos had a median age of 68.5 years (IQR 55.5–70.5) and BMI of 25.6 (IQR 21.3–29.2). A detailed overview can be found in Online Appendix C.
Assessments
The nine experts conducted a total of 16 full-length video assessments (containing ~ 51 video hours) with the MIE-CAT and 128 video clip assessments (containing ~ 21 video hours) with GOALS in 3.5 months. Crowd workers assessed a total of 1984 video clips (containing over 330 video hours) with GOALS in less than 2 days. Overall, the experts and crowd workers showed comparable mean GOALS scores (Table 2). Interestingly, the GOALS video clips scores from experts had a wider range than those of crowd workers (7.50–19.50 versus 12.84–15.63). See Online Appendix D for an overview of the correlating MIE-CAT scores.
Global performance assessment of MIE
Less than 75% of the correlations between GOALS component scores and the related constructs experience (Table 3), clinical parameters (Table 3), and MIE-CAT components (Table 4) were in agreement with our hypotheses for both the crowd and experts GOALS scores. For crowd workers, 14% of the correlations (5 of 36 hypotheses) and for experts, 56% of the correlations (20 of 36 hypotheses) were in agreement with our hypotheses.
There was a poor correlation (r < 0.3) between the GOALS scores and experience of the surgical team for either group (Table 3, Fig. 2a). None of these correlations (0/12) fell within the hypothesized values of 0.3 < r < 0.7. Between the GOALS scores and the two clinical parameters (blood loss & operative time), some correlations did fall within the hypothesized values (Table 3, Fig. 2b and c). For crowd workers, 5/12 correlations (blood loss versus ‘bimanual dexterity,’ ‘efficiency,’ ‘phase,’ and ‘total’ GOALS scores and ‘efficiency’ versus operative time) and for experts 4/12 correlations (blood loss versus ‘bimanual dexterity’/‘tissue handling’ and operative time versus ‘bimanual dexterity’/’efficiency’) were between -0.3 and -0.7, as hypothesized. The correlations between blood loss and ‘bimanual dexterity,’ and the correlation between operative time and ‘efficiency’, were within hypothesized values for both groups. Correlations between the expert GOALS scores and blood loss outside the hypothesized values were all stronger than expected (r > − 0.8).
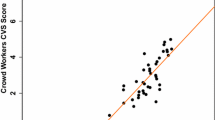
Almost all correlations (16/18) between the experts’ GOALS scores and the MIE-CAT scores were between the hypothesized values of 0.5 and 0.8 (Table 4). The two correlations that correlated less strongly than expected (< 0.5) were between GOALS domain ‘efficiency’ and MIE-CAT quality component ‘end-product quality’ (r = 0.40, 95% CI [− 0.42, 0.86]) and between GOALS ‘phase’ and MIE-CAT ‘phase’ scores (r = 0.45, 95% CI [0.23, 0.63]). None of the correlations between crowd workers’ GOALS scores and the MIE-CAT were above 0.5 (Table 4). Figure 2d visualizes the strong correlation between the experts’ total GOALS scores and the expert’ total MIE-CAT scores (r = 0.76, 95% CI [0.12, 0.95]) versus the minimal correlation between the crowd workers’ GOALS and expert MIE-CAT scores (r = 0.19, 95% CI [− 0.59, 0.79]).
Correlation MIE experts and crowd workers
A poor (ICC < 0.5) level of agreement on domain, video clip, and total GOALS scores was found between the experts and crowd workers (Table 2). All ICC values were below the acceptable 0.7, indicating insufficient agreement. In addition, a proportional bias can be seen (Online Appendix E): experts more frequently scored substantially lower or higher than average, while crowd workers scored the same video clip as ‘average.’ Additionally, only the lowest scoring video was agreed upon by both groups, when ranking the videos based on their total GOALS score (Online Appendix E).
Discussion
In this study, crowd workers and MIE experts scored 64 video clips of MIE using GOALS, which were compared to each other and to eight full-length video assessments using the MIE-CAT. The first aim was to evaluate global performance assessment with GOALS for MIE using convergent validity. We were unable to establish convergent validity for GOALS, whether scored by crowd workers or experts. However, GOALS scored by experts (but not crowd workers) strongly correlated with the experts’ MIE-CAT scores. This suggests video clip assessment by experts using GOALS could be useful to shorten assessment time when in-depth video analysis using the MIE-CAT is not required. The second aim was to evaluate the correlation between MIE experts and crowd workers assessments. A poor correlation between the crowd workers and experts’ GOALS scores was observed, despite promising results in previous studies and rapid results from crowd workers.
