Abstract
Background
More complex cases are being performed robotically. This study aims to characterize trends in robotic pancreatoduodenectomy (RPD) over time and assess opportunities for advanced trainees.
Methods
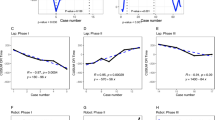
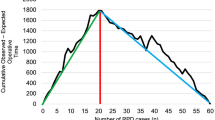
Using the ACS-NSQIP database from 2014 to 2019, PD cases were characterized by operative approach (open-OPN, laparoscopic-LAP, robotic-ROB). Proficiency and postoperative outcomes were described by approach over time.
Results
24,268 PDs were identified, with the ROB approach increasing from 2.8% to 7.5%. Unplanned conversion increased over time for LAP (27.7–39.0%, p = 0.003) but was unchanged for ROB cases (14.8–14.7%, p = 0.257). Morbidity increased for OPN PD (35.5–36.8%, p = 0.041) and decreased for ROB PD (38.7–30.3%, p = 0.010). Mean LOS was lower in ROB than LAP/OPN (9.5 vs. 10.9 vs. 10.9 days, p < 0.00001). Approximately, 100 AHPBA, SSO, and ASTS fellows are being trained each year in North America; however, only about 5 RPDs are available per trainee per year which is far below that recommended to achieve proficiency.
Conclusion
Over a 6-year period, a significant increase was observed in the use of RPD without a concomitant increase in conversion rates. RPD was associated with decreased morbidity and length of stay. Despite this shift, the number of cases being performed is not adequate for all fellows to achieve proficiency before graduation.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the American College of Surgeons. Restrictions apply to the availability of these data, which were used under license for this study. Data are available for request at https://www.facs.org/quality-programs/acs-nsqip/participant-use/puf-form with the permission of the American College of Surgeons.
References
Hoehn RS, Nassour I, Adam MA, Winters S, Paniccia A, Zureikat AH (2021) National trends in robotic pancreas surgery. J Gastrointest Surg 25(4):983–990. https://doi.org/10.1007/s11605-020-04591-w
Hogg ME, Besselink MG, Clavien PA et al (2017) Training in minimally invasive pancreatic resections: a paradigm shift away from “See one, Do one, Teach one.” HPB 19(3):234–245. https://doi.org/10.1016/j.hpb.2017.01.016
Mark Knab L, Zenati MS, Khodakov A et al (2018) Evolution of a novel robotic training curriculum in a complex general surgical oncology fellowship. Ann Surg Oncol 25(12):3445–3452. https://doi.org/10.1245/s10434-018-6686-0
Nota CL, Zwart MJ, Fong Y et al (2017) Developing a robotic pancreas program: the Dutch experience. J Vis Surg 3:106. https://doi.org/10.21037/jovs.2017.07.02
Schmidt CR, Harris BR, Musgrove KA et al (2021) Formal robotic training diminishes the learning curve for robotic pancreatoduodenectomy: Implications for new programs in complex robotic surgery. J Surg Oncol 123(2):375–380. https://doi.org/10.1002/jso.26284
Napoli N, Kauffmann EF, Palmeri M et al (2016) The learning curve in robotic pancreaticoduodenectomy. Dig Surg 33(4):299–307. https://doi.org/10.1159/000445015
Shyr BU, Chen SC, Shyr YM, Wang SE (2018) Learning curves for robotic pancreatic surgery-from distal pancreatectomy to pancreaticoduodenectomy. Medicine 97(45):e13000. https://doi.org/10.1097/MD.0000000000013000
Boone BA, Zenati M, Hogg ME et al (2015) Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg 150(5):416–422. https://doi.org/10.1001/jamasurg.2015.17
Tzeng CW, Cooper AB, Vauthey JN, Curley SA, Aloia TA (2014) Predictors of morbidity and mortality after hepatectomy in elderly patients: analysis of 7621 NSQIP patients. HPB 16(5):459–468. https://doi.org/10.1111/hpb.12155
