Abstract
Background
Fundoplication and medical management are current mainstays for management of Barrett’s esophagus (BE), however our understanding of differences in outcomes between these two treatments is limited. The aim of this study was to perform a systematic review and meta-analysis to evaluate the efficacy of these interventions on BE disease regression and progression.
Methods and procedures
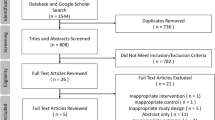
A comprehensive search in MEDLINE, EMBASE, Scopus, Web of Science, and Cochrane Library databases was performed on February 22, 2021. Inclusion criteria were studies with both medical and surgical management comparators, BE diagnosis prior to treatment, patients aged ≥ 18 years, and studies with greater than five patients. Primary outcomes of interest included evaluating changes in histopathologic BE regression and disease progression between interventions. Meta-analysis was performed using a Mantel–Haenszel random-effects model (RevMan 5.4.1).
Results
A total of 7231 studies were retrieved after initial search with nine studies (1 randomized trial, 7 prospective cohorts, 1 retrospective cohort) meeting final inclusion criteria. Of included studies, 890 (65%) patients received medical management while 470 (35%) received surgical management. Medical management included proton pump inhibitors (n = 807, 91%; 6 studies), H2-receptor blockers (n = 40, 4% patients; 3 studies), and combination therapy (n = 43, 5%; 1 study). Nissen fundoplication was the most commonly performed type of fundoplication (n = 265, 93%). Median length of follow-up ranged from 1.5–7 years. Meta-analysis revealed that fundoplication was associated with improved histopathologic regression of metaplasia/low-grade dysplasia (OR 4.38; 95% CI 2.28–8.42; p < 0.00001) and disease progression to dysplasia/adenocarcinoma (OR 0.34; 95% CI 0.12–0.96; p = 0.04) compared to medical therapy.
Conclusion
Fundoplication is superior to medical therapy with regards to improved odds of histopathologic BE disease regression and disease progression. Additional randomized trials which directly compare medical management and surgical intervention are required to delineate the optimal delivery and timing of these interventions.



Similar content being viewed by others
References
Hvid-Jensen F, Pedersen L, Drewes AM, Sørensen HT, Funch-Jensen P (2011) Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med 365:1375–1383. https://doi.org/10.1056/NEJMoa1103042
Marques de Sá I, Pereira AD, Sharma P, Dinis-Ribeiro M (2020) Systematic review of the published guidelines on Barrett’s esophagus: should we stress the consensus or the differences? Dis esophagus Off J Int Soc Dis Esophagus. https://doi.org/10.1093/dote/doaa115
Kestens C, Offerhaus GJA, van Baal JWPM, Siersema PD (2016) Patients with Barrett’s esophagus and persistent low-grade dysplasia have an increased risk for high-grade dysplasia and cancer. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 14:956-962.e1. https://doi.org/10.1016/j.cgh.2015.12.027
Canadian Cancer Society (2019) Survival Statistics for Esophageal Cancer. Available at https://www.cancer.ca/en/cancer-information/cancer-type/esophageal/prognosis-and-survival/survival-statistics/?region=qc. Accessed 16 Jan 2020
Runge TM, Abrams JA, Shaheen NJ (2015) Epidemiology of Barrett’s esophagus and esophageal adenocarcinoma. Gastroenterol Clin North Am 44:203–231. https://doi.org/10.1016/j.gtc.2015.02.001
Maret-Ouda J, Markar SR, Lagergren J (2020) Gastroesophageal reflux disease: a review. JAMA 324:2536–2547. https://doi.org/10.1001/jama.2020.21360
Society of American Gastrointestinal and Endoscopic Surgeons (2020) Survival Statistics for Esophageal Cancer. https://www.sages.org/publications/guidelines/guidelines-for-surgical-treatment-of-gastroesophageal-reflux-disease-gerd/. Accessed 3 Dec 2020