This study found a poor correlation between GOALS scores of crowd workers and experts, in contrast to earlier findings [13,14,15]. Previous studies, with a comparable sample size of crowd workers, found that dry-lab or relatively simple laparoscopic task video assessments show moderate to good agreement between crowd workers and experts [15, 17,18,19,20,21], while low agreement is seen in more complex laparoscopic global performance assessment videos [30]. Crowd workers might be used for relative simple procedures, whereas findings of the current study suggest performance assessment of real life surgeries, especially complex procedures, such as MIE, might technically be too difficult for laypeople to assess [18].
Although we were unable to establish convergent validity for GOALS, whether scored by crowds or experts, GOALS scored by experts (but not crowd workers) strongly correlated with the experts’ MIE-CAT scores [8]. In our view, GOALS is not comprehensive enough to fully capture the quality of a specific complex surgery, such as MIE. This could explain the poor correlation with experience, leading to loss of convergent validity. Moreover, GOALS cannot provide procedure-specific feedback that CATs do [2, 3, 6, 33] and may therefore not be useful for in-depth performance assessment. However, the fact that expert GOALS scores showed a strong correlation with expert MIE-CAT scores, suggest that expert GOALS scores may be used in situations where quicker screening of operative skills is required. If expert GOALS scores deviate from desired scores, this screening may be followed by in-depth review using the MIE-CAT, enabling the benefits of the MIE-CAT for detailed feedback, training, and quality improvement. Such a strategy might be a more efficient way to use the current tools that are available.
This study had several limitations. First, the crowd workers’ training included a skill comparison test with dry-lab videos. Ideally, this training would be more extensive [30] and should have included low- and high-performance surgical MIE videos. Unfortunately, in the beginning of this study these examples did not exist and therefore were not available. Regardless, we question how relatively short instructions can be used to effectively score complex surgical videos. Second, the most representative content for video clip performance assessment for MIE remains unclear. Current video clips were selected by the study team based on procedural-phase landmarks (e.g., introducing the stapler for the creation of the gastric tube) to provide comparable video clips. Successfully, a strong correlation between the assessed video clips with GOALS and full-length surgical videos with the MIE-CAT was observed. We expect performance in video clips will be representative to performance in full-length videos, even when components such as a large bleeding are absent. Nonetheless, future research is desired to determine the optimal video clip content and length, so video clips are representative for the complete procedure. Third, with the current study design we could not determine the individual influence of GOALS and video clips on the validity of global performance assessment of MIE by experts. Additional research would be recommended to investigate this for future use.
Once again video assessment has proven to be very labor intensive. Until performance assessments can be automated with artificial intelligence [11], further research could explore the reliability and validity of (para)medical workers, e.g., OR assistants or surgeons in training, for surgical performance assessment of complex laparoscopic procedures. [34] In addition, video clip assessment with GOALS seems to provide a fair reflection of global performance assessment of MIE if executed by experts and could be investigated to advance MIE video assessments. Experts’ GOALS assessments could be implemented in large-scale global performance video clip assessment as a screening or research tool for global performance levels, e.g., nationwide screening for performance of a specific procedural step, such as the creation of the anastomosis. Moreover, combining global performance assessment for initial screening with procedure-specific assessment for specific feedback and research questions could help optimizing essential MIE-CAT steps and minimize assessment time. Subsequently, shorter assessment time would enhance applicability of the MIE-CAT in daily clinical use. At the same time, a valuable database for computer-assisted video assessments containing global and procedure-specific performance assessments would be collected.
Conclusion
This study showed that global performance assessment of MIE by crowd workers is not useful for assisting expert assessments. MIE might be technically too difficult to assess for laypeople. GOALS, if used by experts, could be considered for large-scale global MIE performance video clip assessments and could be useful to shorten assessment time. However, as GOALS is not comprehensive enough to assess MIE performance in detail, the MIE-CAT can be used for an extensive procedure-specific performance analysis.
