Abstract
Background and aims
Gastrointestinal stromal tumors (GIST) are mostly seen in the stomach. Clinical data on GISTs ≤ 2 cm with > 5 mitosis/50 HPFs are limited. This study aimed to analyze small GISTs with high histological grades to gain a more comprehensive understanding of their clinical characteristics with long-term follow-up.
Methods
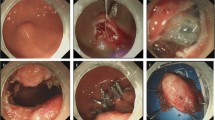
This was a nested cohort study of patients with gastric GISTs ≤ 2 cm and > 5 mitosis/50 HPFs. Individuals with endoscopically resected gastric specimens diagnosed as GISTs between January 2008 and July 2019 were enrolled. We analyzed baseline clinicopathological characteristics, perioperative characteristics, risk of recurrence, and metastasis during follow-up.
Results
A total of 55 patients diagnosed with gastric GISTs ≤ 2 cm and > 5 mitosis/50 HPFs were enrolled. The mean tumor size was 1.6 ± 0.4 cm (median 1.7 cm, range 0.8–2.0 cm). ESD was performed in 33 patients (60.0%) and EFTR in 22 patients (40.0%). Mean mitotic figures were 8.9/50 HPFs. Postoperative bleeding in one patient (1.8%) was the only severe adverse event. The mean follow-up period was 61.2 ± 33.9 months (median 53 months, range 13–133 months). Five patients (5/55, 9.1%) received additional therapies, including partial gastrectomy and adjuvant Imatinib. Only two patients (2/55, 3.6%) showed signs of recurrence. We observed no significant difference regarding baseline clinical characteristics and recurrence among GISTs with mitosis < 10/50 HPF and ≥ 10/50 HPF. No patient had signs of metastasis during follow-up.
Conclusion
Endoscopic resection of gastric GISTs ≤ 2 cm with > 5 mitosis/50 HPFs has a low risk of recurrence and metastasis in the long term. Endoscopic resection of GISTs is safe and feasible.



Similar content being viewed by others
Abbreviations
- GIST:
-
Gastrointestinal stromal tumor
- ESD:
-
Endoscopic submucosal dissection
- EFTR:
-
Endoscopic full-thickness resection
- HPF:
-
High power field
- GI:
-
Gastrointestinal
- NCCN:
-
National comprehensive cancer network
- SEL:
-
Subepithelial lesion
- ASGE:
-
American society of gastrointestinal endoscopy
References
Miettinen M, Sobin LH, Lasota J (2005) Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 29(1):52–68
Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 23(2):70–83
Pidhorecky I, Cheney RT, Kraybill WG et al (2000) Gastrointestinal stromal tumors: current diagnosis, biologic behavior, and management. Ann Surg Oncol 7(9):705–712
Nilsson B, Bümming P, Meis-Kindblom JM et al (2005) Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era–a population-based study in western Sweden. Cancer 103(4):821–829
National Comprehensive Cancer Network (NCCN) (2016) Clinical practice guidelines in oncology. Soft Tissue Sarcoma, Version 1.2016
National Comprehensive Cancer Network (NCCN) (2019) Clinical practice guidelines in oncology. Soft Tissue Sarcoma, Version 6.2019
ASGE Technology Committee (2019) ASGE guideline for endoscopic full-thickness resection and submucosal tunnel endoscopic resection. VideoGIE 4(8):343–350
Xiu H, Zhao C-Y, Liu F-G et al (2019) Comparing about three types of endoscopic therapy methods for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. Scand J Gastroenterol 54(12):1481–1486
Chen Du, Chai N, Linghu E et al (2018) Treatment of cardial submucosal tumors originating from the muscularis propria layer: submucosal tunneling endoscopic resection versus endoscopic submucosal excavation. Surg Endosc 32(11):4543–4551
Hou Y-Y, Lu S-H, Zhou Y et al (2009) Predictive values of clinical and pathological parameters for malignancy of gastrointestinal stromal tumors. Histol Histopathol 24(6):737–747
