Abstract
Background
Evidence on the added value of robotic-assistance in the abdominal phase during esophagectomy is scarce. In 2003, our center implemented the robotic thoracic phase for esophagectomy. In November 2018 the robot was also implemented in the abdominal phase. The aim of this study was to evaluate the implementation of the abdominal phase during robot-assisted minimally invasive esophagectomy (RAMIE).
Methods
Consecutive patients who underwent full RAMIE with intrathoracic anastomosis for esophageal cancer were included. Patients were extracted from a prospectively maintained institutional database. A cumulative sum (CUSUM) analysis was performed for abdominal operation time and abdominal lymph node yield. Intraoperative, postoperative and oncological outcomes including collected lymph nodes per abdominal lymph node station were reported.
Results
Between 2018 and 2021, 70 consecutive patients were included. The majority of the patients had an adenocarcinoma (n = 55, 77%) and underwent neoadjuvant chemo(radio)therapy (n = 65, 95%). The median operative time for the abdominal phase was 180 min (range 110–233). The CUSUM analysis for abdominal operation time showed a plateau at case 22. There were no intraoperative complications or conversions during the abdominal phase. The most common postoperative complications were pneumonia (n = 18, 26%) and anastomotic leakage (n = 14, 20%). Radical resection margins were achieved in 69 (99%) patients. The median total lymph node yield was 42 (range 23–83) and the median abdominal lymph node yield was 16 (range 2–43). The CUSUM analysis for abdominal lymph node yield showed a plateau at case 21. Most abdominal lymph nodes were collected from the left gastric artery (median 4, range 0–20).
Conclusions
This study shows that a robotic abdominal phase was safely implemented for RAMIE without compromising intraoperative, postoperative and oncological outcomes. The learning curve is estimated to be 22 cases in a high-volume center with experienced upper GI robotic surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Robot-assisted minimally invasive esophagectomy (RAMIE) was introduced in 2003 and allows for precise dissection by offering three-dimensional vision, motion scaling and articulating instruments [1]. Recently, the ROBOT trial demonstrated superiority of RAMIE over open esophagectomy [2]. Research on the added value of a robotic system during esophagectomy has mainly focused on the thoracic phase while the added value in the abdominal phase has rarely been reported [3]. In our center, the da Vinci® robotic system (Intuitive Surgical Inc, Sunnyvale, CA) was initially used for the thoracoscopic phase only, as the first Standard-SI systems were not suitable for the abdominal phase due to the need for re-docking during the multiquadrant surgery that is required for dissection of the duodenum, greater gastric curvature, and hiatus. In addition, there were no robotic endowristed sealing instruments available. The dissection of the greater curvature along the gastroepiploic vessels with a rigid robotic ultrasonic scalpel did not add to conventional laparoscopic dissection. With the newest generation robot (Xi®) and the recently introduced robotic bipolar coagulator (vessel sealer®), these limitations have been solved and the robotic abdominal phase could provide technical benefits. However, little has been published about the potential benefits of robotic versus conventional minimally invasive surgery during the abdominal phase of RAMIE. In addition, evidence on the learning curve for the abdominal phase during RAMIE is scarce and only few studies have published on this topic [4, 5]. As surgeons are increasingly willing to adopt full RAMIE as their preferential technique, knowledge about the learning curve for the abdominal phase of RAMIE is important for proctoring programs in order to safely implement the robotic system in the abdominal phase. Therefore, the aim of this study was to evaluate the implementation of the abdominal phase during RAMIE in a high-volume center with experienced upper GI robotic surgeons.
