Abstract
Background
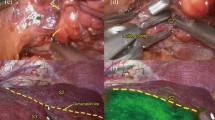
Laparoscopic right posterior hepatectomy is considered difficult on the basis of the surgery difficulty scoring system. In this study, we evaluated the safety and effectiveness of the technical application of indocyanine green (ICG) fluorescence imaging-guided laparoscopic right posterior hepatectomy.
Methods
Twenty-six patients who underwent ICG fluorescence imaging-guided laparoscopic right posterior hepatectomy at Hepatobiliary and Pancreatic Surgery Department of Zhongnan Hospital, Wuhan University, from June 2018 to December 2019, were included. The influence of patient position, trocar placement, hepatic inflow occlusion, central venous pressure (CVP), and the ICG fluorescence imaging-guided method were analyzed.
Results
In 17 patients, the left lateral position was maintained when the main tumor was in the S7, and in the remaining nine patients, the supine position was maintained with the right side of the body raised when the main tumor was in the S6. Ten patients who underwent preoperative injection of ICG were successfully developed for nonanatomical hepatectomy. Sixteen patients received intraoperative ICG injection for anatomical hepatectomy (2 cases had positive imaging findings, 14 cases had negative imaging findings, and 2 cases had failed imaging findings). All patients underwent the Pringle maneuver during the procedure. Four patients were preset with subhepatic vena cava blocking and one patient with suprahepatic inferior vena cava blocking. CVP was controlled at 3.00 ± 0.63 (mean ± SD) cmH2O. The operative time was 216.14 ± 52.05 min, and the bleeding volume was 128.57 ± 75.55 ml. Four patients had Clavien–Dindo level I complications, and one had level III complications. Postoperative hospitalization duration was 6.19 ± 1.40 days. There were 14 patients with hepatocellular carcinoma, 9 with metastatic liver malignancies, 2 with hepatic hemangioma, 1 with focal nodular hyperplasia of the liver, and 10 with hepatitis B liver cirrhosis.
Conclusions
ICG fluorescence imaging guidance could be helpful for the safe implementation of laparoscopic right posterior hepatectomy.






Similar content being viewed by others
References
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267:13–17
Tarantino G, Magistri P, Serra V, Berardi G, Assirati G, Ballarin R, Di Benedetto F (2017) Laparoscopic liver resection of right posterior segments for hepatocellular carcinoma on cirrhosis. J Laparoendosc Adv Surg Tech A 27:559–563
Ishizawa T, Saiura A, Kokudo N (2016) Clinical application of indocyanine green-fluorescence imaging during hepatectomy. Hepatobiliary Surg Nutr 5:322–328
Nakaseko Y, Ishizawa T, Saiura A (2018) Fluorescence-guided surgery for liver tumors. J Surg Oncol 118:324–331
Watanabe J, Ishibe A, Suwa Y, Suwa H, Ozawa M, Momiyama M, Ota M, Endo I (2018) Real-time indocyanine green fluorescence imaging-guided laparoscopic right hemicolectomy in hepatic flexural colon cancer. Dis Colon Rectum 61:1333–1334
Majlesara A, Golriz M, Hafezi M, Saffari A, Stenau E, Maier-Hein L, Muller-Stich BP, Mehrabi A (2017) Indocyanine green fluorescence imaging in hepatobiliary surgery. Photodiagn Photodyn Ther 17:208–215
D’Hondt M, Ovaere S, Knol J, Vandeputte M, Parmentier I, De Meyere C, Vansteenkiste F, Besselink M, Pottel H, Verslype C (2019) Laparoscopic right posterior sectionectomy: single-center experience and technical aspects. Langenbecks Arch Surg 404:21–29
Jin H, Yin Z, Zhou Y, Ma T, Jian Z (2018) Safety and feasibility of a laparoscopy-assisted non-anatomic resection technique for hepatocellular carcinoma located at right posterior segments in cirrhotic patients: a case-controlled study with propensity score matching. Dig Surg 35:411–418
Kim JM, Kwon CH, Joh JW, Na BG, Lee KW, Choi GS, Lee JH (2016) Nonanatomical resection is comparable with anatomical resection in solitary hepatocellular carcinoma <5 cm in the right posterior section. Medicine 95:e5382
Morise Z (2016) Laparoscopic liver resection for posterosuperior tumors using caudal approach and postural changes: a new technical approach. World J Gastroenterol 22:10267–10274
Yip VS, Poon RT, Chok KS, Chan AC, Dai WC, Tsang SH, Chan SC, Lo CM, Cheung TT (2015) Comparison of survival outcomes between right posterior sectionectomy and right hepatectomy for hepatocellular carcinoma in cirrhotic liver: a single-centre experience. World J Surg 39:2764–2770