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591. https://doi.org/10.1016/j.surg.2016.11.014
Beane JD, Borrebach JD, Zureikat AH, Kilbane EM, Thompson VM, Pitt HA (2019) Optimal pancreatic surgery: are we making progress in North America? Ann Surg. https://doi.org/10.1097/SLA.0000000000003628
https://www.surgonc.org/fellows/surgical-oncology-fellowships/. Accessed 1 Feb 2021
https://www.ahpba.org/education-training/. Accessed 1 Feb 2021
https://asts.org/training/transplant-accreditation-certification-council. Accessed 1 Feb 2021
Zimmerman AM, Roye DG, Charpentier KP (2018) A comparison of outcomes between open, laparoscopic and robotic pancreaticoduodenectomy. HPB 20(4):364–369. https://doi.org/10.1016/j.hpb.2017.10.008
Gleeson EM, Pitt HA, Mackay TM et al (2021) Failure to rescue after pancreatoduodenectomy: a transatlantic analysis. Ann Surg 274(3):459–466. https://doi.org/10.1097/SLA.0000000000005000
Kim HS, Han Y, Kang JS et al (2018) Comparison of surgical outcomes between open and robot-assisted minimally invasive pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci 25(2):142–149. https://doi.org/10.1002/jhbp.522
Jin J, Yin SM, Weng Y et al (2022) Robotic versus open pancreaticoduodenectomy with vascular resection for pancreatic ductal adenocarcinoma: surgical and oncological outcomes from pilot experience. Langenbecks Arch Surg. https://doi.org/10.1007/s00423-021-02364-w
Palanivelu C, Senthilnathan P, Sabnis SC et al (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104(11):1443–1450. https://doi.org/10.1002/bjs.10662
Poves I, Burdío F, Morató O et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP Randomized Controlled Trial. Ann Surg 268(5):731–739. https://doi.org/10.1097/SLA.0000000000002893
Kendrick ML, Cusati D (2010) Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg 145(1):19–23. https://doi.org/10.1001/archsurg.2009.243
Kantor O, Pitt HA, Talamonti MS et al (2018) Minimally invasive pancreatoduodenectomy: is the incidence of clinically relevant postoperative pancreatic fistula comparable to that after open pancreatoduodenectomy? Surgery 163(3):587–593. https://doi.org/10.1016/j.surg.2017.12.001
Gall TMH, Alrawashdeh W, Soomro N, White S, Jiao LR (2020) Shortening surgical training through robotics: randomized clinical trial of laparoscopic versus robotic surgical learning curves. BJS Open. https://doi.org/10.1002/bjs5.50353
van Hilst J, de Rooij T, Bosscha K et al (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4(3):199–207. https://doi.org/10.1016/S2468-1253(19)30004-4
Lane T (2018) A short history of robotic surgery. Ann R Coll Surg Engl 100(6_sup):5–7. https://doi.org/10.1308/rcsann.supp1.5
Giulianotti PC, Coratti A, Angelini M et al (2003) Robotics in general surgery: personal experience in a large community hospital. Arch Surg 138(7):777–784. https://doi.org/10.1001/archsurg.138.7.777
Chen K, Pan Y, Liu XL et al (2017) Minimally invasive pancreaticoduodenectomy for periampullary disease: a comprehensive review of literature and meta-analysis of outcomes compared with open surgery. BMC Gastroenterol 17(1):120. https://doi.org/10.1186/s12876-017-0691-9
Aiolfi A, Lombardo F, Bonitta G, Danelli P, Bona D (2021) Systematic review and updated network meta-analysis comparing open, laparoscopic, and robotic pancreaticoduodenectomy. Updates Surg 73(3):909–922. https://doi.org/10.1007/s13304-020-00916-1
Kamarajah SK, Bundred J, Marc OS et al (2020) Robotic versus conventional laparoscopic pancreaticoduodenectomy a systematic review and meta-analysis. Eur J Surg Oncol 46(1):6–14. https://doi.org/10.1016/j.ejso.2019.08.007