Materials and methods
RAMIE experience
Robot-assisted minimally invasive esophagectomy (RAMIE) was implemented in 2003 in the University Medical Center Utrecht [6]. A timeline for key milestones in the development of RAMIE is shown in Fig. 1. Initially, only McKeown procedures were performed with a robot-assisted thoracic phase combined with conventional laparoscopy during the abdominal phase, except for the first 13 cases which involved laparotomies. The learning curve for the robot-assisted thoracic phase was completed in 2008 as published previously [7]. A robot-assisted hand-sewn anastomosis was introduced in 2016. From than onwards, in general patients with distal esophageal cancer underwent Ivor-Lewis esophagectomy and patients with mid or upper esophageal cancer underwent McKeown esophagectomy. In November 2018, the robot was also implemented during the abdominal phase. From then on, all consecutive patients underwent full RAMIE. All RAMIE procedures were carried out by JR and RvH. From October 2020 onwards, which corresponds with case 43, a new surgeon was proctored during the abdominal phase of RAMIE.
Patient population
In this study, all consecutive patients who underwent full RAMIE with intrathoracic anastomosis for esophageal cancer between November 2018 and December 2021 were included. Patients were extracted from a prospectively maintained database. There were no exclusion criteria defined for this study. The institutional review board approved this study and the need for informed consent was waived.
Surgical procedure
RAMIE consisted of a two-field lymphadenectomy, gastric conduit reconstruction and intrathoracic hand-sewn anastomosis. The robot-assisted abdominal phase follows the same surgical steps as a laparoscopically performed phase [3]. The patient was placed in supine position after which 4 robotic ports were placed (3 × 8 mm and 1 × 12 mm) and a 5 mm incision subxiphiodal for the liver retractor and a 10 mm incision for the assistant port (Fig. 2). First, the lesser omentum was opened and dissection took place towards the crus with the Cautery Hook. Hereafter, the greater omentum was opened and the dissection was guided toward the short gastric vessels which were transected with the Vessel Sealer. The procedure continued with the dissection of the celiac trunk. The left gastric vein was transected with the vessel sealer and the left gastric artery with a hem-o-lock. The abdominal lymphadenectomy consisted of a dissection over the celiac trunk (Station 9), the splenic artery (Station 11) and the hepatic artery (station 8) (Fig. 3). The gastric conduit was created with an endowristed stapler device. From December 2018, a robotic stapler device was used. From January 2019, all patients routinely received a feeding jejunostomy which concluded the abdominal phase. In general, no fluorescence techniques were used in the abdominal phase. However, indocyanine green was routinely used in the thoracic phase to determine the location for the anastomosis at the gastric conduit [8]. From March 2019, all lymph nodes were collected separately in different containers according to the LOGICA study protocol [9]. The robot-assisted thoracic phase has been described in detail previously [10]. In summary, patients were placed in a semi-prone position after which 4 robotic arms were inserted and 1 assistant port. The esophagus was mobilized and a full mediastinal lymphadenectomy was performed. The gastric conduit was positioned in the esophageal bed. All patients had a hand-sewn robot-assisted intrathoracic anastomosis which was created with an end-to-side technique [11]. In general, all patients underwent cruroplasty with 2 independent sutures that concluded the thoracic phase.
Outcomes
The primary outcome was the learning curve for the duration of the abdominal phase. The duration of the abdominal phase was defined by the time between the first incision and the moment that all incisions were closed. The docking time of the robotic system was not registered. Learning curve analyses were performed for the abdominal operating time (in minutes). Secondary outcomes were intraoperative complications, conversion rate, postoperative complications according to the definitions of the Esophagectomy Complications Consensus Group [12], length of hospital stay and in-hospital mortality. Oncological outcomes as lymph node yield and resection margins (R0 = margins not involved, R1 = one or more margins involved) were also extracted. Pneumonia was defined according to the Uniform Pneumonia Score [13]. All patient characteristics and perioperative outcomes were prospectively registered in a database. Complications were discussed and registered during a weekly multidisciplinary team meeting.
