Abstract
Background
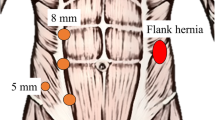
The flank approach to lumbar spine surgery is considered a new minimally invasive alternative to the anterior abdominal approach. Flank incisional hernia is one complication, but it has been poorly studied.
Methods
Retrospective review of patients referred for evaluation of abdominal bulging after Lateral Interbody Fusion (LIF), 2013–2020.
Results
Seventeen patients were evaluated for abdominal bulging after LIF: 14 were diagnosed with incisional hernias. Three with denervation injury without hernia defect were excluded.
Conclusions
This is the largest study addressing incisional flank hernias after LIF, an under-represented complication in the spine literature. We show that the patients present early, within months of their operation, and yet most hernias are not diagnosed for over a year. Although LIF is considered a minimally invasive procedure, the morbidity from hernia complications cannot be overlooked. These flank hernias are difficult to repair with suboptimal outcomes. We prefer robotic approach with primary closure of the defect and extraperitoneal sublay mesh, whenever possible. Prevention is key. To help reduce risk of hernia, we recommend closure of all muscle layers with slowly absorbable suture; this is different than was originally described in the spine literature.




Similar content being viewed by others
References
Brau SA (2002) Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results and complications. Spine J 2(3):216–223
Mobbs R, Phan K, Daly D, Rao PJ, Lennox A (2016) Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Global Spine J 6(2):147–154
Shields DC, Khoo LT, Goldberg G, Vaccaro AR (2007) (2007) Anatomical approaches for minimally invasive surgery. In: Vaccaro AR (ed) Minimally Invasive Spine Surgery. Informa Healthcare, New York, NY, pp 1–11
Ozgur B, Aryan H, Pimenta L, Taylor W (2006) Extreme Lateral Interbody Fusion (LIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6(4):435–443
Rodgers W, Gerber E, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine 36(1):26–32
Isaacs R, Hyde J, Goodrich J, Rodgers W, Phillips F (2010) A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. Spine. https://doi.org/10.1097/BRS.0b013e3182022e04
Sofianos D, Briseno M, Abrams J, Patel A (2010) Complications of the lateral transpsoas approach for lumbar interbody arthrodesis: a case series and literature review. Clin Orthop Relat Res 470(6):1621–1632
Cahill KS, Martinez JL, Wang MY, Vanni S, Levi AD (2012) Motor nerve injuries following the minimally invasive lateral transpsoas approach. J of Neurosurg Spine 17(3):227–231
Galan T, Mohan V, Klineberg E, Gupta M, Roberto R, Ellwitz J (2012) Case report: incisional hernia as a complication of extreme lateral interbody fusion. Spine J 12(4):e1–e6
Gundanna M, Shah K (2018) Delayed incisional hernia following minimally invasive trans-psoas lumbar spine surgery: report of a rare complication and management. Int J Spine Surg 12(2):126–130
Caputo AM, Michael KW, Chapman TM, Jennings JM, Hubbard EW, Isaacs RE, Brown CR (2013) Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci 20(11):1558–1563
Vivas AC, Januszewski J, Hajirawala L, Paluzzi JM, Gandhi SV, Uribe JS (2018) Incisional hernia after minimally invasive lateral retroperitoneal surgery: case series and review of the literature. Operative Neurosurg 16(3):368–373
Castle-Kirszbaum M, Goldschlager T (2019) Letter: incisional hernia after minimally invasive lateral retroperitoneal surgery: case series and review of the literature. Operative Neurosurg 17(4):E188
Edwards C, Geiger T, Bartow K, Ramaswamy A, Fearing N, Thaler K, Ramshaw B (2009) Laparoscopic transperitoneal repair of flank hernias: a retrospective review of 27 patients. Surg Endosc. https://doi.org/10.1007/s00464-009-0477-4
Rodgers W, Gerber E, Patterson J (2010) Fusion after minimally disruptive anterior lumbar interbody fusion: analysis of extreme lateral interbody fusion by computed tomography. SAS J 4(2):63–66
Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M, Kercher KW, Lammers BJ, Parra-Davilla E, Roll S, Towfigh S, van Geffen E, Conze J, van Goor H (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18(1):7–17
Shekarriz B, Graziottin TM, Gholami S, Lu H, Yamada H, Duh Q, Stoller ML (2001) Transperitoneal Preperitoneal Laparoscopic Lumbar Incisional Herniorraphy. J Urol 166(4):1267–1269
Moreno-Egea A, Torralba-Martinez JA, Morales G, Fernandez T, Girela E, Aguayo-Albasini JL (2005) Open vs laparoscopic repair of secondary lumbar hernias: a prospective nonrandomized study. Surg Endoscopy Other Interventional Tech 19(2):184–187
Hesselink VJ, Luijendijk RW, DeWilt JH, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Gecim I, Kocak S, Ersoz S, Bumin C, Aribal D (1996) Recurrence after incisional hernia repair: results and risk factors. Surg Today 26(8):607–609
Israelsson LA, Jonsson T (1997) Overweight and healing of midline incisions: the importance of suture technique. Eur J Surgery 163(3):175–180
Sørensen LT, Hemmingsen UB, Kirkeby LT, Kallehave F, Jørgensen LN. Smoking is a risk factor for incisional hernia. Arch Surg 140(2):119–123
Sugerman HJ, Kellum JM Jr, Reines DH, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171(1):80–84
Sorenson LT (2012) Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg 255(6):1069–1079
Hsiao W, Young K, Wang S, Lin P (2000) Incisional hernia after laparotomy: prospective randomized comparison between early-absorbable and late-absorbable suture materials. World J Surg 24(6):747–752
Luijendijk RW (2000) Incisional Hernia: Risk Factors, Prevention, and Repair. Johnson & Johnson Medical B.V, (Netherlands)
Riet M, Steyerberg E, Nellensteyn J, Bonjer H, Jeekel J (2002) Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg 89(11):1350–1356
O’dwyer PJ, Courtney C. (2003) Factors Involved in Abdominal Wall Closure and Subsequent Incisional Hernia. Surgeon 1(1):17–22
Wissing J, van Vroonhoven JM, Schattenkerk ME, Veen HF, Ponsen R, Jeekel J (1987) Fascia closure after midline laparotomy: results of a randomized trial. Br J Surg 74(8):738–741
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Shirin Towfigh, Erfan Zarrinkhoo, Khadij Assani, Ms. Isabel Capati, and Ms. Negin Fadaee declare that they have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fadaee, N., Zarrinkhoo, E., Assani, K. et al. Flank incisional hernia after lateral approach spine operations: presentation and outcomes after repair. Surg Endosc 36, 2138–2145 (2022). https://doi.org/10.1007/s00464-021-08450-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08450-w