Abstract
Background
We sought to identify the 10-year complication and recurrence rates and associated sociodemographic and operative characteristics associated with non-mesh versus mesh-based ventral hernia repairs (VHRs).
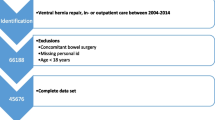
Methods
This was an IRB-approved (2020H0317) retrospective longitudinal study of patients undergoing mesh or non-mesh VHR from 2009–2019 at a single tertiary-care institution. The electronic medical record was used to collect sociodemographic, clinical, and intraoperative details, and early (≤ 30 days) and long-term (> 30-day) postoperative complications. Up to ten-year follow-up was obtained for long-term complications, categorized as: hernia recurrence reoperation (HRR), major complications requiring emergency surgery (MCES) (defined as non-elective operations related to the abdominal wall), and non-recurrence procedural intervention (NRPI) (defined as any procedures related to the abdominal wall, bowel, or mesh). Kaplan–Meier survival curves were obtained for each long-term complication.
Results
Of the 645 patients identified, the mean age at index operation was 52.51 ± 13.57 years with 50.70% female. Of the index operations, 21.24% were for a recurrence. Procedure categories included: 57.36% incisional, 37.21% non-incisional umbilical, 8.22% non-incisional epigastric, 3.88% parastomal, 0.93% diastasis recti, and 0.47% Spigelian hernias. Operative approaches included open (n = 383), laparoscopic (n = 267), and robotic (n = 21). Fascial closure (81.55%) and mesh use (66.2%) were performed in the majority of cases. Median follow-up time was 2098 days (interquartile range 1320–2806). The rate of short-term complications was 4.81% for surgical site infections, 15.04% for surgical site occurrences, and 13.64% for other complications. At 10 years, the HRR-free survival probability was 85.26%, MCES-free survival probability was 94.44%, and NRPI-free survival probability was 78.11%.
Conclusions
A high proportion of patients experienced long-term recurrence and complications requiring intervention after index VHR. For many patients, a ventral hernia develops into a chronic medical condition. Improved efforts at post-market surveillance of operative approaches and mesh location and type should be undertaken to help optimize outcomes.
Graphical abstract




Similar content being viewed by others
References
Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, Beck W, Holzman MD (2012) Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 16:179–183. https://doi.org/10.1007/s10029-011-0879-9
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J, (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398. https://doi.org/10.1056/NEJM200008103430603
Kroese LF, van Eeghem LHA, Verhelst J, Jeekel J, Kleinrensink G-J, Lange JF (2017) Long term results of open complex abdominal wall hernia repair with self-gripping mesh: A retrospective cohort study. Int J Surg 44:255–259. https://doi.org/10.1016/j.ijsu.2017.07.029
Leber GE (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378. https://doi.org/10.1001/archsurg.133.4.378
Burger JWA, Luijendijk RW, Hop WCJ, Halm JA, Verdaasdonk EGG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–585. https://doi.org/10.1097/01.sla.0000141193.08524.e7
Caro-Tarrago A, Olona C, Millán M, Olona M, Espina B, Jorba R (2019) Long-term results of a prospective randomized trial of midline laparotomy closure with onlay mesh. Hernia 23:335–340. https://doi.org/10.1007/s10029-019-01891-2
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316:1575. https://doi.org/10.1001/jama.2016.15217
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Deeken CR, Lake SP (2017) Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J Mech Behav Biomed Mater 74:411–427. https://doi.org/10.1016/j.jmbbm.2017.05.008
Haskins IN, Horne CM, Krpata DM, Prabhu AS, Tastaldi L, Perez AJ, Rosenblatt S, Poulose BK, Rosen MJ (2018) A call for standardization of wound events reporting following ventral hernia repair. Hernia 22:729–736. https://doi.org/10.1007/s10029-018-1748-6
Park AE, Roth JS, Kavic SM (2006) Abdominal wall hernia. Curr Probl Surg 43:326–375. https://doi.org/10.1067/j.cpsurg.2006.02.004
Shankar DA, Itani KMF, O’Brien WJ, Sanchez VM (2017) Factors associated with long-term outcomes of umbilical hernia repair. JAMA Surg 152:461–466. https://doi.org/10.1001/jamasurg.2016.5052
Huntington CR, Cox TC, Blair LJ, Schell S, Randolph D, Prasad T, Lincourt A, Heniford BT, Augenstein VA (2016) Biologic mesh in ventral hernia repair: outcomes, recurrence, and charge analysis. Surgery 160:1517–1527. https://doi.org/10.1016/j.surg.2016.07.008
Park H, de Virgilio C, Kim DY, Shover AL, Moazzez A (2021) Effects of smoking and different BMI cutoff points on surgical site infection after elective open ventral hernia repair. Hernia 25:337–343. https://doi.org/10.1007/s10029-020-02190-x
Jolissaint JS, Dieffenbach BV, Tsai TC, Pernar LI, Shoji BT, Ashley SW, Tavakkoli A (2020) Surgical site occurrences, not BMI, increase the long-term risk of ventral hernia recurrence. Surgery 167:765–771. https://doi.org/10.1016/j.surg.2020.01.001
Prabhu AS, Poulose BK, Rosen MJ (2020) Harnessing the power of collaboration for postmarket surveillance of hernia mesh devices. Ann Surg 271:221–222. https://doi.org/10.1097/SLA.0000000000003437
Huerta S, Varshney A, Patel PM, Mayo HG, Livingston EH (2016) Biological mesh implants for abdominal hernia repair: US food and drug administration approval process and systematic review of its efficacy. JAMA Surg 151:374–381. https://doi.org/10.1001/jamasurg.2015.5234
Segan RD (2010) A Response to “Major complications associated with xenograft biologic mesh implantation in abdominal wall reconstruction” (Harth KC, Rosen MJ. Surg Innov. 2009;16:324–329) and discussion of the MAUDE (Manufacturer and User Facility Device Experience) Database, FDA Regulation of Biologic Implants, and Evidence-Based Medicine. Surg Innov 17:273–275. https://doi.org/10.1177/1553350610371214
Veronin MA, Schumaker RP, Dixit R (2020) The irony of medwatch and the FAERS database: an assessment of data input errors and potential consequences. J Pharm Technol 36:164–167. https://doi.org/10.1177/8755122520928495
Funding
This research was supported by the National Institutes of Health under the Ruth L. Kirschstein National Research Service Award, from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number NIH T32AI106704. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Benjamin K. Poulose has the following disclosures: salary support from the ACHQC, research support from BD Interventional and Advanced Medical Solutions, consulting fees from Ethicon. Dr. Dahlia M. Kenawy, Dr. Jennifer M. Underhill, Dr. Ayanna G. Jacobs, Molly A. Olson, Savannah M. Renshaw, Benjamin T. Gabanic, Dr. Marlene I. Garcia-Neuer, Parviz Kanga, and Aysenur Gunacar have no financial conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This research was supported by the National Institutes of Health under the Ruth L. Kirschstein National Research Service Award, from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number NIH T32AI106704. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kenawy, D.M., Underhill, J.M., Jacobs, A.G. et al. Ten-year outcomes following ventral hernia repair: making the case for better post-market surveillance in the USA. Surg Endosc 37, 5612–5622 (2023). https://doi.org/10.1007/s00464-022-09725-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09725-6