Statistics
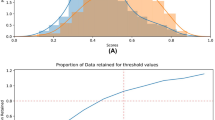
The learning curve for abdominal operation time and abdominal lymph node yield were demonstrated with cumulative sum (CUSUM) analyses (CUSUM = outcome measure of a single patient—mean outcome measure of the total cohort) [7, 14]. CUSUM allows for identifying the length of the learning curve per case instead of analyzing cohorts, resulting in a more precise analysis of the learning curve. The CUSUM formula provides a positive, neutral or negative outcome which is plotted against the mean of the total cohort. This is shown in a graph with the consecutive cases on the horizontal axis and the outcome of the CUSUM formula on the vertical axis. For abdominal operation time, the plateau phase was defined at the point when the operation time started to decrease and for the lymph node yield when the yield increased. Categorical variables were shown as counts with percentage. Continuous variables were shown as means with standard deviation or medians with range. Statistical analyses were performed by using SPSS 25.0 (IBM).
Results
Patients
Between November 2018 and December 2021, 70 consecutive patients underwent full RAMIE with intrathoracic anastomosis. Baseline characteristics are shown in Table 1. The majority of the patients had an adenocarcinoma (n = 55, 79%) and received neoadjuvant chemoradiotherapy (n = 63, 90%).
Intraoperative outcomes
The abdominal operation time was reported in all cases. The median abdominal operating time was 180 min (range 110–233). A CUSUM curve of the abdominal operation time is shown in Fig. 4. The plateau phase occurred at case 22, indicating that the abdominal operation time started to decrease. Total blood loss during RAMIE was median 250 ml (range 100–850). There were no intraoperative complications or conversions during the abdominal phase. During the thoracic phase, 1 complication and 1 conversion occurred. One patient had a bleeding from the subclavian vein which was resolved with a hemoclip. In 1 patient the right lung could not be desufflated requiring conversion to create adequate surgical exposure.
Postoperative outcomes
Postoperative complications are demonstrated in Table 2. Out of 70 patients, 22 (31%) patients developed a postoperative complication Clavien Dindo grade 3 or higher. Anastomotic leakage was diagnosed in 14 patients (20%) and considered grade 1 in 3 patients (4%), grade 2 in 8 patients (11%) and grade 3 in 3 patients (4%). Chyle leak occurred in 5 patients (7%) and pneumonia was diagnosed in 18 patients (26%). The median hospital stay was 12 days (range 6–119). One patient (1%) died in the hospital of aspiration due to mechanic ileus.
Oncological outcomes
A complete resection (i.e., R0) was achieved in 69 patients (99%). The median total lymph node yield was 42 lymph nodes (range 23–83). From March 2019, lymph nodes were collected separately per station according to the LOGICA study protocol. Hence, in 58 patients the lymph node stations were collected separately which is demonstrated in Table 3. From that group, the median abdominal lymph node yield was 16 (range 2–43) and the median thoracic lymph node yield 20 (range 2–46). A median of 6 lymph nodes (0–22) were left attached to the resection specimen or were other lymph node stations. The majority of the abdominal lymph nodes were collected near the left gastric artery (median 4, range 0–20), followed by the hepatic artery (median 3, range 0–9), paracardial (median 2, range 0–12), celiac trunk (median 1, range 0–8) and the splenic artery (median 1, range 0–9). A CUSUM was generated for the abdominal lymph node yield and shown in Fig. 5. After case 21, a plateau phase was observed after which the lymph node yield started to increase.
Discussion
This study reports the implementation of a robot-assisted abdominal phase in 70 consecutive patients who underwent RAMIE for cancer in a high-volume center. There were no intraoperative complications or conversions during the abdominal phase and satisfying postoperative and oncological outcomes were achieved, implying that the implementation of the robot-assisted abdominal phase went safe.
The median abdominal operation time was 180 min (range 110–233). A plateau for abdominal operation time occurred after 22 cases, demonstrated by the CUSUSM analysis. Previous analysis of the learning curve of the thoracic phase by our study group demonstrated that 70 cases were needed to reach the first plateau of proficiency and 24 cases when a structured training program was followed [7]. The pre-existing experience of the surgical team in robot-assisted esophagectomy likely resulted in a shorter learning curve compared to the thoracic phase [15]. In addition, the more than 10 year experience in laparoscopy was probably an advantage compared to a transition from laparotomy to a robot-assisted abdominal phase. Nevertheless, after 43 cases, an increase in operation time was observed. This may be caused by proctoring, as parts of the abdominal phase were performed by fellows in the context of proctoring. Only few other studies demonstrated CUSUM analysis for abdominal operating time during RAMIE. A recent study demonstrated a similar CUSUM for abdominal operation time and showed that the plateau was reached after case 24 [5]. Another study reported a plateau after case 14 for the console time of the robot-assisted abdominal phase.