Zureikat AH, Borrebach J, Pitt HA et al (2017) Minimally invasive hepatopancreatobiliary surgery in North America: an ACS-NSQIP analysis of predictors of conversion for laparoscopic and robotic pancreatectomy and hepatectomy. HPB 19(7):595–602. https://doi.org/10.1016/j.hpb.2017.03.004
van Hilst J, de Graaf N, Abu Hilal M, Besselink MG (2021) The landmark series: minimally invasive pancreatic resection. Ann Surg Oncol 28(3):1447–1456. https://doi.org/10.1245/s10434-020-09335-3
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Vining CC, Hogg ME (2020) How to train and evaluate minimally invasive pancreas surgery. J Surg Oncol 122(1):41–48. https://doi.org/10.1002/jso.25912
Madion MP, Kastenmeier A, Goldblatt MI, Higgins RM (2022) Robotic surgery training curricula: prevalence, perceptions, and educational experiences in general surgery residency programs. Surg Endosc. https://doi.org/10.1007/s00464-021-08930-z
Ramirez Barriga M, Rojas A, Roggin KK, Talamonti MS, Hogg ME (2022) Development of a two-week dedicated robotic surgery curriculum for general surgery residents. J Surg Educ. https://doi.org/10.1016/j.jsurg.2022.02.015
Radi I, Tellez JC, Alterio RE et al (2022) Feasibility, effectiveness and transferability of a novel mastery-based virtual reality robotic training platform for general surgery residents. Surg Endosc. https://doi.org/10.1007/s00464-022-09106-z
Moran GW, Margolin EJ, Wang CN, DeCastro GJ (2022) Using gamification to increase resident engagement in surgical training: our experience with a robotic surgery simulation league. Am J Surg. https://doi.org/10.1016/j.amjsurg.2022.01.020
Liounakos JI, Basil GW, Urakawa H, Wang MY (2021) Intraoperative image guidance for endoscopic spine surgery. Ann Transl Med 9(1):92. https://doi.org/10.21037/atm-20-1119
Ma AK, Daly M, Qiu J et al (2017) Intraoperative image guidance in transoral robotic surgery: a pilot study. Head Neck 39(10):1976–1983. https://doi.org/10.1002/hed.24805
van der Poel HG, Buckle T, Brouwer OR, Valdés Olmos RA, van Leeuwen FW (2011) Intraoperative laparoscopic fluorescence guidance to the sentinel lymph node in prostate cancer patients: clinical proof of concept of an integrated functional imaging approach using a multimodal tracer. Eur Urol 60(4):826–833. https://doi.org/10.1016/j.eururo.2011.03.024
Baker EH, Dowden JE, Cochran AR et al (2016) Qualities and characteristics of successfully matched North American HPB surgery fellowship candidates. HPB 18(5):479–484. https://doi.org/10.1016/j.hpb.2015.12.001
Warner SG, Alseidi AA, Hong J, Pawlik TM, Minter RM (2015) What to expect when you’re expecting a hepatopancreatobiliary surgeon: self-reported experiences of HPB surgeons from different training pathways. HPB 17(9):785–790. https://doi.org/10.1111/hpb.12430
DAngelica MI, Chapman WC (2016) HPB surgery: the specialty is here to stay, but the training is in evolution. Ann Surg Oncol 23(7):2123–2125. https://doi.org/10.1245/s10434-016-5230-3
Sweigert PJ, Eguia E, Baker MS et al (2020) Assessment of textbook oncologic outcomes following pancreaticoduodenectomy for pancreatic adenocarcinoma. J Surg Oncol 121(6):936–944. https://doi.org/10.1002/jso.25861
Funding
This study was not funded by an outside source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Catherine Davis, Miral Grandhi, Victor Gazivoda, Alissa Greenbaum, Timothy Kennedy, Russell Langan, H. Richard Alexander, Henry Pitt, and David August have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Davis, C.H., Grandhi, M.S., Gazivoda, V.P. et al. Robotic pancreatoduodenectomy: trends in technique and training challenges. Surg Endosc 37, 266–273 (2023). https://doi.org/10.1007/s00464-022-09469-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09469-3