Zhu Y, Mei-Dong Xu, Chen Xu et al (2020) Microscopic positive tumor margin does not increase the rate of recurrence in endoscopic resected gastric mesenchymal tumors compared to negative tumor margin. Surg Endosc 34(1):159–169
Li B, Chen T, Qi ZP et al (2019) Efficacy and safety of endoscopic resection for small submucosal tumors originating from the muscularis propria layer in the gastric fundus. Surg Endosc 33(8):2553–2561
Du C, Chai N, Linghu E et al (2018) Treatment of cardial submucosal tumors originating from the muscularis propria layer: submucosal tunneling endoscopic resection versus endoscopic submucosal excavation. Surg Endosc 32(11):4543–4551
Liu S, Zhou X, Yao Y et al (2020) Resection of the gastric submucosal tumor (G-SMT) originating from the muscularis propria layer: comparison of efficacy, patients’ tolerability, and clinical outcomes between endoscopic full-thickness resection and surgical resection. Surg Endosc. https://doi.org/10.1007/s00464-019-07311-x
Zhao Y, Pang T, Zhang B et al (2019) Retrospective comparison of endoscopic full-thickness versus laparoscopic or surgical resection of small (≤5 cm) gastric gastrointestinal stromal tumors. J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04493-6
Khashab MA, Pasricha PJ (2013) Conquering the third space: challenges and opportunities for diagnostic and therapeutic endoscopy. Gastrointest Endosc 77(1):146–148
Joo MK, Park J-J, Kim Ho et al (2016) Endoscopic versus surgical resection of GI stromal tumors in the upper GI tract. Gastrointest Endosc 83(2):318–326
Gronchi A, Bonvalot S, Velasco AP et al (2020) Quality of surgery and outcome in localized gastrointestinal stromal tumors treated within an international intergroup randomized clinical trial of adjuvant imatinib. JAMA Surg 155(6):e200397
McCarter MD, Antonescu CR, Ballman KV et al (2012) Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg 215(1):53–59
Pantuso G, Macaione I, Taverna A et al (2019) Surgical treatment of primary gastrointestinal stromal tumors (GISTs): management and prognostic role of R1 resections. Am J Surg. https://doi.org/10.1016/j.amjsurg.2019.12.006
Hølmebakk T, Hompland I, Bjerkehagen B et al (2018) Recurrence-free survival after resection of gastric gastrointestinal stromal tumors classified according to a strict definition of tumor rupture: a population-based study. Ann Surg Oncol 25(5):1133–1139
Nishida T, Hølmebakk T, Raut CP et al (2019) Defining tumor rupture in gastrointestinal stromal tumor. Ann Surg Oncol 26(6):1669–1675
Andalib I, Yeoun D, Reddy R et al (2018) Endoscopic resection of gastric gastrointestinal stromal tumors originating from the muscularis propria layer in North America: methods and feasibility data. Surg Endosc 32(4):1787–1792
Funding
None.
Author information
Authors and Affiliations
Contributions
TC and JX participated in the original draft preparation. WC, QL, MC, JH, WQ, and XX contributed to resources. YJ contributed to resources and methodology. YZ participated in the conceptualization, supervision, and reviewing and editing of the manuscript. PZ participated in the reviewing and editing of the manuscript.
Corresponding authors
Ethics declarations
Disclosures
Drs. Tian-Yin Chen, Jia-Xin Xu, Wei-Feng Chen, Quan-Lin Li, Ming-Yan Cai, Jian-Wei Hu, Wen-Zheng Qin, Yuan Ji, Xiao-Yue Xu, Yi-Qun Zhang, and Ping-Hong Zhou have no conflicts of interest or financial ties to disclose. All authors disclosed no financial relationships relevant to this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, TY., Xu, JX., Chen, WF. et al. Long-term prognosis of small gastric gastrointestinal stromal tumors with high histological grade: a longitudinal nested cohort study. Surg Endosc 36, 4042–4049 (2022). https://doi.org/10.1007/s00464-021-08725-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08725-2