A recent publication from the Upper GI International Robotic Association (UGIRA) study group demonstrated that only half of the RAMIE procedures are performed fully robotic while the other half consists of a robot-assisted thoracic phase combined with laparoscopy or laparotomy [16]. The added value of a robotic system over laparoscopy during RAMIE is still under debate, as no studies exist specifically comparing conventional laparoscopy to a robot-assisted abdominal phase in RAMIE. However, there are several potential benefits of a robot-assisted abdominal phase. First, the abdominal lymph node dissection around delicate structures (e.g. celiac trunc, hepatic artery, splenic artery) is facilitated by the use of a robotic system. Technical advantages of the robotic system such as a stable camera view, tremor reduction and a fourth arm facilitate a safe though thorough lymph node dissection in this area. In this context several propensity-score matched studies and one randomized control trial have compared abdominal lymph node yield after full RAMIE to full conventional minimally invasive esophagectomy (MIE). All 5 propensity-score matched studies showed a higher abdominal lymph node yield in the robot group, which was statistically significant in 2 studies [17,18,19,20,21]. Results of these studies are summarized in Table 4. The randomized controlled trial comparing 181 full RAMIE patients to 177 full MIE patients with squamous cell carcinoma did not show a difference in abdominal lymph node yield [22]. It must be noted that a median of 7 abdominal lymph nodes (range 4–10) were harvested in both groups which is relatively low especially in contrast with the current study with a median abdominal lymph node yield of 16 (range 2–43). That study might not have focused on the abdominal lymph node making it hard to draw conclusions on the added value of the robot for that part of the procedure.
Although only few studies focused on the abdominal lymph node yield during RAMIE, multiple studies focused on lymph node yield during robot-assisted gastrectomy which has a similar lymphadenectomy. Those studies stated that a robot-assisted lymph node dissection might be superior over laparoscopy which is promising for RAMIE as well [23,24,25]. However, comparing lymph node yield between studies is challenging, since this outcome not only depends on the dissection but also on the methods used for pathology assessment of the resection specimen. Lymph nodes that are separately presented per station instead of en-bloc resections are known to improve lymph node yield, which was the case in the current study [26].
A second potential benefit of a robot-assisted abdominal phase over laparoscopy is that it might be cost-reducing, especially if the thoracic phase is already performed with robotic-assistance. In that case, the same instruments used during the thoracic phase can be used for the abdominal phase instead of a new set of 4–5 laparoscopic instruments, leading to a cost reduction. In addition, recent studies showed that the abdominal operation time for full RAMIE is shorter compared to hybrid RAMIE [22, 27].
Several different analyses are reported to demonstrate the learning curve of RAMIE including CUSUM analyses [29]. A benefit of CUSUM analyses is that it allows for an outcome per individual case, and not per group. Patient outcomes as well as procedure-related outcomes including operation time and blood loss are used for CUSUM analysis [23]. Since patient outcomes generally have a multifactorial etiology, procedure-related outcomes might be more suitable to determine the learning curve. Therefore, this study performed CUSUM analysis for abdominal operation time and lymph node yield.
A strength of this study is the unique level of detail of the dissected abdominal lymph node stations, collected in separate packages in the majority of the patients. In addition, the data was collected in a prospectively maintained database. A limitation might be that the procedures were performed by 2 surgeons who both already completed the learning curve for the robot-assisted thoracic phase. Therefore, the results might not be generalizable to surgeons without robotic experience. On the other hand, it allows for purely investigating the learning curve of the robot-assisted abdominal phase without involving other learning curves.