Zhong FP, Zhang YJ, Liu Y, Zou SB (2017) Prognostic impact of surgical margin in patients with hepatocellular carcinoma: a meta-analysis. Medicine 96:e8043
Siddiqi NN, Abuawwad M, Halls M, Rawashdeh A, Giovinazzo F, Aljaiuossi A, Wicherts D, D’Hondt M, Hilal MA (2018) Laparoscopic right posterior sectionectomy (LRPS): surgical techniques and clinical outcomes. Surg Endosc 32:2525–2532
Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ (2015) Central venous pressure and liver resection: a systematic review and meta-analysis. HPB 17:863–871
Schwarz C, Plass I, Fitschek F, Punzengruber A, Mittlbock M, Kampf S, Asenbaum U, Starlinger P, Stremitzer S, Bodingbauer M, Kaczirek K (2019) The value of indocyanine green clearance assessment to predict postoperative liver dysfunction in patients undergoing liver resection. Sci Rep 9:8421
Wang YY, Zhao XH, Ma L, Ye JZ, Wu FX, Tang J, You XM, Xiang BD, Li LQ (2018) Comparison of the ability of Child-Pugh score, MELD score, and ICG-R15 to assess preoperative hepatic functional reserve in patients with hepatocellular carcinoma. J Surg Oncol 118:440–445
Kokudo T, Hasegawa K, Shirata C, Tanimoto M, Ishizawa T, Kaneko J, Akamatsu N, Arita J, Demartines N, Uldry E, Kokudo N, Halkic N (2019) Assessment of preoperative liver function for surgical decision making in patients with hepatocellular carcinoma. Liver Cancer 8:447–456
Motono N, Iwai S, Funasaki A, Sekimura A, Usuda K, Uramoto H (2019) Low-dose indocyanine green fluorescence-navigated segmentectomy: prospective analysis of 20 cases and review of previous reports. J Thorac Dis 11:702–707
Boogerd LSF, Handgraaf HJM, Huurman VAL, Lam HD, Mieog JSD, van der Made WJ, van de Velde CJH, Vahrmeijer AL (2017) The best approach for laparoscopic fluorescence cholangiography: overview of the literature and optimization of dose and dosing time. Surg Innov 24:386–396
Aoki T, Murakami M, Koizumi T, Matsuda K, Fujimori A, Kusano T, Enami Y, Goto S, Watanabe M, Otsuka K (2018) Determination of the surgical margin in laparoscopic liver resections using infrared indocyanine green fluorescence. Langenbecks Arch Surg 403:671–680
Rhu J, Kim SJ, Choi GS, Kim JM, Joh JW, Kwon CHD (2018) Laparoscopic versus open right posterior sectionectomy for hepatocellular carcinoma in a high-volume center: a propensity score matched analysis. World J Surg 42:2930–2937
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21:745–753
Shilal P, Tuli A (2015) Anatomical variations in the pattern of the right hepatic veins draining the posterior segment of the right lobe of the liver. J Clin Diagn Res 9:AC08-12
Lin CX, Guo Y, Lau WY, Zhang GY, Huang YT, He WZ, Lai EC (2013) Optimal central venous pressure during partial hepatectomy for hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int 12:520–524
Guan X, Nguyen MT, Walsh TM, Kelly B (2016) Robotic single-site endometriosis resection using firefly technology. J Minim Invasive Gynecol 23:10–11
Yu HW, Chung JW, Yi JW, Song RY, Lee JH, Kwon H, Kim SJ, Chai YJ, Choi JY, Lee KE (2017) Intraoperative localization of the parathyroid glands with indocyanine green and Firefly(R) technology during BABA robotic thyroidectomy. Surg Endosc 31:3020–3027
Acknowledgements
The manuscript was written by all the authors. All authors have given approval for the final version of the manuscript. Li Jinghua and Li Xiaomian contributed to the manuscript equally. This work was supported by the grants from the National Key R&D Program of China (SQ2019YFC200078/02), the Scientific Research Project of the Health Commission of Hubei Province (WJ2017Z007), and the special fund for Basic Scientific Research of Wuhan University (2042019kf0327).
Funding
This work was supported by the Grants from the National Key R&D Program of China (SQ2019YFC200078/02), the Scientific Research Project of the Health Commission of Hubei Province (WJ2017Z007), and the special fund for Basic Scientific Research of Wuhan University (2042019kf0327).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jinghua Li, Xiaomian Li, Xiao Zhang, Haitao Wang, Kun Li, Yueming He, Zhisu Liu, Zhonglin Zhang, and Yufeng Yuan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Li, X., Zhang, X. et al. Indocyanine green fluorescence imaging-guided laparoscopic right posterior hepatectomy. Surg Endosc 36, 1293–1301 (2022). https://doi.org/10.1007/s00464-021-08404-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08404-2