Attwood SEA, Lundell L, Ell C, Galmiche J-P, Hatlebakk J, Fiocca R, Lind T, Eklund S, Junghard O (2008) Standardization of surgical technique in antireflux surgery: the LOTUS trial experience. World J Surg 32:995–998. https://doi.org/10.1007/s00268-007-9409-4
Maret-Ouda J, Konings P, Lagergren J, Brusselaers N (2016) Antireflux surgery and risk of esophageal adenocarcinoma: a systematic review and meta-analysis. Ann Surg 263:251–257. https://doi.org/10.1097/SLA.0000000000001438
Haddaway NR, Collins AM, Coughlin DKS (2015) The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE. https://doi.org/10.1371/journal.pone.0138237
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2020) Cochrane handbook for systematic reviews of interventions version 6.1. Available at www.training.cochrane.org/handbook. Accessed 15 Dec 2020
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Attwood SE, Barlow AP, Norris TL, Watson A (1992) Barrett’s oesophagus: effect of antireflux surgery on symptom control and development of complications. Br J Surg 79:1050–1053. https://doi.org/10.1002/bjs.1800791021
Gurski RR, Peters JH, Hagen JA, DeMeester SR, Bremner CG, Chandrasoma PT, DeMeester TR (2003) Barrett’s esophagus can and does regress after antireflux surgery: a study of prevalence and predictive features. J Am Coll Surg 196:703–706. https://doi.org/10.1016/S1072-7515(03)00147-9
Markar SR, Arhi C, Leusink A, Vidal-Diez A, Karthikesalingam A, Darzi A, Lagergren J, Hanna GB (2018) The influence of antireflux surgery on esophageal cancer risk in England: national population-based cohort study. Ann Surg 268:861–867. https://doi.org/10.1097/SLA.0000000000002890
Oberg S, Wenner J, Johansson J, Walther B, Willén R (2005) Barrett esophagus: risk factors for progression to dysplasia and adenocarcinoma. Ann Surg 242:49–54. https://doi.org/10.1097/01.sla.0000167864.46462.9f
Parrilla P, Martínez de Haro LF, Ortiz A, Munitiz V, Molina J, Bermejo J, Canteras M (2003) Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett’s esophagus. Ann Surg 237:291–298. https://doi.org/10.1097/01.SLA.0000055269.77838.8E
Rossi M, Barreca M, de Bortoli N, Renzi C, Santi S, Gennai A, Bellini M, Costa F, Conio M, Marchi S (2006) Efficacy of Nissen fundoplication versus medical therapy in the regression of low-grade dysplasia in patients with Barrett esophagus: a prospective study. Ann Surg 243:58–63. https://doi.org/10.1097/01.sla.0000194085.56699.db
Trentino MDP, Trifero MDM, Marzullo MDA, Arcese MDR, Correnti MDFS, Pappalardo MDG, Castrini MDG (1990) Biomarkers’ evaluation for early neoplastic degeneration in Barrett’s esophagus. A preliminary report on 12 cases. Dis Esophagus 3:29–36. https://doi.org/10.1093/dote/3.1.29
Tolone S, Limongelli P, Romano M, Federico A, Docimo G, Ruggiero R, Brusciano L, Del Genio G, Docimo L (2015) The patterns of reflux can affect regression of non-dysplastic and low-grade dysplastic Barrett’s esophagus after medical and surgical treatment: a prospective case-control study. Surg Endosc 29:648–657. https://doi.org/10.1007/s00464-014-3713-5
Zaninotto G, Parente P, Salvador R, Farinati F, Tieppo C, Passuello N, Zanatta L, Fassan M, Cavallin F, Costantini M, Mescoli C, Battaglia G, Ruol A, Ancona E, Rugge M (2012) Long-term follow-up of Barrett’s epithelium: medical versus antireflux surgical therapy. J Gastrointest Surg Off J Soc Surg Aliment Tract 16:5–7. https://doi.org/10.1007/s11605-011-1739-8
Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ, Association AG (2011) American gastroenterological association technical review on the management of Barrett’s esophagus. Gastroenterol 140:e18–e13. https://doi.org/10.1053/j.gastro.2011.01.031
Oh DS, Demeester SR (2010) Pathophysiology and treatment of Barrett’s esophagus. World J Gastroenterol 16:3762–3772. https://doi.org/10.3748/wjg.v16.i30.3762