The results in the current study showed that a robotic system was safely implemented in the abdominal phase during RAMIE achieving satisfying outcomes. In addition, the learning curve for the robot-assisted abdominal phase was relatively short, likely due to the experience in laparoscopy and because the learning curve for robot-assisted thoracic phase was already completed. Future studies should investigate whether a robotic system is of added value for the abdominal phase over laparoscopy during RAMIE. In order to truly compare a robotic abdominal phase to laparoscopy, 2 cohorts without a learning curve should be compared.
References
Van Hillegersberg R, Boone J, Draaisma WA, Broeders IAMJ, Giezeman MJMM, Rinkes IHMB (2006) First experience with robot-assisted thoracoscopic esophagolymphadenectomy for esophageal cancer. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-005-0674-8
van der Sluis PC, van der Horst S, May AM, Schippers C, Brosens LAA, Joore HCA, Kroese CC, Haj Mohammad N, Mook S, Vleggaar FP, Borel Rinkes IHM, Ruurda JP, van Hillegersberg R (2019) Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer: a randomized controlled trial. Ann Surg 269:621–630. https://doi.org/10.1097/SLA.0000000000003031
de Groot EM, Goense L, Ruurda JP, van Hillegersberg R (2021) State of the art in esophagectomy: robotic assistance in the abdominal phase. Updates Surg. 73(3):823–30
Zhang H, Chen L, Wang Z, Zheng Y, Geng Y, Wang F, Liu D, He A, Ma L, Yuan Y, Wang Y (2018) The learning curve for robotic mckeown esophagectomy in patients with esophageal cancer. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2017.11.058
Berlth F, Mann C, Uzun E, Tagkalos E, Hadzijusufovic E, van Hillegersberg R, Li H, Egberts JH, Lang H, Grimminger PP (2020) Technical details of the abdominal part during full robotic-assisted minimally invasive esophagectomy. Dis Esophagus. https://doi.org/10.1093/dote/doaa084
Ruurda JP, Draaisma WA, Van Hillegersberg R, Borel Rinkes IHM, Gooszen HG, Janssen LWM, Simmermacher RKJ, Broeders IAMJ (2005) Robot-assisted endoscopic surgery: a four-year single-center experience. Dig Surg. https://doi.org/10.1159/000088628
van der Sluis PC, Ruurda JP, van der Horst S, Goense L, van Hillegersberg R (2018) Learning curve for robot-assisted minimally invasive thoracoscopic esophagectomy: results from 312 cases. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2018.01.038
de Groot EM, Kuiper GM, van der Veen A, Fourie L, Goense L, van der Horst S, van den Berg JW, van Hillegersberg R, Ruurda JP (2022) Indocyanine green fluorescence in robot-assisted minimally invasive esophagectomy with intrathoracic anastomosis—a prospective study. Updates Surg. https://doi.org/10.1007/s13304-022-01329-y
Haverkamp L, Brenkman HJF, Seesing MFJ, Gisbertz SS, van Berge Henegouwen MI, Luyer MDP, Nieuwenhuijzen GAP, Wijnhoven BPL, van Lanschot JJB, de Steur WO, Hartgrink HH, Stoot JHMB, Hulsewé KWE, Spillenaar Bilgen EJ, Rütter JE, Kouwenhoven EA, van Det MJ, van der Peet DL, Daams F, Draaisma WA, Broeders IAMJ, van Stel HF, Lacle MM, Ruurda JP, van Hillegersberg R (2015) Laparoscopic versus open gastrectomy for gastric cancer, a multicenter prospectively randomized controlled trial (LOGICA-trial). BMC Cancer. https://doi.org/10.1186/s12885-015-1551-z