References
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJ (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Curtis NJ, Foster JD, Miskovic D, Brown CS, Hewett PJ, Abbott S, Hanna GB, Stevenson AR, Francis NK (2020) Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg. https://doi.org/10.1001/jamasurg.2020.1004
Stulberg JJ, Huang R, Kreutzer L, Ban K, Champagne BJ, Steele SR, Johnson JK, Holl JL, Greenberg CC, Bilimoria KY (2020) Association between surgeon technical skills and patient outcomes. JAMA Surg 155:960–968
Chhabra KR, Thumma JR, Varban OA, Dimick JB (2020) Associations between video evaluations of surgical technique and outcomes of laparoscopic sleeve gastrectomy. JAMA Surg 156:e205532
Balvardi S, Kammili A, Hanson M, Mueller C, Vassiliou M, Lee L, Schwartzman K, Fiore JF, Feldman LS (2022) The association between video-based assessment of intraoperative technical performance and patient outcomes: a systematic review. Surg Endosc 36:7938–7948
Zevin B, Bonrath EM, Aggarwal R, Dedy NJ, Ahmed N, Grantcharov TP (2013) Development, feasibility, validity, and reliability of a scale for objective assessment of operative performance in laparoscopic gastric bypass surgery. J Am Coll Surg 216:955–965 e958
Miskovic D, Ni M, Wyles SM, Kennedy RH, Francis NK, Parvaiz A, Cunningham C, Rockall TA, Gudgeon AM, Coleman MG (2013) Is competency assessment at the specialist level achievable? A study for the national training programme in laparoscopic colorectal surgery in England. Ann Surg 257:476–482
Ketel M, Eddahchouri Y, Klarenbeek B, MIE-CAT Collaboration Group, Hannink G, Rosman C, van Workum F (2023) Competency assessment tool for Minimally Invasive Esophagectomy: development, construct validity, reliability and version 2. Eur J Surg Oncol 49:E59
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondré K, Stanbridge D, Fried GM (2005) A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 190:107–113
McQueen S, McKinnon V, VanderBeek L, McCarthy C, Sonnadara R (2019) Video-based assessment in surgical education: a scoping review. J Surg Educ 76:1645–1654
Wang C, Han L, Stein G, Day S, Bien-Gund C, Mathews A, Ong JJ, Zhao P-Z, Wei S-F, Walker J (2020) Crowdsourcing in health and medical research: a systematic review. Infect Dis Poverty 9:1–9
Tucker JD, Day S, Tang W, Bayus B (2019) Crowdsourcing in medical research: concepts and applications. PeerJ 7:e6762
Katz AJ (2016) The role of crowdsourcing in assessing surgical skills. Surg Laparosc Endosc Percutaneous Tech 26:271–277
Aghdasi N, Bly R, White LW, Hannaford B, Moe K, Lendvay TS (2015) Crowd-sourced assessment of surgical skills in cricothyrotomy procedure. J Surg Res 196:302–306
Oh PJ, Chen J, Hatcher D, Djaladat H, Hung AJ (2018) Crowdsourced versus expert evaluations of the vesico-urethral anastomosis in the robotic radical prostatectomy: is one superior at discriminating differences in automated performance metrics? J Robot Surg 12:705–711
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ (2012) Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol 187:247–252
Chen C, White L, Kowalewski T, Aggarwal R, Lintott C, Comstock B, Kuksenok K, Aragon C, Holst D, Lendvay T (2014) Crowd-sourced assessment of technical skills: a novel method to evaluate surgical performance. J Surg Res 187:65–71
White LW, Kowalewski TM, Dockter RL, Comstock B, Hannaford B, Lendvay TS (2015) Crowd-sourced assessment of technical skill: a valid method for discriminating basic robotic surgery skills. J Endourol 29:1295–1301
Holst D, Kowalewski TM, White LW, Brand TC, Harper JD, Sorensen MD, Truong M, Simpson K, Tanaka A, Smith R (2015) Crowd-sourced assessment of technical skills: differentiating animate surgical skill through the wisdom of crowds. J Endourol 29:1183–1188
Ghani KR, Miller DC, Linsell S, Brachulis A, Lane B, Sarle R, Dalela D, Menon M, Comstock B, Lendvay TS (2016) Measuring to improve: peer and crowd-sourced assessments of technical skill with robot-assisted radical prostatectomy. Eur Urol 69:547–550
Powers MK, Boonjindasup A, Pinsky M, Dorsey P, Maddox M, Su L-M, Gettman M, Sundaram CP, Castle EP, Lee JY (2016) Crowdsourcing assessment of surgeon dissection of renal artery and vein during robotic partial nephrectomy: a novel approach for quantitative assessment of surgical performance. J Endourol 30:447–452
Deal SB, Stefanidis D, Telem D, Fanelli RD, McDonald M, Ujiki M, Brunt LM, Alseidi AA (2017) Evaluation of crowd-sourced assessment of the critical view of safety in laparoscopic cholecystectomy. Surg Endosc 31:5094–5100
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC (2010) The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 63:737–745
van Workum F, Stenstra MH, Berkelmans GH, Slaman AE, van Berge Henegouwen MI, Gisbertz SS, van den Wildenberg FJ, Polat F, Irino T, Nilsson M (2019) Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg 269:88–94
