Abstract
Background
Unnecessary endoscopic retrograde cholangiopancreatography (ERCP) after spontaneous passage of common bile duct stones (CBDSs) should be avoided. This study aimed to examine the cumulative diagnosis rate and the predictive factors of spontaneous CBDS passage during the interval between the imaging diagnosis and ERCP.
Methods
This multicenter retrospective study included 1260 consecutive patients with native papilla diagnosed with CBDSs using imaging modalities. Predictive factors and cumulative diagnosis rate of spontaneously passed CBDSs during the interval between imaging diagnosis and ERCP were analyzed.
Results
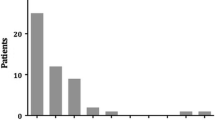
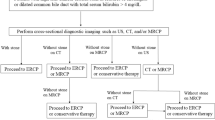
The overall cumulative diagnosis rate of spontaneous CBDS passage was 6.2% (78/1260) during a mean interval of 5.0 days. In the multivariate analysis, CBDS sized < 6 mm on diagnostic imaging, solitary CBDS on diagnostic imaging, intervals between the imaging diagnosis and ERCP, and nondilated common bile duct (< 10 mm) were the significant factors associated with spontaneous CBDS passage. Specifically, the cumulative diagnosis rate of spontaneous passage was significantly higher in patients with solitary and CBDSs sized < 6 mm than in those with other CBDSs (14.4% [54/376] vs. 2.7% [24/884], P < 0.001). In both the asymptomatic and symptomatic groups, the cumulative diagnosis rate of the spontaneous passage of CBDSs was significantly higher in patients with solitary and CBDSs sized < 6 mm on diagnostic imaging than in those with multiple and/or CBDSs sized ≥ 6 mm on diagnostic imaging during a mean interval of 20.5 and 2.4 days, respectively (asymptomatic group: 22.4% [15/67] vs. 3.5% [4/113], P < 0.001, symptomatic group: 12.6% [39/309] vs. 2.6% [20/771], P < 0.001).
Conclusions
Solitary and CBDSs sized < 6 mm on diagnostic imaging can often lead unnecessary ERCP due to spontaneous passage. Preliminary endoscopic ultrasonography immediately before ERCP is recommended, especially in patients with solitary and small CBDSs on diagnostic imaging.




Similar content being viewed by others
References
Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE (2019) Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 51:472–491
Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66:765–782
Tazuma S, Unno M, Igarashi Y, Inui K, Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, Ryozawa S, Nimura Y, Fujita N, Kubota K, Shoda J, Tabata M, Mine T, Sugano K, Watanabe M, Shimosegawa T (2017) Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol 52:276–300
Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB, ASGE Standards of Practice Committee (2019) ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 89:1075–1105
Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM, ASGE Standards of Practice Committee (2017) Adverse events associated with ERCP. Gastrointest Endosc 85:32–47
Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC (2004) A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg 239:28–33
Khan OA, Balaji S, Branagan G, Bennett DH, Davies N (2011) Randomized clinical trial of routine on-table cholangiography during laparoscopic cholecystectomy. Br J Surg 98:362–367
Hauer-Jensen M, Karesen R, Nygaard K, Solheim K, Amlie EJ, Havig O, Rosseland AR (1993) Prospective randomized study of routine intraoperative cholangiography during open cholecystectomy: long-term follow-up and multivariate analysis of predictors of choledocholithiasis. Surgery 113:318–323
Frossard JL, Hadengue A, Amouyal G, Choury A, Marty O, Giostra E, Sivignon F, Sosa L, Amouyal P (2000) Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc 51:175–179
Andreozzi P, de Nucci G, Devani M, Redaelli D, Schettino M, Iuliano D, Zulli C, Maurano A, Bottiglieri ME, Paspatis G, Dinelli M, Manes G (2022) The high rate of spontaneous migration of small size common bile duct stones may allow a significant reduction in unnecessary ERCP and related complications: results of a retrospective, multicenter study. Surg Endosc 36:3542–3548
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Park BK, Seo JH, Jeon HH, Choi JW, Won SY, Cho YS, Lee CK, Park H, Kim DW (2018) A nationwide population-based study of common bile duct stone recurrence after endoscopic stone removal in Korea. J Gastroenterol 53:670–678