van der Sluis PC, Ruurda JP, van der Horst S, Verhage RJJ, Besselink MGH, Prins MJD, Haverkamp L, Schippers C, Rinkes IHB, Joore HCA, ten Kate FJW, Koffijberg H, Kroese CC, van Leeuwen MS, Lolkema MPJK, Reerink O, Schipper MEI, Steenhagen E, Vleggaar FP, Voest EE, Siersema PD, van Hillegersberg R (2012) Robot-assisted minimally invasive thoraco-laparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer, a randomized controlled trial (ROBOT trial). Trials. https://doi.org/10.1186/1745-6215-13-230
de Groot EM, Möller T, Kingma BF, Grimminger PP, Becker T, van Hillegersberg R, Egberts JH, Ruurda JP (2020) Technical details of the hand-sewn and circular-stapled anastomosis in robot-assisted minimally invasive esophagectomy. Dis Esophagus 33(2):doaa055
Low DE, Alderson D, Cecconello I, Chang AC, Darling GE, D’Journo XB, Griffin SM, Hölscher AH, Hofstetter WL, Jobe BA, Kitagawa Y, Kucharczuk JC, Law SYK, Lerut TE, Maynard N, Pera M, Peters JH, Pramesh CS, Reynolds JV, Smithers BM, Van Lanschot JJB (2015) International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. https://doi.org/10.1097/SLA.0000000000001098
Seesing MFJ, Wirsching A, Van Rossum PSN, Weijs TJ, Ruurda JP, Van Hillegersberg R, Low DE (2018) Defining pneumonia after esophagectomy for cancer: validation of the Uniform Pneumonia Score in a high volume center in North America. Dis Esophagus. https://doi.org/10.1093/dote/doy002
Feike Kingma B, Hadzijusufovic E, van der Sluis PC, Bano E, Lang H, Ruurda JP, van Hillegersberg R, Grimminger PP (2020) A structured training pathway to implement robot-assisted minimally invasive esophagectomy: the learning curve results from a high-volume center. Dis Esophagus. https://doi.org/10.1093/dote/doaa047
Hsieh MJ, Park SY, Wen YW, Kim DJ, Chiu CH, Chao YK (2022) Impact of prior thoracoscopic experience on the learning curve of robotic McKeown esophagectomy: a multidimensional analysis. Surg Endosc. https://doi.org/10.1007/s00464-022-09050-y
Kingma BF, Grimminger P, van der Sluis P, van Det M, Kouwenhoven E, Chao Y-K, Tsai C-Y, Fuchs H, Bruns C, Sarkaria I, Luketich J, Haveman J, van Etten B, Chiu P, Chan S, Rouanet P, Mourregot A, Hölzen J-P, Sallum R, Cecconello I, Egberts J-H, Benedix F, Henegouwen M, Gisbertz S, Perez D, Jansen K, Hubka M, Low D, Biebl M, Pratschke J, Turner P, Pursnani K, Chaudry A, Smith M, Mazza E, Strignano P, Ruurda J, van Hillegersberg R (2020) Worldwide techniques and outcomes in robot-assisted minimally invasive esophagectomy (RAMIE): results from the Multicenter International Registry. Ann Surg. https://doi.org/10.1097/SLA.0000000000004550
Deng HY, Huang WX, Li G, Li SX, Luo J, Alai G, Wang Y, Liu LX, Lin YD (2018) Comparison of short-term outcomes between robot-assisted minimally invasive esophagectomy and video-assisted minimally invasive esophagectomy in treating middle thoracic esophageal cancer. Dis Esophagus. https://doi.org/10.1093/dote/doy012
Deng HY, Luo J, Li SX, Li G, Alai G, Wang Y, Liu LX, Lin YD (2019) Does robot-assisted minimally invasive esophagectomy really have the advantage of lymphadenectomy over video-assisted minimally invasive esophagectomy in treating esophageal squamous cell carcinoma? A propensity score-matched analysis based on short-term. Dis Esophagus. https://doi.org/10.1093/dote/doy110
Zhang Y, Han Y, Gan Q, Xiang J, Jin R, Chen K, Che J, Hang J, Li H (2019) Early outcomes of robot-assisted versus thoracoscopic-assisted Ivor Lewis esophagectomy for esophageal cancer: a propensity score-matched study. Ann Surg Oncol. https://doi.org/10.1245/s10434-019-07273-3
