Abstract
Background
Total thoracoscopic segmentectomy (TTS) is a technically challenging procedure in children but results in more parenchyma preservation, better pain control, better cosmetic results, and a shorter hospital stay. However, definitive data describing the learning curve of TTS has yet to be obtained. Here, we review the safety and efficiency of our initial experiences with pediatric TTS and evaluate our learning curve.
Methods
This was a retrospective study of all pediatric patients undergoing TTS between December 2016 and January 2020. Pediatric patients who underwent TTS were included, while those undergoing lobectomy or wedge resection were excluded.
Results
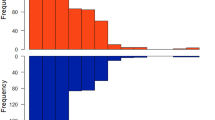
One hundred and twelve patients were retrospectively analyzed to evaluate the learning curve and were divided chronologically into three phases, the ascending phase (A), plateau phase (B) and descending phase (C), through cumulative summation (CUSUM) of the operative time (OT). Phases A, B, and C comprised 28, 51, and 33 cases, respectively. OT decreased significantly from phases A to B (p < 0.001) and from phase B to C (p = 0.076). No significant differences were observed in the demographic factors among the three phases. The conversion rate was zero, and the complication rate was 0.9%. Differences in technical parameters, such as length of stay and chest tube duration, were statistically insignificant between phases A and B or B and C. There were no mortalities.
Conclusion
CUSUMOT indicates that the learning curve of at least 79 cases is required for TTS in our institute. We emphasize that the learning curve should be cautiously interpreted because many factors in different institutions may influence the exact parabola and actual learning curve.
Graphical abstract



Similar content being viewed by others
Abbreviations
- TTS:
-
Total thoracoscopic segmentectomy
- CLM:
-
Congenital lung malformation
- CPAM:
-
Congenital pulmonary airway malformation
- iBPS:
-
Intralobar bronchopulmonary sequestration
- CUSUM:
-
Cumulative summation
References
Rothenberg SS (2000) Thoracoscopic lung resection in children. J Pediatr Surg 35:271–274
Rothenberg SS, Kuenzler KA, Middlesworth W, Kay S, Yoder S, Shipman K, Rodriguez R, Stolar CJ (2011) Thoracoscopic lobectomy in infants less than 10 kg with prenatally diagnosed cystic lung disease. J Laparoendosc Adv Surg Tech A 21(2):181–184
He T, Sun X, Yang Y, Yuan M, Yang G, Cheng K, Chang Xu (2022) Learning curve for total thoracoscopic lobectomy for treating pediatric patients with congenital lung malformation. Asian J Surg 45(7):1383–1388. https://doi.org/10.1016/j.asjsur.2021.08.061. (Epub 2021 Oct 8)
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25(3):855–860
Wang X, Guo H, Quanteng H, Ying Y, Chen B (2021) Pulmonary function after segmentectomy versus lobectomy in patients with early-stage non-small-cell lung cancer: a meta-analysis. J Int Med Res. 49(9):03000605211044204. https://doi.org/10.1177/03000605211044204
Laros CD, Westermann CJJ (1987) Dilatation, compensatory growth, or both after pneumonectomy during childhood and adolescence: a thirty-year follow-up study. J Thorac Cardiovasc Surg 93:570–576
Thurlbeck WM (1983) Postpneumonectomy compensatory lung growth. Am Rev Respir Dis 128:965–967
Brody JS (1975) Time course of and stimuli to compensatory growth of the lung after pneumonectomy. J Clin Investig 56(4):897–904. https://doi.org/10.1172/JCI108169
Rannels DE, Burkhart LR, Watkins CA (1984) Effect of age on the accumulation of lung protein following unilateral pneumonectomy in rats. Growth 48:297–308
Huang J-X, Hong S-M, Hong J-J, Chen Q, Cao H (2021) Medium-term pulmonary function test after thoracoscopic lobectomy and segmentectomy for congenital lung malformation: a comparative study with normal control. Front Pediatr. 9:755328. https://doi.org/10.3389/fped.2021.755328
Laje P, Pearson EG, Simpao AF, Rehman MA, Sinclair T, Hedrick HL, Adzick NS, Flake AW (2015) The first 100 infant thoracoscopic lobectomies: observations through the learning curve and comparison to open lobectomy. J Pediatr Surg 50:1811–1816
Diamond IR, Herrera P, Langer JC, Kim PC (2007) Thoracoscopic versus open resection of congenital lung lesions: a case matched study. J Pediatr Surg 42:1057–1061
Vu LT, Farmer DL, Nobuhara KK, Miniati D, Lee H (2008) Thoracoscopic versus open resection for congenital cystic adenomatoid malformations of the lung. J Pediatr Surg 43:35–39
Park S, Kim ER, Hwang Y, Lee HJ, Park IK, Kim YT, Kang CH (2017) Serial improvement of quality metrics in pediatric thoracoscopic lobectomy for congenital lung malformation: an analysis of learning curve. Surg Endosc 31(10):3932–3938
Carrott PW Jr, Jones DR (2013) Teaching video-assisted thoracoscopic (VATS) lobectomy. J Thorac Dis 5(Suppl 3):S207–S211
Tsubota N, Ayabe K, Doi O, Mori T, Namikawa S, Taki T, Watanabe Y (1998) Ongoing prospective study of segmentectomy for small lung tumors: study group of extended segmentectomy for small lung tumor. Ann Thorac Surg 66(5):1787–1790. https://doi.org/10.1016/s0003-4975(98)00819-4
Misaki N, Chang SS, Gotoh M, Yamamoto Y, Satoh K, Yokomise HJ (2009) a novel method for determining adjacent lung segments with infrared thoracoscopy. Thorac Cardiovasc Surg 138(3):613–618. https://doi.org/10.1016/j.jtcvs.2009.01.003. (Epub 2009 Mar 9)
Matsuoka H, Nishio W, Sakamoto T, Harada H, Yoshimura M, Tsubota N (2003) selective segmental jet injection to distinguish the intersegmental plane using jet ventilation. Jpn J Thorac Cardiovasc Surg 51(8):400–401. https://doi.org/10.1007/BF02719478
Sato M, Murayama T, Nakajima J (2016) Techniques of stapler based navigational thoracoscopic segmentectomy using virtual assisted lung mapping (VAL-MAP). J Thorac Dis 8:S716–S730
Wu WB, Xia Y, Pan XL, Wang J, He ZC, Xu J, Wen W, Xu XF, Zhu Q, Chen L (2019) Three-dimensional navigation-guided thoracoscopic combined subsegmentectomy for intersegmental pulmonary nodules. Thorac Cancer 10:41–46
Lau CT, Au DM, Wong KKY (2019) Application of indocyanine green in pediatric surgery. Pediatr Surg Int 35(10):1035–1041. https://doi.org/10.1007/s00383-019-04502-4. (Epub 2019 Jun 26)
Acknowledgements
None.
Funding
This study is supported by the National Natural Science Foundation of China (NO. 31201095) to Chang Xu.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chang Xu was granted by the National Natural Science Foundation of China (NO.31201095). Drs. Taozhen He, Miao Yuan, Gang Yang, Kaisheng Cheng, MS. Xiaoyan Sun, and MS. Shiyi Dai have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, T., Sun, X., Liu, C. et al. Learning curve for total thoracoscopic segmentectomy in treating pediatric patients with congenital lung malformation. Surg Endosc 37, 5129–5136 (2023). https://doi.org/10.1007/s00464-023-09987-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09987-8