Kawaji Y, Isayama H, Nakai Y, Saito K, Sato T, Hakuta R, Saito T, Takahara N, Mizuno S, Kogure H, Matsubara S, Tada M, Kitano M, Koike K (2019) Multiple recurrences after endoscopic removal of common bile duct stones: a retrospective analysis of 976 cases. J Gastroenterol Hepatol 34:1460–1466
Ryozawa S, Itoi T, Katanuma A, Okabe Y, Kato H, Horaguchi J, Fujita N, Yasuda K, Tsuyuguchi T, Fujimoto K (2018) Japan gastroenterological endoscopy Society guidelines for endoscopic sphincterotomy. Dig Endosc 30:149–173
Meeralam Y, Al-Shammari K, Yaghoobi M (2017) Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc 86:986–993
Giljaca V, Gurusamy KS, Takwoingi Y, Higgie D, Poropat G, Štimac D, Davidson BR (2015) Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD011549
Petrov MS, Savides TJ (2009) Systematic review of endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis. Br J Surg 96:967–974
Kim SB, Kim KH, Kim TN (2016) Comparison of outcomes and complications of endoscopic common bile duct stone removal between asymptomatic and symptomatic patients. Dig Dis Sci 61:1172–1177
Saito H, Koga T, Sakaguchi M, Kadono Y, Kamikawa K, Urata A, Imamura H, Tada S, Kakuma T, Matsushita I (2019) Post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with asymptomatic common bile duct stones. J Gastroenterol Hepatol 34:1153–1159
Xu XD, Qian JQ, Dai JJ, Sun ZX (2020) Endoscopic treatment for choledocholithiasis in asymptomatic patients. J Gastroenterol Hepatol 35:165–169
Xiao L, Geng C, Li X, Li Y, Wang C (2021) Comparable safety of ERCP in symptomatic and asymptomatic patients with common bile duct stones: a propensity-matched analysis. Scand J Gastroenterol 56:111–117
Kadokura M, Takenaka Y, Yoda H, Yasumura T, Okuwaki T, Tanaka K, Amemiya F (2021) Asymptomatic common bile duct stones are associated with increased risk of post-endoscopic retrograde cholangiopancreatography pancreatitis. JMA J 4:141–147
Saito H, Kadono Y, Shono T, Kamikawa K, Urata A, Nasu J, Imamura H, Matsushita I, Kakuma T, Tada S (2021) Endoscopic retrograde cholangiopancreatography-related complications for bile duct stones in asymptomatic and symptomatic patients. JGH Open 5:1382–1390
Buxbaum JL, Buitrago C, Lee A, Elmunzer BJ, Riaz A, Ceppa EP, Al-Haddad M, Amateau SK, Calderwood AH, Fishman DS, Fujii-Lau LL, Jamil LH, Jue TL, Kwon RS, Law JK, Lee JK, Naveed M, Pawa S, Sawhney MS, Schilperoort H, Storm AC, Thosani NC, Qumseya BJ, Wani S (2021) ASGE guideline on the management of cholangitis. Gastrointest Endosc 94:207–221
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN (2018) American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology 154:1096–1101
Buscarini E, Tansini P, Vallisa D, Zambelli A, Buscarini L (2003) EUS for suspected choledocholithiasis: do benefits outweigh costs? A prospective, controlled study. Gastrointest Endosc 57:510–518
Gurusamy KS, Giljaca V, Takwoingi Y, Higgie D, Poropat G, Štimac D, Davidson BR (2015) Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD011548
Anderson SW, Rho E, Soto JA (2008) Detection of biliary duct narrowing and choledocholithiasis: accuracy of portal venous phase multidetector CT. Radiology 247:418–427
Saito H, Iwagoi Y, Noda K, Atsuji S, Takaoka H, Kajihara H, Shono T, Nasu J, Obara H, Kakuma T, Tada S, Morishita S, Matsushita I, Katahira K (2021) Dual-layer spectral detector computed tomography versus magnetic resonance cholangiopancreatography for biliary stones. Eur J Gastroenterol Hepatol 33:32–39
Kim CW, Chang JH, Lim YS, Kim TH, Lee IS, Han SW (2013) Common bile duct stones on multidetector computed tomography: attenuation patterns and detectability. World J Gastroenterol 19:1788–1796
Acknowledgements
We would like to thank the staff involved in ERCP at the participating institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Hirokazu Saito, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Haruo Imamura, Ikuo Matsushita, Tatsuyuki Kakuma, and Shuji Tada have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saito, H., Iwasaki, H., Itoshima, H. et al. Unnecessary endoscopic retrograde cholangiopancreatography associated with the spontaneous passage of common bile duct stones into the duodenum: a multicenter retrospective study. Surg Endosc 37, 4585–4593 (2023). https://doi.org/10.1007/s00464-023-09954-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09954-3