Yang Y, Zhang X, Li B, Hua R, Yang Y, He Y, Ye B, Guo X, Sun Y, Li Z (2020) Short- and mid-term outcomes of robotic versus thoraco-laparoscopic McKeown esophagectomy for squamous cell esophageal cancer: a propensity score-matched study. Dis Esophagus. https://doi.org/10.1093/dote/doz080
Xu Y, Li XK, Cong ZZ, Zhou H, Wu WJ, Qiang Y, Yi J, Shen Y (2021) Long-term outcomes of robotic-assisted versus thoraco-laparoscopic McKeown esophagectomy for esophageal cancer: a propensity score-matched study. Dis Esophagus. https://doi.org/10.1093/dote/doaa114
Yang Y, Li B, Yi J, Hua R, Chen H, Tan L, Li H, He Y, Guo X, Sun Y, Yu B, Li Z (2021) Robot-assisted versus conventional minimally invasive esophagectomy for resectable esophageal squamous cell carcinoma. Ann Surg. https://doi.org/10.1097/sla.0000000000005023
Marano L, Fusario D, Savelli V, Marrelli D, Roviello F (2021) Robotic versus laparoscopic gastrectomy for gastric cancer: an umbrella review of systematic reviews and meta-analyses. Updates Surg 5:1673–1689
Li Z, Li J, Li B, Bai B, Liu Y, Lian B, Zhao Q (2018) Robotic versus laparoscopic gastrectomy with D2 lymph node dissection for advanced gastric cancer: a propensity score-matched analysis. Cancer Manag Res 10:705–714. https://doi.org/10.2147/CMAR.S161007
Cianchi F, Indennitate G, Trallori G, Ortolani M, Paoli B, Macrì G, Lami G, Mallardi B, Badii B, Staderini F, Qirici E, Taddei A, Ringressi MN, Messerini L, Novelli L, Bagnoli S, Bonanomi A, Foppa C, Skalamera I, Fiorenza G, Perigli G (2016) Robotic vs laparoscopic distal gastrectomy with D2 lymphadenectomy for gastric cancer: a retrospective comparative mono-institutional study. BMC Surg 16:1–6. https://doi.org/10.1186/s12893-016-0180-z
Veeramachaneni NK, Zoole JB, Decker PA, Putnam JB, Meyers BF (2008) Lymph node analysis in esophageal resection: American College of Surgeons Oncology Group Z0060 Trial. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2008.04.043
Grimminger PP, Staubitz JI, Perez D, Ghadban T, Reeh M, Scognamiglio P, Izbicki JR, Biebl M, Fuchs H, Bruns CJ, Lang H, Becker T, Egberts JH (2021) Multicenter experience in robot-assisted minimally invasive esophagectomy—a comparison of hybrid and totally robot-assisted techniques. J Gastrointest Surg. https://doi.org/10.1007/s11605-021-05044-8
Goense L, van Dijk WA, Govaert JA, van Rossum PSN, Ruurda JP, van Hillegersberg R (2017) Hospital costs of complications after esophagectomy for cancer. Eur J Surg Oncol 43:696–702. https://doi.org/10.1016/j.ejso.2016.11.013
Claassen L, van Workum F, Rosman C (2019) Learning curve and postoperative outcomes of minimally invasive esophagectomy. J Thorac Dis 11(5):777–785
Acknowledgements
There are no acknowledgements.
Funding
No funding is received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jelle Ruurda and Richard van Hillegersberg are both proctors for Intuitive Surgical Inc and consultants for Medtronic. Eline de Groot, Lucas Goense,Feike Kingma and Jan Willem van den Berg have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Groot, E.M., Goense, L., Kingma, B.F. et al. Implementation of the robotic abdominal phase during robot-assisted minimally invasive esophagectomy (RAMIE): results from a high-volume center. Surg Endosc 37, 1357–1365 (2023). https://doi.org/10.1007/s00464-022-09681-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09681-1