Keller DS, Winslow ER, Goldberg JE, Ahuja V (2021) Video-based coaching: current status and role in surgical practice (Part 1) from the society for surgery of the alimentary tract, health care quality and outcomes committee. J Gastrointest Surg 25:2439–2446
Eddahchouri Y, van Workum F, van den Wildenberg FJ, van Berge Henegouwen MI, Polat F, van Goor H, Pierie J-PE, Klarenbeek BR, Gisbertz SS, Rosman C (2021) European consensus on essential steps of Minimally Invasive Ivor Lewis and McKeown Esophagectomy through Delphi methodology. Surg Endosc 36:446–460
van Workum F, Verstegen MH, Klarenbeek BR, Bouwense SA, van Berge Henegouwen MI, Daams F, Gisbertz SS, Hannink G, Haveman JW, Heisterkamp J (2021) Intrathoracic vs cervical anastomosis after totally or hybrid minimally invasive esophagectomy for esophageal cancer: a randomized clinical trial. JAMA Surg. https://doi.org/10.1001/jamasurg.2021.1555
Ubels S, Lubbers M, Verstegen MH, Bouwense SA, van Daele E, Ferri L, Gisbertz SS, Griffiths EA, Grimminger P, Hanna G (2022) Treatment of anastomotic leak after esophagectomy: insights of an international case vignette survey and expert discussions. Dis Esophagus. https://doi.org/10.1093/dote/doac020
Kelly JD, Petersen A, Lendvay TS, Kowalewski TM (2020) The effect of video playback speed on surgeon technical skill perception. Int J Comput Assist Radiol Surg 15:739–747
Deal SB, Scully RE, Wnuk G, George BC, Alseidi AA (2020) Crowd-sourced and attending assessment of general surgery resident operative performance using global ratings scales. J Surg Educ 77:e214–e219
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60:34–42
De Vet HC, Terwee CB, Mokkink LB, Knol DL (2011) Measurement in medicine: a practical guide. Cambridge University Press, Cambridge
Tsai AY, Mavroveli S, Miskovic D, van Oostendorp S, Adamina M, Hompes R, Aigner F, Spinelli A, Warusavitarne J, Knol J (2019) Surgical quality assurance in COLOR III: standardization and competency assessment in a randomized controlled trial. Ann Surg 270:768–774
Dai JC, Lendvay TS, Sorensen MD (2017) Crowdsourcing in surgical skills acquisition: a developing technology in surgical education. J Grad Med Educ 9:697–705
Acknowledgements
We thank all the people involved in the GOALS and MIE-CAT video assessments for their contribution to this study, especially for the participating MIE experts in the MIE-GOALS Collaboration Group for their valuable time and effort. We also acknowledge the help of Mary Lynn Gaddis, Henry Choi, and Michiel Schumacher for providing access to the online C-CATS platform, incorporating our tool and finding crowd workers. Crowd workers were compensated for their contribution.
Funding
This study was funded via the investigator-initiated study proposal rewarded by Ethicon Endo-Surgery by Johnson & Johnson Medical Limited. The study was performed independently, and Ethicon had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit to manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mirte Ketel, Bastiaan Klarenbeek, Camiel Rosman, Yassin Eddahchouri, and Frans van Workum declare funding from Ethicon for the submitted work. However, Ethicon as sponsor had no role in the design and conduct of the study: collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Both Camiel Rosman and Bastiaan Klarenbeek report grants from Medtronic and Bastiaan Klarenbeek reports grants from ZonMW, Stichting Bergh in het Zadel, BeNeFit, Stichting Sasha Swartouw, and Radboud Oncology Fund outside of the submitted work. In addition, C-SATS donated the use of their product for the completion of this study. Elke van Daele reports a study grant ‘Kom op tegen kanker’ outside of the submitted work. Christian Gutschow received speaker honoraria: BD/Bard Medical, Johnson & Johnson, B. Braun/Aesculap, Micro-Tech Europe GmbH, and Bristol-Myers Squibb; Consulting fees: BD/Bard Medical and Medtronic; and Research grant: B. Braun/Aesculap, all outside of the submitted work. Misha Luyer received consulting fees from Medtronic and Galvani, outside of the submitted work. Robert Merritt received consulting fees from Astra Zeneca as advisory board and Honoria from Intuitive Surgical for lectures, all outside of the submitted work. Grard Nieuwenhuijzen received consulting fees from Medtronic, outside of the submitted work. Inger Abma, Miguel Cuesta, Michal Hubka, Arnulf Hölscher, and Yaxing Shen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ketel, M.H.M., Klarenbeek, B.R., Eddahchouri, Y. et al. Crowd-sourced and expert video assessment in minimally invasive esophagectomy. Surg Endosc 37, 7819–7828 (2023). https://doi.org/10.1007/s00464-023-10297-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10297-2