Tobey NA, Hosseini SS, Argote CM, Dobrucali AM, Awayda MS, Orlando RC (2004) Dilated intercellular spaces and shunt permeability in nonerosive acid-damaged esophageal epithelium. Am J Gastroenterol 99:13–22. https://doi.org/10.1046/j.1572-0241.2003.04018.x
Oberg S, Peters JH, DeMeester TR, Chandrasoma P, Hagen JA, Ireland AP, Ritter MP, Mason RJ, Crookes P, Bremner CG (1997) Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg 226:522–532. https://doi.org/10.1097/00000658-199710000-00013
Nasr AO, Dillon MF, Conlon S, Downey P, Chen G, Ireland A, Leen E, Bouchier-Hayes D, Walsh TN (2012) Acid suppression increases rates of Barrett’s esophagus and esophageal injury in the presence of duodenal reflux. Surgery 151:382–390. https://doi.org/10.1016/j.surg.2011.08.021
Jürgens S, Meyer F, Spechler SJ, Souza R (2012) The role of bile acids in the neoplastic progression of Barrett’s esophagus - a short representative overview. Z Gastroenterol 50:1028–1034. https://doi.org/10.1055/s-0032-1312922
Kauer WK, Peters JH, DeMeester TR, Ireland AP, Bremner CG, Hagen JA (1995) Mixed reflux of gastric and duodenal juices is more harmful to the esophagus than gastric juice alone. The need for surgical therapy re-emphasized. Ann Surg 222:525–533. https://doi.org/10.1097/00000658-199522240-00010
Stein HJ, Kauer WKH, Feussner H, Siewert JR (1998) Bile reflux in benign and malignant Barrett’s esophagus: effect of medical acid suppression and Nissen fundoplication. J Gastrointest Surg 2:333–341. https://doi.org/10.1016/S1091-255X(98)80072-3
Niebisch S, Fleming FJ, Galey KM, Wilshire CL, Jones CE, Litle VR, Watson TJ, Peters JH (2012) Perioperative risk of laparoscopic fundoplication: safer than previously reported—analysis of the American college of surgeons national surgical quality improvement program 2005 to 2009. JACS 215:61–68. https://doi.org/10.1016/j.jamcollsurg.2012.03.022
Cameron AJ (1999) Barrett’s esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol 94:2054–2059. https://doi.org/10.1111/j.1572-0241.1999.01277.x
Roman S, Kahrilas PJ (2015) Mechanisms of Barrett’s oesophagus (clinical): LOS dysfunction, hiatal hernia, peristaltic defects. Best Pract Res Clin Gastroenterol 29:17–28. https://doi.org/10.1016/j.bpg.2014.11.002
Van Soest EM, Siersema PD, Dieleman JP, Sturkenboom MCJM, Kuipers EJ (2006) Persistence and adherence to proton pump inhibitors in daily clinical practice. Aliment Pharmacol Ther 24:377–385. https://doi.org/10.1111/j.1365-2036.2006.02982.x
Hungin APS, Hill C, Molloy-Bland M, Raghunath A (2012) Systematic review: patterns of proton pump inhibitor use and adherence in gastroesophageal reflux disease. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 10:109–116. https://doi.org/10.1016/j.cgh.2011.07.008
El-Serag HB, Fitzgerald S, Richardson P (2009) The extent and determinants of prescribing and adherence with acid-reducing medications: a national claims database study. Am J Gastroenterol 104:2161–2167. https://doi.org/10.1038/ajg.2009.312
Corey KE, Schmitz SM, Shaheen NJ (2003) Does a surgical antireflux procedure decrease the incidence of esophageal adenocarcinoma in Barrett’s esophagus? A meta-analysis. Am J Gastroenterol 98:2390–2394. https://doi.org/10.1111/j.1572-0241.2003.08702.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ms. Wilson and Kung, and Drs. Mocanu, Sun, Deng, Jogiat, Switzer, Wong and Karmali have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.



Rights and permissions
About this article
Cite this article
Wilson, H., Mocanu, V., Sun, W. et al. Fundoplication is superior to medical therapy for Barrett’s esophagus disease regression and progression: a systematic review and meta-analysis. Surg Endosc 36, 2554–2563 (2022). https://doi.org/10.1007/s00464-021-08543-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08543-6